Abstract
Preterm premature rupture of membranes (pPROM) poses a significant threat to fetal viability and increases the risk for newborn morbidities. The perinatal period of preterm infants affected by pPROM is often characterized by higher rates of mortality and morbidity, with associated risks of cerebral palsy, developmental delays, compromised immune function, respiratory diseases, and sensory impairments. pPROM is believed to result from a variety of causes, including but not limited to microbially induced infections, stretching of fetal membranes, oxidative stress, inflammatory responses, and age-related changes in the fetal-placental interface. Maternal stress, nutritional deficiencies, and medically induced procedures such as fetoscopy are also considered potential contributing factors to pPROM. This comprehensive review explores the potential etiologies leading to pPROM, delves into the intricate molecular mechanisms through which these etiologies cause membrane ruptures, and provides a concise overview of diagnostic and treatment approaches for pPROM. Based on available therapeutic options, this review proposes and explores the possibilities of utilizing a novel composite hydrogel composed of amniotic membrane particles for repairing ruptured fetal membranes, thereby holding promise for its clinical application.
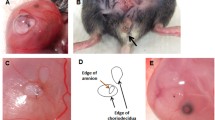
Graphical Abstract






Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Naeye RL, Peters EC. Causes and consequences of premature rupture of fetal membranes. Lancet. 1980;315(8161):192–4.
Mercer BM, Crouse DT, Goldenberg RL, et al. The antibiotic treatment of PPROM study: systemic maternal and fetal markers and perinatal outcomes. Am J Obstet Gynecol. 2012;206(2):145. e1-145. e9.
Musilova I, Andrys C, Drahosova M, et al. Late preterm prelabor rupture of fetal membranes: fetal inflammatory response and neonatal outcome. Pediatr Res. 2018;83(3):630–7.
Caughey AB, Robinson JN, Norwitz ER. Contemporary diagnosis and management of preterm premature rupture of membranes. Rev Obstet Gynecol. 2008;1(1):11.
Swiatkowska-Freund M, Traczyk-Łos A, Partyka A, et al. Perinatal outcome in preterm premature rupture of membranes before 37 weeks of gestation. Ginekol Pol. 2019;90(11):645–50.
Waters TP, Mercer BM. The management of preterm premature rupture of the membranes near the limit of fetal viability. Am J Obstet Gynecol. 2009;201(3):230–40.
Goldenberg RL, Culhane JF, Iams JD, et al. Epidemiology and causes of preterm birth. Lancet. 2008;371(9606):75–84.
Patel RM. Short-and long-term outcomes for extremely preterm infants. Am J Perinatol. 2016;33(03):318–28.
Bhandari A, McGrath-Morrow S. Long-term pulmonary outcomes of patients with bronchopulmonary dysplasia. Semin Perinatol. 2013;37(2):132–7.
Herzlich J, Mangel L, Halperin A, et al. Neonatal outcomes in women with preterm premature rupture of membranes at periviable gestational age. Sci Rep. 2022;12(1):11999.
Manuck TA, Varner MW. Neonatal and early childhood outcomes following early vs later preterm premature rupture of membranes. Am J Obstet Gynecol. 2014;211(3):308. e1-308. e6.
Choi EK, Kim SY, Heo JM, et al. Perinatal outcomes associated with latency in late preterm premature rupture of membranes. Int J Environ Res Public Health. 2021;18(2):672.
Boettcher LB, Clark EAS. Neonatal and childhood outcomes following preterm premature rupture of membranes. Obstet Gynecol Clin North Am. 2020;47(4):671–80.
Soylu H, Jefferies A, Diambomba Y, et al. Rupture of membranes before the age of viability and birth after the age of viability: comparison of outcomes in a matched cohort study. J Perinatol. 2010;30(10):645–9.
Li S, Zhang M, Tian H, et al. Preterm birth and risk of type 1 and type 2 diabetes: systematic review and meta-analysis. Obes Rev. 2014;15(10):804–11.
