Abstract
Study design
Cross-sectional comparative study.
Objectives
Evaluate prevalence and clinical relevance of an underlying pathology in painful adolescent idiopathic scoliosis (AIS) patients after a non-diagnostic history, physical examination and spinal X-ray using Magnetic Resonance Image (MRI) as diagnostic tool.
Summary of background data
Discrepancies regarding indications of routine MRI screening in painful AIS patients are multifactorial. Few studies have investigated relationship and practical importance of painful AIS with an underlying pathology by MRI.
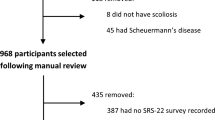
Method
A total of 152-consecutive AIS patients complaining of back pain during a 36-month period were enrolled. All patients underwent whole-spine MRI after a non-diagnostic history, physical examination and spinal X-ray. Underlying pathologies were reported as neural and non-neural axis abnormalities based on MRI reports. Variables such as sex, age, constant or intermittent pain, night pain, back pain location (thoracic or lumbar pain), Cobb-angle and follow-up were evaluated as clinical markers to predict presence of underlying MRI pathologies.
Results
The presence of an underlying pathology was found by MRI in 54 painful AIS patients (35.5%). Isolated syringomyelia was the only neural axis abnormality found in 6 patients (3.9%). Non-neural axis abnormalities (31.6%) were composed by: 32 herniated nucleus pulposus, 5 vertebral disc desiccation, 4 ovarian cysts, 3 renal cysts, 2 sacral cysts, and 2 vertebral hemangiomas. There was no association with gender, age of presentation, initial coronal Cobb angle and follow up; with presence of an underlying pathology. Lumbar pain location was identified as an adequate clinical marker that correlated with presence of an underlying pathology (p = 0.01).
Conclusions
Prevalence of underlying pathologies diagnosed by MRI in painful AIS was found high (35.5%), but it’s clinical relevance and implication are debatable. The use of MRI did not affect orthopedic management of painful AIS patients who showed an underlying pathology. A thorough evaluation must be performed by clinicians; and discussed with patients and family prior to undergo further imaging management.
Level of evidence
Level III.
Similar content being viewed by others
References
Singhal R, Perry DC, Prasad S, Davidson NT, Bruce CE (2013) The use of routine preoperative magnetic resonance imaging in identifying intraspinal anomalies in patients with idiopathic scoliosis: a 10-year review. Eur Spine J 22(2):355–359. https://doi.org/10.1007/s00586-012-2538-y(Epub 2012 Oct 13)
Lee CS, Hwang CJ, Kim NH, Noh HM, Lee MY, Yoon SJ, Lee DH (2017) Preoperative magnetic resonance imaging evaluation in patients with adolescent idiopathic scoliosis. Asian Spine J. 11(1):37–43. https://doi.org/10.4184/asj.2017.11.1.37(Epub 2017 Feb 17)
Nakahara D, Yonezawa Kobanawa K, Sakoda J, Nojiri H, Kamano S, Okuda T, Kurosawa H (2011) Magnetic resonance imaging evaluation of patients with idiopathic scoliosis: a prospective study of four hundred seventy-two outpatients. Spine (Phila Pa 1976) 36(7):E482–E485. https://doi.org/10.1097/brs.0b013e3181e029ed
Diab M, Landman Z, Lubicky J, Dormans J, Erickson M, Richards BS, members of the Spinal Deformity (2011) Use and outcome of MRI in the surgical treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 36(8):667–671. https://doi.org/10.1097/brs.0b013e3181da218c
Davids JR, Chamberlin E, Blackhurst DW (2004) Indications for magnetic resonance imaging in presumed adolescent idiopathic scoliosis. J Bone Joint Surg Am 86:2187–2195
Swarup I, Silberman J, Blanco J, Widmann R (2019) Incidence of intraspinal and extraspinal MRI abnormalities in patients with adolescent idiopathic scoliosis. Spine Deform. 7(1):47–52. https://doi.org/10.1016/j.jspd.2018.06.006
Samuelsson L, Lindell D, Kogler H (1991) Spinal cord and brain stem anomalies in scoliosis. MR screening of 26 cases. Acta Orthop Scand. 62(5):403–406
Maiocco B, Deeney VF, Coulon R, Parks PF Jr (1997) Adolescent idiopathic scoliosis and the presence of spinal cord abnormalities. Preoperative magnetic resonance imaging analysis. Spine (Phila Pa 1976) 22(21):2537–2541
Do T, Fras C, Burke S, Widmann RF, Rawlins B, Boachie-Adjei O (2001) Clinical value of routine preoperative magnetic resonance imaging in adolescent idiopathic scoliosis. A prospective study of three hundred and twenty-seven patients. J Bone Joint Surg Am. 83(4):577–579
Qiao J, Zhu Z, Zhu F et al (2013) Indication for preoperative MRI of neural axis abnormalities in patients with presumed thoracolumbar/lumbar idiopathic scoliosis. Eur Spine J 22:360e
