Abstract
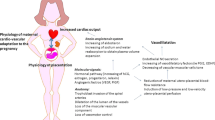
Early onset fetal growth restriction (FGR) is one of the main adverse pregnancy conditions, often associated with poor neonatal outcomes. Frequently, early onset FGR is associated with early onset hypertensive disorders of pregnancy (HDP), and in particular preeclampsia (PE). However, to date, it is still an open question whether pregnancies complicated by early FGR plus HDP (FGR-HDP) and those complicated by early onset FGR without HDP (normotensive-FGR (n-FGR)) show different prenatal and postnatal outcomes and, consequently, should benefit from different management and long-term follow-up. Recent data support the hypothesis that the presence of PE may have an additional impact on maternal hemodynamic impairment and placental lesions, increasing the risk of poor neonatal outcomes in pregnancy affected by early onset FGR-HDP compared to pregnancy affected by early onset n-FGR. This review aims to elucidate this poor studied topic, comparing the clinical characteristics, perinatal outcomes, and potential long-term sequelae of early onset FGR-HDP and early onset n-FGR.


Similar content being viewed by others
Data Availability
The authors confirm that the data supporting the findings of this study are available within the article.
References
Resnik R. Intrauterine growth restriction. Obstet Gynecol. 2002;99(3):490–6.
Lees CC, Stampalija T, Baschat AA, et al. ISUOG Practice guidelines: diagnosis and management of small-for-gestational-age fetus and fetal growth restriction. Ultrasound Obstet Gynecol. 2020;56(2):298–312.
Mecacci F, Avagliano L, Lisi F, et al. Fetal growth restriction: does an integrated maternal hemodynamic-placental model fit better? Reprod Sci. 2021;28(9):2422–35.
Figueras F, Caradeux J, Crispi F, Eixarch E, Peguero A, Gratacos E. Diagnosis and surveillance of late-onset fetal growth restriction. Am J Obstet Gynecol. 2018;218(2):S790–802.
Ferrazzi E, Zullino S, Stampalija T, et al. Bedside diagnosis of two major clinical phenotypes of hypertensive disorders of pregnancy: clinical phenotypes of HDP. Ultrasound Obstet Gynecol. 2016;48(2):224–31.
Foo FL, Mahendru AA, Masini G, et al. Association between prepregnancy cardiovascular function and subsequent preeclampsia or fetal growth restriction. Hypertension. 2018;72(2):442–50.
Thilaganathan B. Placental syndromes: getting to the heart of the matter: perspective. Ultrasound Obstet Gynecol. 2017;49(1):7–9.
Di Martino DD, Stampalija T, Zullino S, et al. Maternal hemodynamic profile during pregnancy and in the post-partum in hypertensive disorders of pregnancy and fetal growth restriction. Am J Obstet Gynecol MFM. 2023;5(3):100841.
Ornaghi S, Caricati A, Di Martino DD, et al. Non-invasive maternal hemodynamic assessment to classify high-risk pregnancies complicated by fetal growth restriction. Front Clin Diabetes Healthc. 2022;3:851971.
Kovo M, Schreiber L, Elyashiv O, Ben-Haroush A, Abraham G, Bar J. Pregnancy outcome and placental findings in pregnancies complicated by fetal growth restriction with and without preeclampsia. Reprod Sci. 2015;22(3):316–21.
Huppertz B. Placental pathology in pregnancy complications. Thromb Res. 2011;127:S96–9.
Redman CWG, Staff AC, Roberts JM. Syncytiotrophoblast stress in preeclampsia: the convergence point for multiple pathways. Am J Obstet Gynecol. 2022;226(2):S907–27.
Huppertz B. Trophoblast differentiation, fetal growth restriction and preeclampsia. Pregnancy Hypertens Int J Womens Cardiovasc Health. 2011;1(1):79–86.
Mayhew TM. A stereological perspective on placental morphology in normal and complicated pregnancies. J Anat. 2009;215(1):77–90.
Herraiz I, Quezada MS, Rodriguez-Calvo J, Gómez-Montes E, Villalaín C, Galindo A. Longitudinal change of sFlt-1/PlGF ratio in singleton pregnancy with early-onset fetal growth restriction. Ultrasound Obstet Gynecol. 2018;52(5):631–8.