Kajantie E, Hovi P. Is very preterm birth a risk factor for adult cardiometabolic disease? Semin Fetal Neonatal Med. 2014;19(2):112–211.
Quintero RA, Morales WJ, Kalter CS, et al. Transabdominal intra-amniotic endoscopic assessment of previable premature rupture of membranes. Am J Obstet Gynecol. 1998;179(1):71–6.
Beckmann MW, Wiegratz I, Dereser MM, et al. Diagnostik des Blasensprungs: Vergleich des vaginalen Nachweises von fetalem Fibronectin und der intraamnialen Injektion von Indigo Carmine. Geburtshilfe Frauenheilkd. 1993;53(02):86–91.
Tseng SCG, Espana EM, Kawakita T, et al. How does amniotic membrane work? Ocul Surf. 2004;2(3):177–87.
Hay ED. Extracellular matrix. J Cell Biol. 1981;91(3 Pt 2):205s–23s.
Menon R, Richardson LS. Preterm prelabor rupture of the membranes: a disease of the fetal membranes. Semin Perinatol. 2017;41(7):409–19.
Munoz-Torres JR, Martínez-González SB, Lozano-Luján AD, et al. Biological properties and surgical applications of the human amniotic membrane. Front Bioeng Biotechnol. 2023;10:1067480.
Díaz-Prado S, Muiños-López E, Hermida-Gómez T, et al. Human amniotic membrane as an alternative source of stem cells for regenerative medicine. Differentiation. 2011;81(3):162–71.
Toothaker JM, Presicce P, Cappelletti M, et al. Immune cells in the placental villi contribute to intra-amniotic inflammation. Front Immunol. 2020;11:866.
Llorca T, Ruiz-Magaña MJ, Martinez-Aguilar R, et al. Decidualized human decidual stromal cells inhibit chemotaxis of activated T cells: a potential mechanism of maternal-fetal immune tolerance. Front Immunol. 2023;14:1223539.
Nadeau HCG, Subramaniam A, Andrews WW. Infection and preterm birth. Semin Fetal Neonatal Med. 2016;21(2):100–5.
Chu DM, Seferovic M, Pace RM, et al. The microbiome in preterm birth. Best Pract Res Clin Obstet Gynaecol. 2018;52:103–13.
Marom Y, Gengrinovitch S, Shalev E, et al. Collagen bundling and alignment in equibiaxially stretched human amnion. J Biomech. 2020;108:109896.
Menon R, Boldogh I, Hawkins HK, et al. Histological evidence of oxidative stress and premature senescence in preterm premature rupture of the human fetal membranes recapitulated in vitro. Am J Pathol. 2014;184(6):1740–51.
Dutta EH, Behnia F, Boldogh I, et al. Oxidative stress damage-associated molecular signaling pathways differentiate spontaneous preterm birth and preterm premature rupture of the membranes. Mol Hum Reprod. 2016;22(2):143–57.
Armstrong-Wells J, Donnelly M, Post MD, et al. Inflammatory predictors of neurologic disability after preterm premature rupture of membranes. Am J Obstet Gynecol. 2015;212(2):212. e1-212. e9.
Behnia F, Sheller S, Menon R. Mechanistic differences leading to infectious and sterile inflammation. Am J Reprod Immunol. 2016;75(5):505–18.
Bonney EA, Krebs K, Saade G, et al. Differential senescence in feto-maternal tissues during mouse pregnancy. Placenta. 2016;43:26–34.
Mogami H, Word RA. Healing mechanism of ruptured fetal membrane. Front Physiol. 2020;11:623.
Mercer BM, Lewis R. Preterm labor and preterm premature rupture of the membranes: diagnosis and management. Infect Dis Clin. 1997;11(1):177–201.
Lee KN, Park KH, Ahn K, et al. Extracellular matrix-related and serine protease proteins in the amniotic fluid of women with early preterm labor: association with spontaneous preterm birth, intra-amniotic inflammation, and microbial invasion of the amniotic cavity. Am J Reprod Immunol. 2023;90(1):e13736.
