Abstract
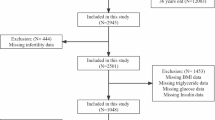
At present, the effect of body fat distribution on female reproductive health is still inconclusive. The purpose of our study was to analyze the correlation between female infertility rates and the fat mass portion of the android region to the gynoid region (the A/G ratio) among US women of reproductive age. Female infertility is defined as a failure to get pregnant after 12 months of unprotected sexual activity. A total of 3434 women of reproductive age were included in this study as part of the 2013–2018 National Health and Nutrition Examination Survey (NHANES). The A/G ratio was used to assess the body fat distribution of participants. Based on the comprehensive study design and sample weights, it was determined that the A/G ratio was associated with female infertility primarily through logistic regression analyses. After adjusting for potential confounders, the multivariate regression analysis indicated an increase in the A/G ratio was correlated with an increase in the prevalence of female infertility (OR = 4.374, 95% CI:1.809–10.575). Subgroup analyses showed an increased prevalence of infertility in non-Hispanic Whites (P = 0.012), non-diabetic individuals (P = 0.008), individuals under 35 years old (P = 0.002), and individuals with secondary infertility (P = 0.01). The trend tests and smooth curve fitting illustrate a linear trend between the A/G ratio and female infertility. Future researches are warranted to confirm the causal relationship between body fat distribution and female infertility, which may provide an insight into future prevention and treatment of female infertility.


Similar content being viewed by others
Data Availability
The survey data are publicly available on the internet for data users and researchers throughout the world http://www.cdc.gov/nchs/nhanes/.
Code Availability
All statistical analyses were conducted using SAS; programs are available from the corresponding author upon request.
Abbreviations
- A/G ratio:
-
The fat mass portion of the android region to the gynoid region
- NHANES:
-
National Health and Nutrition Examination Survey
- CDC:
-
Centers for Disease Control
- PCOS:
-
Polycystic ovary syndrome
- DXA:
-
Dual-energy X-ray absorptiometry
- NCHS:
-
National Center for Health Statistics
- PIR:
-
Poverty to income ratio
- GAM:
-
The generalized additive model
- MRI:
-
Magnetic resonance imaging
- CT:
-
Computed tomography
References
Carson SA, Kallen AN. Diagnosis and management of infertility: a review. JAMA. 2021;326(1):65–76. https://doi.org/10.1001/jama.2021.4788.
Ou XH, Zhu CC, Sun SC. Effects of obesity and diabetes on the epigenetic modification of mammalian gametes. J Cell Physiol. 2019;234(6):7847–55. https://doi.org/10.1002/jcp.27847.
Macaluso M, Wright-Schnapp TJ, Chandra A, et al. A public health focus on infertility prevention, detection, and management. Fertil Steril. 2010;93(1):16.e1-10. https://doi.org/10.1016/j.fertnstert.2008.09.046.
Jaacks LM, Vandevijvere S, Pan A, et al. The obesity transition: stages of the global epidemic. Lancet Diabetes Endocrinol. 2019;7(3):231–40. https://doi.org/10.1016/S2213-8587(19)30026-9.
Zhu L, Zhou B, Zhu X, et al. Association between body mass index and female infertility in the United States: data from National Health and Nutrition Examination Survey 2013–2018. Int J Gen Med. 2022;15:1821–31. https://doi.org/10.2147/IJGM.S349874.
Liou TH, Yang JH, Hsieh CH, Lee CY, Hsu CS, Hsu MI. Clinical and biochemical presentations of polycystic ovary syndrome among obese and nonobese women. Fertil Steril. 2009;92(6):1960–5. https://doi.org/10.1016/j.fertnstert.2008.09.003.
Barber TM, Golding SJ, Alvey C, et al. Global adiposity rather than abnormal regional fat distribution characterizes women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2008;93(3):999–1004. https://doi.org/10.1210/jc.2007-2117.