Di Martino DD, Avagliano L, Ferrazzi E, et al. Hypertensive disorders of pregnancy and fetal growth restriction: clinical characteristics and placental lesions and possible preventive nutritional targets. Nutrients. 2022;14(16):3276.
Chen W, Wei Q, Liang Q, Song S, Li J. Diagnostic capacity of sFlt-1/PlGF ratio in fetal growth restriction: a systematic review and meta-analysis. Placenta. 2022;127:37–42.
Stepan H, Hund M, Andraczek T. Combining biomarkers to predict pregnancy complications and redefine preeclampsia: the angiogenic-placental syndrome. Hypertension. 2020;75(4):918–26.
Herraiz I, Llurba E, Verlohren S, Galindo A. on behalf of the Spanish Group for the study of angiogenic markers in preeclampsia. Update on the diagnosis and prognosis of preeclampsia with the aid of the sFlt-1/ PlGF ratio in singleton pregnancies. Fetal Diagn Ther. 2018;43(2):81–9.
Lim S, Li W, Kemper J, Nguyen A, Mol BW, Reddy M. Biomarkers and the prediction of adverse outcomes in preeclampsia: a systematic review and meta-analysis. Obstet Gynecol. 2021;137(1):72–81.
Veisani Y, Jenabi E, Delpisheh A, Khazaei S. Angiogenic factors and the risk of preeclampsia: a systematic review and meta-analysis. Int J Reprod Biomed. 2019;17(1):1.
Stepan H, Galindo A, Hund M, et al. Clinical utility of sFlt-1 and PlGF in screening, prediction, diagnosis and monitoring of pre-eclampsia and fetal growth restriction. Ultrasound Obstet Gynecol. 2022;61:168–80.
Agrawal S, Shinar S, Cerdeira AS, Redman C, Vatish M. Predictive performance of PlGF (placental growth factor) for screening preeclampsia in asymptomatic women: a systematic review and meta-analysis. Hypertension. 2019;74(5):1124–35.
Agrawal S, Cerdeira AS, Redman C, Vatish M. Meta-analysis and systematic review to assess the role of soluble FMS-Like tyrosine kinase-1 and placenta growth factor ratio in prediction of preeclampsia: the SaPPPhirE study. Hypertension. 2018;71(2):306–16.
NICE National Istitute for Health and Care Excellence. PlGF-based testing to help diagnose suspected pre-eclampsia. In: Diagnostics guidance; 2022.
Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, et al. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J. 2018;39(34):3165–241.
Hund M, Allegranza D, Schoedl M, Dilba P, Verhagen-Kamerbeek W, Stepan H. Multicenter prospective clinical study to evaluate the prediction of short-term outcome in pregnant women with suspected preeclampsia (PROGNOSIS): study protocol. BMC Pregnancy Childbirth. 2014;14(1):324.
Zeisler H, Llurba E, Chantraine F, et al. Predictive value of the sFlt-1:PlGF ratio in women with suspected preeclampsia. N Engl J Med. 2016;374(1):13–22.
Stepan H, Herraiz I, Schlembach D, et al. Implementation of the sFlt-1/PlGF ratio for prediction and diagnosis of pre-eclampsia in singleton pregnancy: implications for clinical practice. Ultrasound Obstet Gynecol. 2015;45(3):241–6.
Zhao M, Zhu Z, Liu C, Zhang Z. Dual-cutoff of sFlt-1/PlGF ratio in the stratification of preeclampsia: a systematic review and meta-analysis. Arch Gynecol Obstet. 2017;295(5):1079–87.
Rana S, Powe CE, Salahuddin S, et al. Angiogenic factors and the risk of adverse outcomes in women with suspected preeclampsia. Circulation. 2012;125(7):911–9. https://doi.org/10.1161/CIRCULATIONAHA.111.054361.
Verlohren S, Herraiz I, Lapaire O, et al. The sFlt-1/PlGF ratio in different types of hypertensive pregnancy disorders and its prognostic potential in preeclamptic patients. Am J Obstet Gynecol. 2012;206(1):58.e1–8.