Katzman PJ, Metlay LA. Fetal inflammatory response is often present at early stages of intra-amniotic infection, and its distribution along cord is variable. Pediatr Dev Pathol. 2010;13(4):265–72.
Gondo K, Yamasaki F, Nomiyama M, et al. Relationship of maternal inflammatory response and fetal inflammatory response to duration and intensity of intra-amniotic infection and inflammation. Placenta. 2023;137:23–30.
Yap V, Perlman JM. Mechanisms of brain injury in newborn infants associated with the fetal inflammatory response syndrome. Semin Fetal Neonatal Med. 2020;25(4):101110.
Vrachnis N, Vitoratos N, Iliodromiti Z, et al. Intrauterine inflammation and preterm delivery. Ann N Y Acad Sci. 2010;1205(1):118–22.
Romero R, Espinoza J, Kusanovic JP, et al. The preterm parturition syndrome. BJOG. 2006;113:17–42.
Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm delivery. N Engl J Med. 2000;342(20):1500–7.
Fang X, Wang Y, Zhang Y, et al. NLRP3 inflammasome and its critical role in gynecological disorders and obstetrical complications. Front Immunol. 2021;11:555826.
Miller AS, Hidalgo TN, Abrahams VM. Human fetal membrane IL-1β production in response to bacterial components is mediated by uric-acid induced NLRP3 inflammasome activation. J Reprod Immunol. 2022;149:103457.
Zhu J, Ma C, Luan X, et al. Inflammasome components and ADAMTS4 in premature rupture of membranes. Mol Med Rep. 2021;23(2):1–1.
Kemp MW. Preterm birth, intrauterine infection, and fetal inflammation. Front Immunol. 2014;5:574.
Boyle AK, Rinaldi SF, Norman JE, et al. Preterm birth: inflammation, fetal injury and treatment strategies. J Reprod Immunol. 2017;119:62–6.
Kindinger LM, Bennett PR, Lee YS, et al. The interaction between vaginal microbiota, cervical length, and vaginal progesterone treatment for preterm birth risk. Microbiome. 2017;5:1–14.
Madianos PN, Bobetsis YA, Offenbacher S. Adverse pregnancy outcomes (APO s) and periodontal disease: pathogenic mechanisms. J Clin Periodontol. 2013;40:S170–80.
Niyibizi J, Mayrand MH, Audibert F, et al. Association between human papillomavirus infection among pregnant women and preterm birth. JAMA Netw Open. 2021;4(9):e2125308–e2125308.
Easterlin MC, De Beritto T, Yeh AM, et al. Extremely preterm infant born to a mother with severe COVID-19 pneumonia. J Investig Med High Impact Case Rep. 2020;8:2324709620946621.
Wenstrom KD, Andrews WW, Bowles NE, et al. Intrauterine viral infection at the time of second trimester genetic amniocentesis. Obstet Gynecol. 1998;92(3):420–4.
Cross SN, Potter JA, Aldo P, et al. Viral infection sensitizes human fetal membranes to bacterial lipopolysaccharide by MERTK inhibition and inflammasome activation. J Immunol. 2017;199(8):2885–95.
Romero R, Miranda J, Chaiworapongsa T, et al. Prevalence and clinical significance of sterile intra-amniotic inflammation in patients with preterm labor and intact membranes. Am J Reprod Immunol. 2014;72(5):458–74.
Gomez-Lopez N, Romero R, Garcia-Flores V, et al. Inhibition of the NLRP3 inflammasome can prevent sterile intra-amniotic inflammation, preterm labor/birth, and adverse neonatal outcomes. Biol Reprod. 2019;100(5):1306–18.
Xia C, Braunstein Z, Toomey AC, et al. S100 proteins as an important regulator of macrophage inflammation. Front Immunol. 2018;8:1908.
Lannon SMR, Vanderhoeven JP, Eschenbach DA, et al. Synergy and interactions among biological pathways leading to preterm premature rupture of membranes. Reprod Sci. 2014;21(10):1215–27.