Khanna G (2009) Role of imaging in scoliosis. Pediatr Radiol 39(Suppl 2):S247–S251. https://doi.org/10.1007/s00247-008-1126-0
Benli IT, Uzümcügil O, Aydin E, Ateş B, Gürses L, Hekimoğlu B (2006) Magnetic resonance imaging abnormalities of neural axis in Lenke type 1 idiopathic scoliosis. Spine (Phila Pa 1976) 31(16):1828–1833
Jones JY, Saigal G, Palasis S et al (2019) ACR appropriateness criteria® scoliosis-child. J Am Coll Radiol. 16(5S):S244–S251. https://doi.org/10.1016/j.jacr.2019.02.018
Taylor LJ (1986) Painful scoliosis: a need for further investigation. Br Med J (Clin Res Ed) 292(6513):120–122. https://doi.org/10.1136/bmj.292.6513.120
Fraser RD, Paterson DC, Simpson DA (1977) Orthopaedic aspects of spinal tumors in children. J Bone Joint Surg Br 59(2):143–151
Rand RW, Rand CW (1960) Intraspinal tumors of childhood. Thomas: Springfield, Ill, p xi
Citron N, Edgar MA, Sheehy J, Thomas DGT (1984) Intramedullary spinal cord tumors presenting as scoliosis. J Bone Joint Surg Br 66(4):513–517
Schwend RM, Hennrikus W, Hall JE, Emans JB (1995) Childhood scoliosis: clinical indications for magnetic resonance imaging. J Bone Joint Surg Am 77(1):46–53
Barnes PD, Brody JD, Jaramillo D, Akbar JU, Emans JB (1993) Atypical idiopathic scoliosis: MR imaging evaluation. Radiology 186(1):247–253
Morcuende JA, Dolan LA, Vazquez JD, Jirasirakul A, Weinstein SL (2004) A prognostic model for the presence of neurogenic lesions in atypical idiopathic scoliosis. Spine (Phila Pa 1976) 29:51–58
Ramirez N, Johnston CE, Browne RH (1997) The prevalence of back pain in children who have idiopathic scoliosis. J Bone Joint Surg Am 79(3):364–368
Feldman DS, Straight JJ, Badra MI et al (2006) Evaluation of an algorithmic approach to pediatric back pain. J Pediatr Orthop 26:353–357
Feldman DS, Hedden DM, Wright JG (2000) The use of bone scan to investigate back pain in children and adolescents. J Pediatr Orthop 20:790–795
Ramirez N, Flynn JM, Hill BW et al (2015) Evaluation of a systematic approach to pediatric back pain: the utility of magnetic resonance imaging. J Pediatr Orthop 35(1):28–32. https://doi.org/10.1097/BPO.0000000000000190
Fekete TF, Mannion AF, Haschtmann D, Loibl M, Kleinstück FS, Jeszenszky DJ (2019) Back pain and its change after surgery in adolescents and young adults with idiopathic scoliosis. Spine Deform. 7(5):754–758. https://doi.org/10.1016/j.jspd.2019.02.004
Sato T, Hirano T, Ito T et al (2011) Back pain in adolescents with idiopathic scoliosis: epidemiological study for 43,630 pupils in Niigata City, Japan. Eur Spine J. 20(2):274–279. https://doi.org/10.1007/s00586-010-1657-6(Epub 2010 Dec 17)
Balagué F, Pellisé F (2016) Adolescent idiopathic scoliosis and back pain. Scoliosis Spinal Disord. 11(1):27. https://doi.org/10.1186/s13013-016-0086-7
Wong AYL, Samartzis D, Cheung PWH, Yin Cheung JP (2019) How common is back pain and what biopsychosocial factors are associated with back pain in patients with adolescent idiopathic scoliosis? Clin Orthop Relat Res 477(4):676–686. https://doi.org/10.1097/CORR.0000000000000569
Calloni SF, Huisman TA, Poretti A, Soares BP (2017) Back pain and scoliosis in children: when to image, what to consider. Neuroradiol J. 30(5):393–404. https://doi.org/10.1177/1971400917697503(Epub 2017 Mar 20)
Altaf F, Heran MKS, Wilson LF (2014) Back pain in children and adolescents. Bone Joint J 96-B:717–723
Janicki JA, Alman B (2007) Scoliosis: review of diagnosis and treatment. Paediatr Child Health. 12(9):771–776
Rajasekaran S, Kamath V, Kiran R, Shetty AP (2010) Intraspinal anomalies in scoliosis: an MRI analysis of 177 consecutive scoliosis patients. Indian J Orthop. 44(1):57–63. https://doi.org/10.4103/0019-5413.58607
Funding
This study did not receive any type of funding sources.
Author information
Authors and Affiliations
Contributions
NR, GO, AC, LC, NR and II: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. NR, GO, AC, LC, NR and II: Drafting the work or revising it critically for important intellectual content. NR, GO, AC, LC, NR and II: Final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Ramírez, Dr. Olivella, Dr. Cuneo, Dr. Carrazana, Mrs. Ramírez & Dr. Iriarte declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board committee of Ponce Research Institute (Protocol # 150320-NR) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ramírez, N., Olivella, G., Cuneo, A. et al. Prevalence and clinical relevance of underlying pathological conditions in painful adolescent idiopathic scoliosis: a MRI-based study. Spine Deform 8, 663–668 (2020). https://doi.org/10.1007/s43390-020-00065-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00065-w