Bonacina E, Armengol-Alsina M, Hurtado I, et al. sFlt-1 to PlGF ratio cut-offs to predict adverse pregnancy outcomes in early-onset FGR and SGA: a prospective observational study. J Obstet Gynaecol. 2022;42(7):2840–5.
Signore C, Mills JL, Qian C, et al. Circulating angiogenic factors and placental abruption. Obstet Gynecol. 2006;108(2):338–44.
Kumar M, Balyan K, Debnath E, Shankar S, Apte A, Jha S. Role of sFLT-1/PlGF ratio in predicting severe adverse materno-fetal outcome in high risk women. Pregnancy Hypertens. 2022;30:154–60.
Herraiz I, Simón E, Gómez-Arriaga PI, et al. Clinical implementation of the sFlt-1/PlGF ratio to identify preeclampsia and fetal growth restriction: a prospective cohort study. Pregnancy Hypertens. 2018;13:279–85.
Kwiatkowski S, Dołegowska B, Kwiatkowska E, et al. Maternal endothelial damage as a disorder shared by early preeclampsia, late preeclampsia and intrauterine growth restriction. J Perinat Med. 2017;45(7):793–802.
Hendrix M, Bons J, Van Haren A, et al. Role of sFlt-1 and PlGF in the screening of small-for-gestational age neonates during pregnancy: a systematic review. Ann Clin Biochem Int J Lab Med. 2020;57(1):44–58.
Triunfo S, Lobmaier S, Parra-Saavedra M, et al. Angiogenic factors at diagnosis of late-onset small-for-gestational age and histological placental underperfusion. Placenta. 2014;35(6):398–403.
Triunfo S, Crovetto F, Crispi F, et al. Association of first-trimester angiogenic factors with placental histological findings in late-onset preeclampsia. Placenta. 2016;42:44–50.
Kovo M, Schreiber L, Ben-Haroush A, Wand S, Golan A, Bar J. Placental vascular lesion differences in pregnancy-induced hypertension and normotensive fetal growth restriction. Am J Obstet Gynecol. 2010;202(6):561.e1–5.
Veerbeek JHW, Nikkels PGJ, Torrance HL, et al. Placental pathology in early intrauterine growth restriction associated with maternal hypertension. Placenta. 2014;35(9):696–701.
Vakil P, Henry A, Craig ME, Gow ML. A review of infant growth and psychomotor developmental outcomes after intrauterine exposure to preeclampsia. BMC Pediatr. 2022;22(1):513.
Villar J, Carroli G, Wojdyla D, et al. Preeclampsia, gestational hypertension and intrauterine growth restriction, related or independent conditions? Am J Obstet Gynecol. 2006;194(4):921–31.
Lees C, Marlow N, Arabin B, et al. Perinatal morbidity and mortality in early-onset fetal growth restriction: cohort outcomes of the trial of randomized umbilical and fetal flow in Europe (TRUFFLE): short-term outcomes following early FGR. Ultrasound Obstet Gynecol. 2013;42(4):400–8.
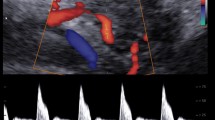
Arduini D, Rizzo G, Romanini C. The development of abnormal heart rate patterns after absent end-diastolic velocity in umbilical artery: analysis of risk factors. Am J Obstet Gynecol. 1993;168(1):43–50.
Bekedam DJ, Visser GHA, van der Zee AGJ, Snijders RJM, Poelmann-Weesjes G. Abnormal velocity waveforms of the umbilical artery in growth retarded fetuses: relationship to antepartum late heart rate decelerations and outcome. Early Hum Dev. 1990;24(1):79–89.
Hecher K, Hackelöer BJ. Cardiotocogram compared to Doppler investigation of the fetal circulation in the premature growth-retarded fetus: longitudinal observations: cardiotocography and fetal Doppler. Ultrasound Obstet Gynecol. 1997;9(3):152–61.
Mari G, Hanif F, Kruger M. Sequence of cardiovascular changes in IUGR in pregnancies with and without preeclampsia. Prenat Diagn. 2008;28(5):377–83.
