Abstract
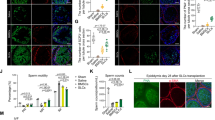
Diabetes is known to negatively affect male reproduction. Recent clinical results have confirmed that mesenchymal stem cell (MSC)–based therapies are safe and effective for the treatment of diabetes. However, the effect and potential mechanism through which MSC transplantation improves diabetes-derived male reproductive dysfunction are still unknown. In the present study, we first established a male T1D mouse model through intraperitoneal injection of streptozotocin for five consecutive days. Subsequently, we evaluated the blood glucose levels, fertility, and histology and immunology of the pancreas, testes, and penis of T1D mice with or without transplantation of menstrual blood–derived endometrial stem cells (MenSCs) or umbilical cord mesenchymal stem cells (UCMSCs). Glucose was added to the medium in which the Leydig cells were cultured to imitate high glucose–injured cell viability. Subsequently, we evaluated the cellular viability, ROS levels, and mitochondrial membrane potential of Leydig cells treated with or without MenSC-conditioned medium (MenSC-CM) using a CCK8 assay, immunofluorescence, and flow cytometry. The targeted proteins are involved in the potential mechanism underlying MenSC-derived improvements, which was further validated via Western blotting. Collectively, our results indicated that MenSC transplantation significantly ameliorated reproductive dysfunction in male T1D mice by enhancing cellular antioxidative capacity and promoting angiogenesis. This study provides solid evidence and support for the application of MSCs to improve diabetes-induced male reproductive dysfunction.





Similar content being viewed by others
Data Availability
The raw data of the study can be obtained from the corresponding author without reservation.
References
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2012;35(Suppl 1):S64–71.
Ma RC, Chan JC. Type 2 diabetes in East Asians: similarities and differences with populations in Europe and the United States. Ann N Y Acad Sci. 2013;1281(1):64–91.
La Vignera S, Condorelli RA, Di Mauro M, et al. Reproductive function in male patients with type 1 diabetes mellitus. Andrology. 2015;3(6):1082–7.
La Vignera S, Calogero AE, Condorelli R, Lanzafame F, Giammusso B, Vicari E. Andrological characterization of the patient with diabetes mellitus. Minerva Endocrinol. 2009;34(1):1–9.
Kouidrat Y, Pizzol D, Cosco T, et al. High prevalence of erectile dysfunction in diabetes: a systematic review and meta-analysis of 145 studies. Diabet Med. 2017;34(9):1185–92.
Agbaje IM, Rogers DA, McVicar CM, et al. Insulin dependant diabetes mellitus: implications for male reproductive function. Hum Reprod. 2007;22(7):1871–7.
Amaral S, Oliveira PJ, Ramalho-Santos J. Diabetes and the impairment of reproductive function: possible role of mitochondria and reactive oxygen species. Curr Diabetes Rev. 2008;4(1):46–54.
Mallidis C, Agbaje IM, Rogers DA, et al. Advanced glycation end products accumulate in the reproductive tract of men with diabetes. Int J Androl. 2009;32(4):295–305.
Karimi J, Goodarzi MT, Tavilani H, Khodadadi I, Amiri I. Relationship between advanced glycation end products and increased lipid peroxidation in semen of diabetic men. Diabetes Res Clin Pract. 2011;91(1):61–6.
Malavige LS, Levy JC. Erectile dysfunction in diabetes mellitus. J Sex Med. 2009;6(5):1232–47.
Yim MB, Yim HS, Lee C, Kang SO, Chock PB. Protein glycation: creation of catalytic sites for free radical generation. Ann N Y Acad Sci. 2001;928:48–53.
Castela A, Gomes P, Domingues VF, et al. Role of oxidative stress-induced systemic and cavernosal molecular alterations in the progression of diabetic erectile dysfunction. J Diabetes. 2015;7(3):393–401.
Zhang Y, Yu J, Kahkoska AR, Wang J, Buse JB, Gu Z. Advances in transdermal insulin delivery. Adv Drug Deliv Rev. 2019;139:51–70.
Shamloul R, Ghanem H. Erectile dysfunction. Lancet. 2013;381(9861):153–65.
Dang LT, Bui AN, Le-Thanh Nguyen C, et al. Intravenous infusion of human adipose tissue-derived mesenchymal stem cells to treat type 1 diabetic mellitus in mice: an evaluation of grafted cell doses. Adv Exp Med Biol. 2018;1083:145–56.
Sharifian P, Yari S, Hasanein P, Manteghi NY. Conditioned medium of bone marrow mesenchymal stem cells improves sperm parameters and reduces histological alteration in rat testicular ischaemia/reperfusion model. Andrologia. 2022;54(11): e14624.