Menon R, Behnia F, Polettini J, et al. Novel pathways of inflammation in human fetal membranes associated with preterm birth and preterm pre-labor rupture of the membranes. Semin Immunopathol. 2020;42:431–50.
Polettini J, Silva MG, Kacerovsky M, et al. Screening of lysyl oxidase (LOX) and lysyl oxidase like (LOXL) enzyme expression and activity in preterm prelabor rupture of fetal membranes. J Perinat Med. 2016;44(1):99–109.
Millar LK, Stollberg J, DeBuque L, et al. Fetal membrane distention: determination of the intrauterine surface area and distention of the fetal membranes preterm and at term. Am J Obstet Gynecol. 2000;182(1):128–34.
Marom Y, Goldman S, Shalev E, et al. Characterization of irreversible physio-mechanical processes in stretched fetal membranes. Acta Biomater. 2016;30:299–310.
Joyce EM, Diaz P, Tamarkin S, et al. In-vivo stretch of term human fetal membranes. Placenta. 2016;38:57–66.
Padron JG, Norman Ing ND, Ng PK, et al. Stretch causes cell stress and the downregulation of Nrf2 in primary amnion cells. Biomolecules. 2022;12(6):766.
Kendal-Wright CE, Hubbard D, Gowin-Brown J, et al. Stretch and inflammation-induced Pre-B cell colony-enhancing factor (PBEF/Visfatin) and Interleukin-8 in amniotic epithelial cells. Placenta. 2010;31(8):665–74.
Condon JC, Jeyasuria P, Faust JM, et al. Surfactant protein secreted by the maturing mouse fetal lung acts as a hormone that signals the initiation of parturition. Proc Natl Acad Sci. 2004;101(14):4978–83.
Waldorf KMA, Singh N, Mohan AR, et al. Uterine overdistention induces preterm labor mediated by inflammation: observations in pregnant women and nonhuman primates. Am J Obstet Gynecol. 2015;213(6):830. e1-830. e19.
Menon R. Oxidative stress damage as a detrimental factor in preterm birth pathology. Front Immunol. 2014;5:567.
Chai M, Barker G, Menon R, et al. Increased oxidative stress in human fetal membranes overlying the cervix from term non-labouring and post labour deliveries. Placenta. 2012;33(8):604–10.
Myatt L. Reactive oxygen and nitrogen species and functional adaptation of the placenta. Placenta. 2010;31:S66–9.
Smith JA, Park S, Krause JS, et al. Oxidative stress, DNA damage, and the telomeric complex as therapeutic targets in acute neurodegeneration. Neurochem Int. 2013;62(5):764–75.
Armstrong E, Boonekamp J. Does oxidative stress shorten telomeres in vivo? A meta-analysis. Ageing Res Rev. 2023;85:101854.
Hoare M, Das T, Alexander G. Ageing, telomeres, senescence, and liver injury. J Hepatol. 2010;53(5):950–61.
Panelli DM, Bianco K. Cellular aging and telomere dynamics in pregnancy. Curr Opin Obstet Gynecol. 2022;34(2):57–61.
Ilekis JV, Tsilou E, Fisher S, et al. Placental origins of adverse pregnancy outcomes: potential molecular targets: an Executive Workshop Summary of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Am J Obstet Gynecol. 2016;215(1):S1–46.
Burton GJ. Oxygen, the Janus gas; its effects on human placental development and function. J Anat. 2009;215(1):27–35.
Sajjad Y, Leonard M, Doyle M. Antioxidant levels in the cord blood of term fetus. J Obstet Gynaecol. 2000;20(5):468–71.
Thornburg KL, Kolahi K, Pierce M, et al. Biological features of placental programming. Placenta. 2016;48:S47–53.
Morales-Prieto DM, Fuentes-Zacarías P, Murrieta-Coxca JM, et al. Smoking for two-effects of tobacco consumption on placenta. Mol Aspects Med. 2022;87:101023.
Buhimschi IA, Buhimschi CS, Pupkin M, et al. Beneficial impact of term labor: nonenzymatic antioxidant reserve in the human fetus. Am J Obstet Gynecol. 2003;189(1):181–8.
