Abstract
Study design
Retrospective study.
Objective
To analyze the relationships between three-dimensional (3D) measurements of spinal deformity and Scoliosis Research Society-22 (SRS-22) scores in preoperative patients with major thoracic adolescent idiopathic scoliosis (AIS).
Summary and background data
Previous studies reported 2D measurements were not or only weakly correlated with preoperative SRS-22 scores. However, 2D measures do not always accurately represent the 3D deformity.
Methods
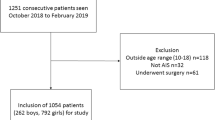
A multicenter prospective registry of surgically treated AIS patients was reviewed for patients with right major thoracic AIS (Lenke type 1–4) who underwent biplanar radiography and completed the SRS-22 questionnaire preoperatively. For the 3D measurements, two reference frames were utilized: global (gravity/patient-based) and local (vertebra/disc-based). To obtain regional measurements, the individual segments in the appropriate reference plane were summed between the levels of interest. Patients were divided into two groups for each SRS-22 domain according to their scores: low (< 4) and high (≥ 4) score groups. Group differences and correlations with SRS-22 scores were analyzed with p < 0.01 as the threshold for significance.
Results
There were 405 eligible patients (mean age, 14.4 years). The mean 3D thoracic curve was 59° (45°–115°). The only significant group difference of 3D measurements occurred in the local lumbar lordosis (LL) with a small mean difference (− 3.4°, p = 0.008) in the mental health domain. In the correlation analyses, global and local thoracic kyphosis (TK) and TK/LL ratio demonstrated significant, but weak, correlations with function and total scores (|r|< 0.2, p < 0.01).
Conclusion
3D measurements of scoliosis severity have only weak associations with preoperative SRS-22 scores, which might indicate a limit to the discriminative capacity of the SRS-22 within surgical range major thoracic AIS curves. Interestingly, the sagittal plane was the principle 3D plane in which significant correlations existed.
Level of evidence
II, prognostic.


Similar content being viewed by others
References
Weinstein SL, Dolan LA, Spratt KF et al (2003) Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA 289:559–567
Weinstein SL, Zavala DC, Ponseti IV (1981) Idiopathic scoliosis: long-term follow-up and prognosis in untreated patients. J Bone Jt Surg Am 63:702–712
Tones M, Moss N, Polly DW Jr (2006) A review of quality of life and psychosocial issues in scoliosis. Spine (Phila Pa 1976) 31:3027–3038
Asher M, Min Lai S, Burton D et al (2003) Discrimination validity of the Scoliosis Research Society-22 patient questionnaire: relationship to idiopathic scoliosis curve pattern and curve size. Spine (Phila Pa 1976) 28:74–78
Verma K, Lonner B, Hoashi JS et al (2010) Demographic factors affect Scoliosis Research Society-22 performance in healthy adolescents: a comparative baseline for adolescents with idiopathic scoliosis. Spine (Phila Pa 1976) 35:2134–2139
Haher TR, Gorup JM, Shin TM et al (1999) Results of the Scoliosis Research Society instrument for evaluation of surgical outcome in adolescent idiopathic scoliosis. A multicenter study of 244 patients. Spine (Phila Pa 1976) 24:1435–1440
Bastrom TP, Bartley C, Marks MC et al (2015) Postoperative perfection: ceiling effects and lack of discrimination with both SRS-22 and -24 outcomes instruments in patients with adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 40:E1323–E1329
Berliner JL, Verma K, Lonner BS et al (2013) Discriminative validity of the Scoliosis Research Society 22 questionnaire among five curve-severity subgroups of adolescents with idiopathic scoliosis. Spine J 13:127–133
Parent EC, Hill D, Mahood J et al (2009) Discriminative and predictive validity of the Scoliosis Research Society-22 questionnaire in management and curve-severity subgroups of adolescents with idiopathic scoliosis. Spine (Phila Pa 1976) 34:2450–2457
Rainoldi L, Zaina F, Villafane JH et al (2015) Quality of life in normal and idiopathic scoliosis adolescents before diagnosis: reference values and discriminative validity of the SRS-22. A cross-sectional study of 1,205 pupils. Spine J 15:662–667
Asher M, Lai SM, Burton D et al (2004) The influence of spine and trunk deformity on preoperative idiopathic scoliosis patients' health-related quality of life questionnaire responses. Spine (Phila Pa 1976) 29:861–868
Brewer P, Berryman F, Baker D et al (2013) Influence of Cobb Angle and ISIS2 surface topography volumetric asymmetry on Scoliosis Research Society-22 outcome scores in scoliosis. Spine Deform 1:452–457
Wang L, Wang YP, Yu B et al (2014) Relation between self-image score of SRS-22 with deformity measures in female adolescent idiopathic scoliosis patients. Orthop Traumatol Surg Res 100:797–801
Djurasovic M, Glassman SD, Sucato DJ et al (2018) Improvement in Scoliosis Research Society-22R pain scores after surgery for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 43:127–132
Ward WT, Friel NA, Kenkre TS et al (2017) SRS-22r scores in nonoperated adolescent idiopathic scoliosis patients with curves greater than forty degrees. Spine (Phila Pa 1976) 42:1233–1240