Bar J, Weiner E, Levy M, Gilboa Y. The thrifty phenotype hypothesis: the association between ultrasound and Doppler studies in fetal growth restriction and the development of adult disease. Am J Obstet Gynecol MFM. 2021;3(6):100473.
Ashraf UM, Hall DL, Rawls AZ, Alexander BT. Epigenetic processes during preeclampsia and effects on fetal development and chronic health. Clin Sci. 2021;135(19):2307–27.
De Boo HA, Harding JE. The developmental origins of adult disease (Barker) hypothesis. Aust N Z J Obstet Gynaecol. 2006;46(1):4–14.
Martyn CN, Gale CR, Jespersen S, Sherriff SB. Impaired fetal growth and atherosclerosis of carotid and peripheral arteries. Lancet. 1998;352(9123):173–8.
Chan PYL, Morris JM, Leslie GI, Kelly PJ, Gallery EDM. The long-term effects of prematurity and intrauterine growth restriction on cardiovascular, renal, and metabolic function. Int J Pediatr. 2010;2010:1–10.
Schreuder M, Delemarre-van de Waal H, van Wijk A. Consequences of intrauterine growth restriction for the kidney. Kidney Blood Press Res. 2006;29(2):108–25.
Crispi F, Miranda J, Gratacós E. Long-term cardiovascular consequences of fetal growth restriction: biology, clinical implications, and opportunities for prevention of adult disease. Am J Obstet Gynecol. 2018;218(2):S869–79.
Alici Davutoglu E, Ozel A, Oztunc F, Madazli R. Modified myocardial performance index and its prognostic significance for adverse perinatal outcome in early and late onset fetal growth restriction. J Matern Fetal Neonatal Med. 2020;33(2):277–82.
Crispi F, Hernandez-Andrade E, Pelsers MMAL, et al. Cardiac dysfunction and cell damage across clinical stages of severity in growth-restricted fetuses. Am J Obstet Gynecol. 2008;199(3):254.e1–8.
Tranquilli AL, Landi B, Giannubilo SR, Sibai BM. Preeclampsia: no longer solely a pregnancy disease. Pregnancy Hypertens Int J Womens Cardiovasc Health. 2012;2(4):350–7.
Tenhola S, Rahiala E, Halonen P, Vanninen E, Voutilainen R. Maternal preeclampsia predicts elevated blood pressure in 12-year-old children: evaluation by ambulatory blood pressure monitoring. Pediatr Res. 2006;59(2):320–4.
Davis EF, Lazdam M, Lewandowski AJ, et al. Cardiovascular risk factors in children and young adults born to preeclamptic pregnancies: a systematic review. Pediatrics. 2012;129(6):e1552–61.
Pinheiro TV, Brunetto S, Ramos JGL, Bernardi JR, Goldani MZ. Hypertensive disorders during pregnancy and health outcomes in the offspring: a systematic review. J Dev Orig Health Dis. 2016;7(4):391–407.
Karatza AA, Dimitriou G. Preeclampsia emerging as a novel risk factor for cardiovascular disease in the offspring. Curr Pediatr Rev. 2020;16(3):194–9.
Lazdam M, de la Horra A, Pitcher A, et al. Elevated blood pressure in offspring born premature to hypertensive pregnancy: is endothelial dysfunction the underlying vascular mechanism? Hypertension. 2010;56(1):159–65.
Lewandowski AJ, Augustine D, Lamata P, et al. Preterm heart in adult life: cardiovascular magnetic resonance reveals distinct differences in left ventricular mass, geometry, and function. Circulation. 2013;127(2):197–206.
Youssef L, Miranda J, Paules C, et al. Fetal cardiac remodeling and dysfunction is associated with both preeclampsia and fetal growth restriction. Am J Obstet Gynecol. 2020;222(1):79.e1–9.
Crispi F, Domínguez C, Llurba E, Martín-Gallán P, Cabero L, Gratacós E. Placental angiogenic growth factors and uterine artery Doppler findings for characterization of different subsets in preeclampsia and in isolated intrauterine growth restriction. Am J Obstet Gynecol. 2006;195(1):201–7.