Lappas M, Permezel M, Rice GE. N-acetyl-cysteine inhibits phospholipid metabolism, proinflammatory cytokine release, protease activity, and Nuclear Factor-κB deoxyribonucleic acid-binding activity in human fetal membranes in vitro. J Clin Endocrinol Metab. 2003;88(4):1723–9.
Davenport AP, Hyndman KA, Dhaun N, et al. Endothelin. Pharmacol Rev. 2016;68(2):357–418.
Mendelson CR, Montalbano AP, Gao L. Fetal-to-maternal signaling in the timing of birth. J Steroid Biochem Mol Biol. 2017;170:19–27.
Renshall LJ, Beards F, Evangelinos A, et al. Targeted delivery of epidermal growth factor to the human placenta to treat fetal growth restriction. Pharmaceutics. 2021;13(11):1778.
Zaga-Clavellina V, Flores-Espinosa P, Pineda-Torres M, et al. Tissue-specific IL-10 secretion profile from term human fetal membranes stimulated with pathogenic microorganisms associated with preterm labor in a two-compartment tissue culture system. J Matern Fetal Neonatal Med. 2014;27(13):1320–7.
Boldenow E, Hogan KA, Chames MC, et al. Role of cytokine signaling in group B Streptococcus-stimulated expression of human beta defensin-2 in human extraplacental membranes. Am J Reprod Immunol. 2015;73(3):263–72.
Reinl EL, England SK. Fetal-to-maternal signaling to initiate parturition. J Clin Invest. 2015;125(7):2569–71.
Strauss JF III. Extracellular matrix dynamics and fetal membrane rupture. Reprod Sci. 2013;20(2):140–53.
Gilman-Sachs A, Dambaeva S, Garcia MDS, et al. Inflammation induced preterm labor and birth. J Reprod Immunol. 2018;129:53–8.
Richardson LS, Vargas G, Brown T, et al. Discovery and characterization of human amniochorionic membrane microfractures. Am J Pathol. 2017;187(12):2821–30.
Ji J, Yang L. Advances on human amniotic epithelial cells and its clinical application potential. Sheng li xue bao:[Acta Physiologica Sinica]. 2022;74(1):80–92.
Menon R. Fetal inflammatory response at the fetomaternal interface: a requirement for labor at term and preterm. Immunol Rev. 2022;308(1):149–67.
Richardson L, Menon R. Proliferative, migratory, and transition properties reveal metastate of human AmnionáCells. Am J Pathol. 2018;188(9):2004–15.
Menon R. Human fetal membranes at term: dead tissue or signalers of parturition? Placenta. 2016;44:1–5.
Zhu Y, Liu X, Ding X, et al. Telomere and its role in the aging pathways: telomere shortening, cell senescence and mitochondria dysfunction. Biogerontology. 2019;20:1–16.
Menon R, Yu J, Basanta-Henry P, et al. Short fetal leukocyte telomere length and preterm prelabor rupture of the membranes. PLoS ONE. 2012;7(2):e31136.
Menon R, Behnia F, Polettini J, et al. Placental membrane aging and HMGB1 signaling associated with human parturition. Aging (Albany NY). 2016;8(2):216.
Lavu N, Richardson L, Radnaa E, et al. Oxidative stress-induced downregulation of glycogen synthase kinase 3 beta in fetal membranes promotes cellular senescence. Biol Reprod. 2019;101(5):1018–30.
Fabrizio VA, Lindsay CV, Wilcox M, et al. The serotonin reuptake inhibitor fluoxetine induces human fetal membrane sterile inflammation through p38 MAPK activation. J Reprod Immunol. 2023;155:103786.
Menon R, Boldogh I, Urrabaz-Garza R, et al. Senescence of primary amniotic cells via oxidative DNA damage. PLoS ONE. 2013;8(12):e83416.
Menon R, Fortunato SJ, Milne GL, et al. Amniotic fluid eicosanoids in preterm and term births: effects of risk factors for spontaneous preterm labor. Obstet Gynecol. 2011;118(1):121.