Hayashi K, Upasani VV, Pawelek JB et al (2009) Three-dimensional analysis of thoracic apical sagittal alignment in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 34:792–797
Glaser DA, Doan J, Newton PO (2012) Comparison of 3-dimensional spinal reconstruction accuracy: biplanar radiographs with EOS versus computed tomography. Spine (Phila Pa 1976) 37:1391–1397
Newton PO, Fujimori T, Doan J et al (2015) Defining the "three-dimensional sagittal plane" in thoracic adolescent idiopathic scoliosis. J Bone Jt Surg Am 97:1694–1701
Stokes IA (1994) Three-dimensional terminology of spinal deformity. A report presented to the Scoliosis Research Society by the Scoliosis Research Society working group on 3-D terminology of spinal deformity. Spine (Phila Pa 1976) 19:236–248
Sangole A, Aubin CE, Labelle H et al (2010) The central hip vertical axis: a reference axis for the Scoliosis Research Society three-dimensional classification of idiopathic scoliosis. Spine (Phila Pa 1976) 35:E530–E534
Bago J, Perez-Grueso FJ, Les E et al (2009) Minimal important differences of the SRS-22 Patient Questionnaire following surgical treatment of idiopathic scoliosis. Eur Spine J 18:1898–1904
Carreon LY, Sanders JO, Diab M et al (2010) The minimum clinically important difference in Scoliosis Research Society-22 appearance, activity, and pain domains after surgical correction of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 35:2079–2083
Bagheri A, Liu XC, Tassone C et al (2018) Reliability of three-dimensional spinal modeling of patients with idiopathic scoliosis using EOS system. Spine Deform 6:207–212
Carreau JH, Bastrom T, Petcharaporn M et al (2014) Computer-generated, three-dimensional spine model from biplanar radiographs: a validity study in idiopathic scoliosis curves greater than 50 degrees. Spine Deform 2:81–88
Ilharreborde B, Steffen JS, Nectoux E et al (2011) Angle measurement reproducibility using EOS three-dimensional reconstructions in adolescent idiopathic scoliosis treated by posterior instrumentation. Spine (Phila Pa 1976) 36:E1306–E1313
Glassman SD, Bridwell K, Dimar JR et al (2005) The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 30:2024–2029
Schwab FJ, Blondel B, Bess S et al (2013) Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 38:E803–E812
Zhu F, Chu WC, Sun G et al (2011) Rib length asymmetry in thoracic adolescent idiopathic scoliosis: is it primary or secondary? Eur Spine J 20:254–259
Acknowledgements
Funding to support this study was received from the Rady Children’s Hospital Assaraf Family. Fund and from research grants to Setting Scoliosis Straight Foundation from DePuy Synthes. Spine, EOS imaging, K2M, Medtronic, NuVasive and Zimmer Biomet in support of Harms. Study Group research.
Harms Study Group Investigators: Aaron Buckland, MD; New York University Amer Samdani, MD; Shriners Hospitals for Children—Philadelphia, Amit Jain, MD; Johns Hopkins Hospital, Baron Lonner, MD; Mount Sinai Hospital, Benjamin Roye, MD; Columbia University, Burt Yaszay, MD; Rady Children’s Hospital, Chris Reilly, MD; BC Children’s Hospital, Daniel Hedequist, MD; Boston Children’s Hospital, Daniel Sucato, MD; Texas Scottish Rite Hospital, David Clements, MD; Cooper Bone & Joint Institute New Jersey. Title Page: Firoz Miyanji, MD; BC Children’s Hospital, Harry Shufflebarger, MD; Nicklaus Children's Hospital, Jack Flynn, MD; Children’s Hospital of Philadelphia, Jahangir Asghar, MD; Cantor Spine Institute, Jean Marc Mac Thiong, MD; CHU Sainte-Justine, Joshua Pahys, MD; Shriners Hospitals for Children—Philadelphia, Juergen Harms, MD; Klinikum Karlsbad-Langensteinbach, Karlsbad, Keith Bachmann, MD; University of Virginia, Larry Lenke, MD; Columbia University, Mark Abel, MD; University of Virginia, Michael Glotzbecker, MD; Boston Children’s Hospital, Michael Kelly, MD; Washington University, Michael Vitale, MD; Columbia University, Michelle Marks, PT, MA; Setting Scoliosis Straight Foundation, Munish Gupta, MD; Washington University, Nicholas Fletcher, MD; Emory University, Patrick Cahill, MD; Children’s Hospital of Philadelphia, Paul Sponseller, MD; Johns Hopkins Hospital, Peter Gabos, MD: Nemours/Alfred I. duPont Hospital for Children, Peter Newton, MD; Rady Children’s Hospital, Peter Sturm, MD; Cincinnati Children’s Hospital, Randal Betz, MD; Institute for Spine & Scoliosis, Ron Lehman, MD; Columbia University, Stefan Parent, MD: CHU Sainte-Justine, Stephen George, MD; Nicklaus Children's Hospital, Steven Hwang, MD; Shriners Hospitals for Children—Philadelphia, Suken Shah, MD; Nemours/Alfred I. duPont Hospital for Children, Tom Errico, MD; Nicklaus Children's Hospital, Vidyadhar Upasani, MD; Rady Children’s Hospital.
Funding
Funding was provided by Setting Scoliosis Straight Foundation.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Ethical approval
IRB approval was obtained for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ohashi, M., Bastrom, T.P., Bartley, C.E. et al. Associations between three-dimensional measurements of the spinal deformity and preoperative SRS-22 scores in patients undergoing surgery for major thoracic adolescent idiopathic scoliosis. Spine Deform 8, 1253–1260 (2020). https://doi.org/10.1007/s43390-020-00150-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00150-0