Dolfing JG, Stassen CM, van Haard PM, Wolffenbuttel BH, Schweitzer DH. Comparison of MRI-assessed body fat content between lean women with polycystic ovary syndrome (PCOS) and matched controls: less visceral fat with PCOS. Hum Reprod. 2011;26(6):1495–500. https://doi.org/10.1093/humrep/der070.
Wass P, Waldenström U, Rössner S, Hellberg D. An android body fat distribution in females impairs the pregnancy rate of in-vitro fertilization-embryo transfer. Hum Reprod. 1997;12(9):2057–60. https://doi.org/10.1093/humrep/12.9.2057.
Messina C, Albano D, Gitto S, et al. Body composition with dual energy X-ray absorptiometry: from basics to new tools. Quant Imaging Med Surg. 2020;10(8):1687–98. https://doi.org/10.21037/qims.2020.03.02.
Zhu K, Walsh JP, Murray K, Hunter M, Hui J, Hung J. DXA-derived vs standard anthropometric measures for predicting cardiometabolic risk in middle-aged australian men and women. J Clin Densitom. 2022;25(3):299–307. https://doi.org/10.1016/j.jocd.2022.01.006.
Lu Z, Tilly MJ, Aribas E, et al. Imaging-based body fat depots and new-onset atrial fibrillation in general population: a prospective cohort study. BMC Med. 2022;20(1):317. https://doi.org/10.1186/s12916-022-02505-y.
Ma M, Liu X, Jia G, Geng B, Xia Y. The association between body fat distribution and bone mineral density: evidence from the US population. BMC Endocr Disord. 2022;22(1):170. https://doi.org/10.1186/s12902-022-01087-3.
Godinho-Mota J, Gonçalves LV, Soares LR, et al. Abdominal adiposity and physical inactivity are positively associated with breast cancer: a case-control study. Biomed Res Int. 2018;2018:4783710. https://doi.org/10.1155/2018/4783710.
Xiao Z, Xu H. Gender-specific body composition relationships between adipose tissue distribution and peak bone mineral density in young Chinese adults. Biomed Res Int. 2020;2020:6724749. https://doi.org/10.1155/2020/6724749.
Ciardullo S, Oltolini A, Cannistraci R, Muraca E, Perseghin G. Sex-related association of nonalcoholic fatty liver disease and liver fibrosis with body fat distribution in the general US population. Am J Clin Nutr. 2022;115(6):1528–34. https://doi.org/10.1093/ajcn/nqac059.
Curtin LR, Mohadjer LK, Dohrmann SM, et al. The National Health and Nutrition Examination Survey: sample design, 1999–2006. Vital Health Stat 2. 2012;155:1–39.
Shepherd JA, Fan B, Lu Y, et al. A multinational study to develop universal standardization of whole-body bone density and composition using GE Healthcare Lunar and Hologic DXA systems. J Bone Miner Res. 2012;27(10):2208–16. https://doi.org/10.1002/jbmr.1654.
Venkatesh SS, Ferreira T, Benonisdottir S, et al. Obesity and risk of female reproductive conditions: a Mendelian randomisation study. PLoS Med. 2022;19(2):e1003679. https://doi.org/10.1371/journal.pmed.1003679.
Lainez NM, Coss D. Obesity, Neuroinflammation, and reproductive function. Endocrinology. 2019;160(11):2719–36. https://doi.org/10.1210/en.2019-00487.
Zaadstra BM, Seidell JC, Van Noord PA, et al. Fat and female fecundity: prospective study of effect of body fat distribution on conception rates. BMJ. 1993;306(6876):484–7. https://doi.org/10.1136/bmj.306.6876.484.
Adamska A, Raczkowski A, Stachurska Z, et al. Body composition and serum concentration of thyroid hormones in euthyroid men and women from general population. J Clin Med. 2022;11(8). https://doi.org/10.3390/jcm11082118
Adamska A, Popławska-Kita A, Siewko K, et al. Body composition and serum anti-Müllerian hormone levels in euthyroid caucasian women with hashimoto thyroiditis. Front Endocrinol (Lausanne). 2021;12:657752. https://doi.org/10.3389/fendo.2021.657752.