Gratacos E, Sanin-Blair J, Lewi L, et al. A histological study of fetoscopic membrane defects to document membrane healing. Placenta. 2006;27(4–5):452–6.
Johnson JWC, Egerman RS, Moorhead J. Cases with ruptured membranes that “reseal.” Am J Obstet Gynecol. 1990;163(3):1024–30.
Behzad F, Dickinson MR, Charlton A, et al. Brief communication: sliding displacement of amnion and chorion following controlled laser wounding suggests a mechanism for short-term sealing of ruptured membranes. Placenta. 1994;15(7):775–8.
Avilla-Royo E, Ochsenbein-Kölble N, Vonzun L, et al. Biomaterial-based treatments for the prevention of preterm birth after iatrogenic rupture of the fetal membranes. Biomater Sci. 2022;10(14):3695–715.
Litwinska E, Litwinska M, Czuba B, et al. Amniocentesis in twin pregnancies: risk factors of fetal loss. J Clin Med. 2022;11(7):1937.
Mann LK, Papanna R, Moise KJ Jr, et al. Fetal membrane patch and biomimetic adhesive coacervates as a sealant for fetoscopic defects. Acta Biomater. 2012;8(6):2160–5.
Mogami H, Hari Kishore A, Akgul Y, et al. Healing of preterm ruptured fetal membranes. Sci Rep. 2017;7(1):13139.
Kawamura Y, Mogami H, Yasuda E, et al. Fetal macrophages assist in the repair of ruptured amnion through the induction of epithelial-mesenchymal transition. Sci Signal. 2022;15(751):eabi5453.
Tchirikov M, Schlabritz-Loutsevitch N, Maher J, et al. Mid-trimester preterm premature rupture of membranes (PPROM): etiology, diagnosis, classification, international recommendations of treatment options and outcome. J Perinat Med. 2018;46(5):465–88.
Lee A, Ryu KJ, Ahn KH, et al. Spontaneous healing of human amnion in the premature rupture of membrane model. Placenta. 2020;97:29–35.
Kumar D, Moore RM, Mercer BM, et al. In an in-vitro model using human fetal membranes, 17-α hydroxyprogesterone caproate is not an optimal progestogen for inhibition of fetal membrane weakening. Am J Obstet Gynecol. 2017;217(6):695. e1-695. e14.
Sonnemann KJ, Bement WM. Wound repair: toward understanding and integration of single-cell and multicellular wound responses. Annu Rev Cell Dev Biol. 2011;27:237–63.
Murray PJ, Wynn TA. Protective and pathogenic functions of macrophage subsets. Nat Rev Immunol. 2011;11(11):723–37.
Romero R, Dey SK, Fisher SJ. Preterm labor: one syndrome, many causes. Science. 2014;345(6198):760–5.
Adekola H, Gill N, Sakr S, et al. Outcomes following intra-amniotic instillation with indigo carmine to diagnose prelabor rupture of membranes in singleton pregnancies: a single center experience. J Matern Fetal Neonatal Med. 2016;29(4):544–9.
Nikolova T, Uotila J, Nikolova N, et al. Prediction of spontaneous preterm delivery in women presenting with premature labor: a comparison of placenta alpha microglobulin-1, phosphorylated insulin-like growth factor binding protein-1, and cervical length. Am J Obstet Gynecol. 2018;219(6):610. e1-610. e9.
Adama van Scheltema PN, In’t Anker PS, Vereecken A, et al. Biochemical composition of fluids for amnioinfusion during fetoscopy. Gynecol Obstet Invest. 2008;66(4):227–30.
Ronzoni S, Boucoiran I, Yudin MH, et al. Guideline No. 430: diagnosis and management of preterm prelabour rupture of membranes. J Obstet Gynaecol Can. 2022;44(11):1193-1208. e1.
Sosa CG, Herrera E, Restrepo JC, et al. Comparison of placental alpha microglobulin-1 in vaginal fluid with intra-amniotic injection of indigo carmine for the diagnosis of rupture of membranes. J Perinat Med. 2014;42(5):611–6.