Kvehaugen AS, Dechend R, Ramstad HB, Troisi R, Fugelseth D, Staff AC. Endothelial function and circulating biomarkers are disturbed in women and children after preeclampsia. Hypertension. 2011;58(1):63–9.
Barker D, Eriksson J, Forsén T, Osmond C. Fetal origins of adult disease: strength of effects and biological basis. Int J Epidemiol. 2002;31(6):1235–9.
Morrison JL, Duffield JA, Muhlhausler BS, Gentili S, McMillen IC. Fetal growth restriction, catch-up growth and the early origins of insulin resistance and visceral obesity. Pediatr Nephrol. 2010;25(4):669–77.
Dahlquist GG, Patterson C, Soltesz G. Perinatal risk factors for childhood type 1 diabetes in Europe. The EURODIAB Substudy 2 Study Group. Diabetes Care. 1999;22(10):1698–702.
Yang L, Huang C, Zhao M, et al. Maternal hypertensive disorders during pregnancy and the risk of offspring diabetes mellitus in childhood, adolescence, and early adulthood: a nationwide population-based cohort study. BMC Med. 2023;21(1):59.
Malhotra A, Allison BJ, Castillo-Melendez M, Jenkin G, Polglase GR, Miller SL. Neonatal morbidities of fetal growth restriction: pathophysiology and impact. Front Endocrinol. 2019;10:55.
Gagliardi L, Rusconi F, Da Frè M, et al. Pregnancy disorders leading to very preterm birth influence neonatal outcomes: results of the population-based ACTION cohort study. Pediatr Res. 2013;73(6):794–801.
Collaborators of the hypertensive disorders of pregnancy study group, Rocha G, De Lima FF, Machado AP, Guimarães H. Preeclampsia predicts higher incidence of bronchopulmonary dysplasia. J Perinatol. 2018;38(9):1165–73.
Hansen AR, Barnés CM, Folkman J, McElrath TF. Maternal preeclampsia predicts the development of bronchopulmonary dysplasia. J Pediatr. 2010;156(4):532–6.
Brembilla G, Righini A, Scelsa B, et al. Neuroimaging and neurodevelopmental outcome after early fetal growth restriction: NEUROPROJECT—FGR. Pediatr Res. 2021;90(4):869–75.
Baschat AA. Neurodevelopment after fetal growth restriction. Fetal Diagn Ther. 2014;36(2):136–42.
Morsing E, Brodszki J, Thuring A, Maršál K. Infant outcome after active management of early-onset fetal growth restriction with absent or reversed umbilical artery blood flow. Ultrasound Obstet Gynecol. 2021;57(6):931–41.
Kajantie E, Eriksson JG, Osmond C, Thornburg K, Barker DJP. Pre-eclampsia is associated with increased risk of stroke in the adult offspring: the Helsinki Birth Cohort Study. Stroke. 2009;40(4):1176–80.
Li C, Miao JK, Xu Y, et al. Prenatal, perinatal and neonatal risk factors for perinatal arterial ischaemic stroke: a systematic review and meta-analysis. Eur J Neurol. 2017;24(8):1006–15.
Lehman LL, Rivkin MJ. Perinatal arterial ischemic stroke: presentation, risk factors, evaluation, and outcome. Pediatr Neurol. 2014;51(6):760–8.
van Esch JJA, van Heijst AF, de Haan AFJ, van der Heijden OWH. Early-onset preeclampsia is associated with perinatal mortality and severe neonatal morbidity. J Matern Fetal Neonatal Med. 2017;30(23):2789–94.
Jelin A, Cheng Y, Shaffer B, Kaimal A, Little S, Caughey A. Early-onset preeclampsia and neonatal outcomes. J Matern Fetal Neonatal Med. 2009;23:1–5.
Kong L, Chen X, Liang Y, Forsell Y, Gissler M, Lavebratt C. Association of preeclampsia and perinatal complications with offspring neurodevelopmental and psychiatric disorders. JAMA Netw Open. 2022;5(1):e2145719.
Walker CK, Krakowiak P, Baker A, Hansen RL, Ozonoff S, Hertz-Picciotto I. Preeclampsia, placental insufficiency, and autism spectrum disorder or developmental delay. JAMA Pediatr. 2015;169(2):154. https://doi.org/10.1001/jamapediatrics.2014.2645.