Delitala AP, Capobianco G, Delitala G, Cherchi PL, Dessole S. Polycystic ovary syndrome, adipose tissue and metabolic syndrome. Arch Gynecol Obstet. 2017;296(3):405–19. https://doi.org/10.1007/s00404-017-4429-2.
Pierre A, Taieb J, Giton F, et al. Dysregulation of the anti-Müllerian hormone system by steroids in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2017;102(11):3970–8. https://doi.org/10.1210/jc.2017-00308.
Polak AM, Adamska A, Krentowska A, et al. Body composition, serum concentrations of androgens and insulin resistance in different polycystic ovary syndrome phenotypes. J Clin Med. 2020;9(3). https://doi.org/10.3390/jcm9030732
Jiang K, Luan H, Pu X, Wang M, Yin J, Gong R. Association between visceral adiposity index and insulin resistance: a cross-sectional study based on US adults. Front Endocrinol (Lausanne). 2022;13:921067. https://doi.org/10.3389/fendo.2022.921067.
Brüning JC, Gautam D, Burks DJ, et al. Role of brain insulin receptor in control of body weight and reproduction. Science. 2000;289(5487):2122–5. https://doi.org/10.1126/science.289.5487.2122.
Dickmann U, Ritter G, Kretzschmar H. Pemphigoid and cerebral infarct. Syntropy of 2 diseases? Case report. Nervenarzt. 1986;57(5):309–10.
Marseglia L, Manti S, D’Angelo G, et al. Oxidative stress in obesity: a critical component in human diseases. Int J Mol Sci. 2014;16(1):378–400. https://doi.org/10.3390/ijms16010378.
Velez LM, Seldin M, Motta AB. Inflammation and reproductive function in women with polycystic ovary syndrome†. Biol Reprod. 2021;104(6):1205–17. https://doi.org/10.1093/biolre/ioab050.
Martin JH, Nixon B, Cafe SL, Aitken RJ, Bromfield EG, Lord T. Oxidative stress and reproductive function: oxidative stress and in vitro ageing of the post-ovulatory oocyte: an update on recent advances in the field. Reproduction. 2022;164(6):F109–24. https://doi.org/10.1530/REP-22-0206.
Manolopoulos KN, Karpe F, Frayn KN. Gluteofemoral body fat as a determinant of metabolic health. Int J Obes (Lond). 2010;34(6):949–59. https://doi.org/10.1038/ijo.2009.286.
Abdo NM, Ahmad H, Loney T, et al. Characterization of fertility clinic attendees in the Abu Dhabi Emirate, United Arab Emirates: a cross-sectional study. Int J Environ Res Public Health. 2023;20(3)
Dongarwar D, Mercado-Evans V, Adu-Gyamfi S, Laracuente ML, Salihu HM. Racial/ethnic disparities in infertility treatment utilization in the US, 2011–2019. Syst Biol Reprod Med. 2022;68(3):180–9. https://doi.org/10.1080/19396368.2022.2038718.
Komorowski AS, Jain T. A review of disparities in access to infertility care and treatment outcomes among Hispanic women. Reprod Biol Endocrinol. 2022;20(1):1. https://doi.org/10.1186/s12958-021-00875-1.
Eller A, Ejzenberg D, Monteleone P, Soares JJ, Baracat EC. Vitamin D and in vitro fertilization: a systematic review. J Assist Reprod Genet. 2023. https://doi.org/10.1007/s10815-023-02767-2.
Hajhashemy Z, Foshati S, Saneei P. Relationship between abdominal obesity (based on waist circumference) and serum vitamin D levels: a systematic review and meta-analysis of epidemiologic studies. Nutr Rev. 2022;80(5):1105–17. https://doi.org/10.1093/nutrit/nuab070.