Navathe R, Schoen CN, Heidari P, et al. Azithromycin vs erythromycin for the management of preterm premature rupture of membranes. Am J Obstet Gynecol. 2019;221(2):144. e1-144. e8.
Vogel JP, Nardin JM, Dowswell T, et al. Combination of tocolytic agents for inhibiting preterm labour. Cochrane Database Syst Rev. 2014;2014(7):CD006169.
Lee JH, Romero R, Kim SM, et al. A new antibiotic regimen treats and prevents intra-amniotic inflammation/infection in patients with preterm PROM. J Matern Fetal Neonatal Med. 2016;29(17):2727–37.
Yudin MH, van Schalkwyk J, Van Eyk N, et al. Antibiotic therapy in preterm premature rupture of the membranes. J Obstet Gynaecol Can. 2009;31(9):863–7.
Hutzal CE, Boyle EM, Kenyon SL, et al. Use of antibiotics for the treatment of preterm parturition and prevention of neonatal morbidity: a metaanalysis. Am J Obstet Gynecol. 2008;199(6):620. e1-620. e8.
Meeraus WH, Petersen I, Gilbert R. Association between antibiotic prescribing in pregnancy and cerebral palsy or epilepsy in children born at term: a cohort study using the health improvement network. PLoS ONE. 2015;10(3):e0122034.
Roberts D, Brown J, Medley N, et al. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2017;3(3):CD00445.
Romejko-Wolniewicz E, Teliga-Czajkowska J, Czajkowski K. Antenatal steroids: can we optimize the dose? Curr Opin Obstet Gynecol. 2014;26(2):77.
Abramovici A, Cantu J, Jenkins SM. Tocolytic therapy for acute preterm labor. Obstetrics and Gynecology Clinics. 2012;39(1):77–87.
Tchirikov M, Zhumadilov Z, Winarno AS, et al. Treatment of preterm premature rupture of membranes with oligo-/anhydramnion colonized by multiresistant bacteria with continuous amnioinfusion and antibiotic administrations through a subcutaneously implanted intrauterine port system: A case report. Fetal Diagn Ther. 2017;42(1):71–6.
Tchirikov M, Bapayeva G, Zhumadilov ZS, et al. Treatment of PPROM with anhydramnion in humans: first experience with different amniotic fluid substitutes for continuous amnioinfusion through a subcutaneously implanted port system. J Perinat Med. 2013;41(6):657–63.
Shields LE, Moore TR, Bace RA. Fetal electrolyte and acid-base responses to amnioinfusion: lactated Ringer’s versus normal saline in the ovine fetus. J Soc Gynecol Investig. 1995;2(4):602–8.
Goździewicz T, Rycel-Dziatosz M, Madziar K, et al. Long-term amnioinfusion through an intrauterine catheter in preterm premature rupture of membranes before 26 weeks of gestation: a retrospective multicenter study. Fetal Diagn Ther. 2021;48(8):582–7.
Goebel S, Naberezhnev Y, Seliger G, et al. Continuous amnioinfusion via a subcutaneously implanted port system with PPROM and anhydramnios< 28+ 0 weeks of gestation: an international prospective randomized trial. Ultraschall in der Medizin-Eur J Ultrasound. 2016;37(1):15.
Luo X, Liu Y, Pang J, et al. Thermo/photo dual-crosslinking chitosan-gelatin methacrylate hydrogel with controlled shrinking property for contraction fabrication. Carbohydr Polym. 2020;236:116067.
Devaud YR, Züger S, Zimmermann R, et al. Minimally invasive surgical device for precise application of bioadhesives to prevent iPPROM. Fetal Diagn Ther. 2019;45(2):102–10.
Young BK, Roqué H, Abdelhak YE, et al. Minimally invasive endoscopy in the treatment of preterm premature rupture of membranes by application of fibrin sealant. J Perinat Med. 2000;28(4):326–30.
Avilla-Royo E, Seehusen F, Devaud YR, et al. In vivo sealing of fetoscopy-induced fetal membrane defects by mussel glue. Fetal Diagn Ther. 2022;49(11–12):518–27.