Nayernia K, Lee JH, Drusenheimer N, et al. Derivation of male germ cells from bone marrow stem cells. Lab Invest. 2006;86(7):654–63.
Zang L, Li Y, Hao H, et al. Efficacy and safety of umbilical cord-derived mesenchymal stem cells in Chinese adults with type 2 diabetes: a single-center, double-blinded, randomized, placebo-controlled phase II trial. Stem Cell Res Ther. 2022;13(1):180.
Hu J, Wang Y, Gong H, et al. Long term effect and safety of Wharton’s jelly-derived mesenchymal stem cells on type 2 diabetes. Exp Ther Med. 2016;12(3):1857–66.
Liu Y, Niu R, Yang F, et al. Biological characteristics of human menstrual blood-derived endometrial stem cells. J Cell Mol Med. 2018;22(3):1627–39.
Liu Y, Niu R, Li W, et al. Therapeutic potential of menstrual blood-derived endometrial stem cells in cardiac diseases. Cell Mol Life Sci. 2019;76(9):1681–95.
Zhang S, Zhang R, Yin X, et al. MenSCs transplantation improve the viability of injured endometrial cells through activating PI3K/Akt pathway. Reprod Sci. 2023;30(11):3325–38.
Sun SY, Gao Y, Liu GJ, Li YK, Gao W, Ran XW. Efficacy and safety of stem cell therapy for T1DM: an updated systematic review and meta-analysis. J Diabetes Res. 2020;2020:5740923.
Lu J, Shen SM, Ling Q, et al. One repeated transplantation of allogeneic umbilical cord mesenchymal stromal cells in type 1 diabetes: an open parallel controlled clinical study. Stem Cell Res Ther. 2021;12(1):340.
Schlatt S, Ehmcke J. Regulation of spermatogenesis: an evolutionary biologist’s perspective. Semin Cell Dev Biol. 2014;29:2–16.
Mallidis C, Agbaje I, Rogers D, et al. Distribution of the receptor for advanced glycation end products in the human male reproductive tract: prevalence in men with diabetes mellitus. Hum Reprod. 2007;22(8):2169–77.
Zickri MB, Moustafa MH, Fasseh AE, Kamar SS. Antioxidant and antiapoptotic paracrine effects of mesenchymal stem cells on spermatogenic arrest in oligospermia rat model. Ann Anat. 2021;237: 151750.
Li H, Yahaya BH, Ng WH, Yusoff NM, Lin J. Front Mol Neurosci. 2019;12:80.
Brownlee M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes. 2005;54(6):1615–25.
Brownlee M. Biochemistry and molecular cell biology of diabetic complications. Nature. 2001;414(6865):813–20.
Fetterman JL, Holbrook M, Westbrook DG, et al. Mitochondrial DNA damage and vascular function in patients with diabetes mellitus and atherosclerotic cardiovascular disease. Cardiovasc Diabetol. 2016;15:53.
Yaribeygi H, Sathyapalan T, Atkin SL, Sahebkar A. Molecular mechanisms linking oxidative stress and diabetes mellitus. Oxid Med Cell Longev. 2020;2020:8609213.
Kosaric N, Srifa W, Bonham CA, et al. Macrophage subpopulation dynamics shift following intravenous infusion of mesenchymal stromal cells. Mol Ther. 2020;28(9):2007–22.
Kim SW, Zhu GQ, Bae WJ. Mesenchymal stem cells treatment for erectile dysfunction in diabetic rats. Sex Med Rev. 2020;8(1):114–21.
Funding
This project was supported by Henan Province Foundation (No. 22A320043, No. 22A310008, No. LHGJ20200941, and No. LHGJ 20220989) and the Xinxiang Medical University Foundation (No. YJSCX202225Y).
Author information
Authors and Affiliations
Contributions
Y Liu conceived and designed the study; Y Lu, R Liu, X Kang, and S Zhang conducted the experiments; Y Lu and Y Sun analysed the data; and Y Lu, R Liu, and X Kang drafted the manuscript. All the authors read and approved the final manuscript. Y Liu is the guarantor of this study and, as such, had full access to all the data in this work and is responsible for the integrity of the data and the accuracy of the data analysis. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
All methods were carried out in accordance with relevant guidelines and regulations. The Ethics Committee of the Xinxiang Medical University has approved all the experiments. The informed consent was obtained from study participants.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lu, Y., Liu, R., Kang, X. et al. Menstrual Blood–Derived Endometrial Stem Cell Transplantation Improves Male Reproductive Dysfunction in T1D Mice by Enhancing Antioxidative Capacity. Reprod. Sci. (2024). https://doi.org/10.1007/s43032-024-01498-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43032-024-01498-8