Zheng W, Zhang X, Feng Y, et al. Association of corpus callosum development with fetal growth restriction and maternal preeclampsia or gestational hypertension. JAMA Netw Open. 2022;5(8):e2226696.
Warshafsky C, Pudwell J, Walker M, Wen SW, Smith GN. Prospective assessment of neurodevelopment in children following a pregnancy complicated by severe pre-eclampsia. BMJ Open. 2016;6(7):e010884.
Many A, Fattal A, Leitner Y, Kupferminc MJ, Harel S, Jaffa A. Neurodevelopmental and cognitive assessment of children born growth restricted to mothers with and without preeclampsia. Hypertens Pregnancy. 2003;22(1):25–9.
Morsing E, Maršál K. Pre-eclampsia—an additional risk factor for cognitive impairment at school age after intrauterine growth restriction and very preterm birth. Early Hum Dev. 2014;90(2):99–101.
Crispi F, Comas M, Hernández-Andrade E, et al. Does pre-eclampsia influence fetal cardiovascular function in early-onset intrauterine growth restriction? Ultrasound Obstet Gynecol. 2009;34(6):660–5.
Afzal-Ahmed I, Mann GE, Shennan AH, Poston L, Naftalin RJ. Preeclampsia inactivates glucose-6-phosphate dehydrogenase and impairs the redox status of erythrocytes and fetal endothelial cells. Free Radic Biol Med. 2007;42(12):1781–90.
Yuluğ E, Yenilmez E, Unsal MA, Aydin S, Tekelioglu Y, Arvas H. Apoptotic and morphological features of the umbilical artery endothelium in mild and severe pre-eclampsia. Acta Obstet Gynecol Scand. 2006;85(9):1038–45.
Marchi L, Pasquini L, Elvan-Taspinar A, Bilardo CM. Cardiovascular hemodynamic changes after antenatal corticosteroids in growth restricted and appropriate for gestational age fetuses. Ultraschall Med - Eur J Ultrasound. 2020;41(03):292–9.
Fratelli N, Prefumo F, Wolf H, et al. Effects of antenatal betamethasone on fetal Doppler indices and short term fetal heart rate variation in early growth restricted fetuses. Ultraschall Med - Eur J Ultrasound. 2021;42(01):56–64.
Morrison JL, Botting KJ, Soo PS, et al. Antenatal steroids and the IUGR fetus: are exposure and physiological effects on the lung and cardiovascular system the same as in normally grown fetuses? J Pregnancy. 2012;2012:1–15.
Bernstein IM, Horbar JD, Badger GJ, Ohlsson A, Golan A. Morbidity and mortality among very-low-birth-weight neonates with intrauterine growth restriction. Am J Obstet Gynecol. 2000;182(1):198–206.
Magann EF, Bass D, Chauhan SP, Sullivan DL, Martin RW, Martin JN. Antepartum corticosteroids: disease stabilization in patients with the syndrome of hemolysis, elevated liver enzymes, and low platelets (HELLP). Am J Obstet Gynecol. 1994;171(4):1148–53.
Amorim MMR, Santosa LC, Faúndes A. Corticosteroid therapy for prevention of respiratory distress syndrome in severe preeclampsia. Am J Obstet Gynecol. 1999;180(5):1283–8.
van Runnard Heimel PJ, Huisjes AJM, Franx A, Koopman C, Bots ML, Bruinse HW. A randomised placebo-controlled trial of prolonged prednisolone administration to patients with HELLP syndrome remote from term. Eur J Obstet Gynecol Reprod Biol. 2006;128(1-2):187–93.
Hagen A, Ebert A, Lange J, Zemlin M, Hopp H. The impact of pregnancy-prolonging management on maternal and neonatal morbidity in HELLP-Syndrom. Zentralbl Gynakol. 2001;123(9):513–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mecacci, F., Romani, E., Clemenza, S. et al. Early Fetal Growth Restriction with or Without Hypertensive Disorders: a Clinical Overview. Reprod. Sci. 31, 591–602 (2024). https://doi.org/10.1007/s43032-023-01330-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-023-01330-9