Deprest J, Van Mieghem T, Emonds MP, et al. Amniopatch to treat iatrogenic rupture of the fetal membranes. Gynecol Obstet Fertil. 2011;39(6):378–82.
Liekens D, Lewi L, Jani J, et al. Enrichment of collagen plugs with platelets and amniotic fluid cells increases cell proliferation in sealed iatrogenic membrane defects in the foetal rabbit model. Prenat Diagn. 2008;28(6):503–7.
Quintero RA, Kontopoulos EV, Chmait R, et al. Management of twin–twin transfusion syndrome in pregnancies with iatrogenic detachment of membranes following therapeutic amniocentesis and the role of interim amniopatch. Ultrasound Obstet Gynecol. 2005;26(6):628–33.
Mogami H, Kishore AH, Word RA. Collagen type 1 accelerates healing of ruptured fetal membranes. Sci Rep. 2018;8(1):696.
Papanna R, Mann LK, Tseng SCG, et al. Cryopreserved human amniotic membrane and a bioinspired underwater adhesive to seal and promote healing of iatrogenic fetal membrane defect sites. Placenta. 2015;36(8):888–94.
Méhats C, Schmitz T, Marcellin L, et al. Biochemistry of fetal membranes rupture. Gynecol Obstet Fertil. 2011;39(6):365–9.
Zhang Q, Lai D. Application of human amniotic epithelial cells in regenerative medicine: a systematic review. Stem Cell Res Ther. 2020;11(1):1–16.
Zheng Y, Ji S, Wu H, et al. Topical administration of cryopreserved living micronized amnion accelerates wound healing in diabetic mice by modulating local microenvironment. Biomaterials. 2017;113:56–67.
Zhou Z, Xun J, Wu C, et al. Acceleration of burn wound healing by micronized amniotic membrane seeded with umbilical cord-derived mesenchymal stem cells. Mater Today Bio. 2023;20:100686.
Richardson LS, Taylor RN, Menon R. Reversible EMT and MET mediate amnion remodeling during pregnancy and labor. Sci Signal. 2020;13(618):eaay1486.
Cazzell S, Stewart J, Agnew PS, et al. Randomized controlled trial of micronized dehydrated human amnion/chorion membrane (dHACM) injection compared to placebo for the treatment of plantar fasciitis. Foot Ankle Int. 2018;39(10):1151–61.
Clare G, Suleman H, Bunce C, et al. Amniotic membrane transplantation for acute ocular burns. Cochrane Database Syst Rev. 2022;9(9):CD009379.
Castellanos G, Bernabe-Garcia A, Moraleda JM, et al. Amniotic membrane application for the healing of chronic wounds and ulcers. Placenta. 2017;59:146–53.
Andrewartha N, Yeoh G. Human amnion epithelial cell therapy for chronic liver disease. Stem Cells Int. 2019;2019:1–10.
Kalluri R. EMT: when epithelial cells decide to become mesenchymal-like cells. J Clin Invest. 2009;119(6):1417–9.
Tantengco OAG, Vink J, Medina PMB, et al. Oxidative stress promotes cellular damages in the cervix: implications for normal and pathologic cervical function in human pregnancy. Biol Reprod. 2021;105(1):204–16.
Acknowledgements
The authors express their gratitude for the National Natural Science Foundation of China (12002232, 12272251), the General Project Basic Research Program of Shanxi Province (202103021223100), the Department of Science and Technology of Shanxi Province [No. 20210302124305], and the Project founded by Health Commission of Shanxi Province [No. 2021132].
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
All involved consented to publication.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yang Liu and Junmei Fan were recognized as co-corresponding authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, L., Yang, T., Wen, M. et al. Frontiers in the Etiology and Treatment of Preterm Premature Rupture of Membrane: From Molecular Mechanisms to Innovative Therapeutic Strategies. Reprod. Sci. 31, 917–931 (2024). https://doi.org/10.1007/s43032-023-01411-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-023-01411-9