Guerrero R, Vega GL, Grundy SM, Browning JD. Ethnic differences in hepatic steatosis: an insulin resistance paradox? Hepatology. 2009;49(3):791–801. https://doi.org/10.1002/hep.22726.
Thong EP, Codner E, Laven J, Teede H. Diabetes: a metabolic and reproductive disorder in women. Lancet Diabetes Endocrinol. 2020;8(2):134–49. https://doi.org/10.1016/S2213-8587(19)30345-6.
Sharpe A, Morley LC, Tang T, Norman RJ, Balen AH. Metformin for ovulation induction (excluding gonadotrophins) in women with polycystic ovary syndrome. Cochrane Database Syst Rev. 2019;12(12):CD013505. https://doi.org/10.1002/14651858.CD013505.
Morley LC, Tang T, Yasmin E, Norman RJ, Balen AH. Insulin-sensitising drugs (metformin, rosiglitazone, pioglitazone, D-chiro-inositol) for women with polycystic ovary syndrome, oligo amenorrhoea and subfertility. Cochrane Database Syst Rev. 2017;11(11):CD003053. https://doi.org/10.1002/14651858.CD003053.pub6.
Codner E, Merino PM, Tena-Sempere M. Female reproduction and type 1 diabetes: from mechanisms to clinical findings. Hum Reprod Update. 2012;18(5):568–85. https://doi.org/10.1093/humupd/dms024.
Dyńka D, Kowalcze K, Ambrozkiewicz F, Paziewska A. Effect of the ketogenic diet on the prophylaxis and treatment of diabetes mellitus: a review of the meta-analyses and clinical trials. Nutrients. 2023;15(3). https://doi.org/10.3390/nu15030500
Gutierrez-Mariscal FM, Alcalá-Diaz JF, Quintana-Navarro GM, et al. Changes in quantity plant-based protein intake on type 2 diabetes remission in coronary heart disease patients: from the CORDIOPREV study. Eur J Nutr. 2023. https://doi.org/10.1007/s00394-022-03080-x.
Kulak D, Polotsky AJ. Should the ketogenic diet be considered for enhancing fertility? Maturitas. 2013;74(1):10–3. https://doi.org/10.1016/j.maturitas.2012.10.003.
Kim K, Yisahak SF, Nobles CJ, et al. Low intake of vegetable protein is associated with altered ovulatory function among healthy women of reproductive age. J Clin Endocrinol Metab. 2021;106(7):e2600–12. https://doi.org/10.1210/clinem/dgab179.
Cao Q, Zheng R, He R, et al. Age-specific prevalence, subtypes and risk factors of metabolic diseases in Chinese adults and the different patterns from other racial/ethnic populations. BMC Public Health. 2022;22(1):2078. https://doi.org/10.1186/s12889-022-14555-1.
Acknowledgements
We thank the staff and the participants of the NHANES study for their valuable contributions.
Funding
This work was supported by the National Natural Science Foundation of China Youth Fund (No.82104903).
Author information
Authors and Affiliations
Contributions
R Zhu collected data. HW Han organized the study and performed the statistical analysis. XZ Wang and J Jin drafted the manuscript, to which all authors contributed, and approved the final version for publication.
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. All analyses were based on data of the National Health and Nutrition Examination Survey (NHANES). The study was approved by the ethics review board of the National Center for Health Statistics. The detailed information is located on the NHANES website. Written informed consent was obtained from each participant before their inclusion on the NHANES database. Detailed information on the ethics application and written informed consent are provided on the NHANES website.
Consent to Participate
The America National Center for Health Statistics has obtained informed consent from each participant before their inclusion. Detailed information is provided on the NHANES website.
Consent for Publication
The participant has consented to the submission of the research article to the journal.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, X., Zhu, R., Han, H. et al. Body Fat Distribution and Female Infertility: a Cross-Sectional Analysis Among US Women. Reprod. Sci. 30, 3243–3252 (2023). https://doi.org/10.1007/s43032-023-01280-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-023-01280-2