Abstract
AGD is the distance measured from the anus to the genital tubercle. Recent evidence suggests that a shorter AGD, a sensitive biomarker of the prenatal hormonal environment, could be associated with higher endometriosis risk. However, studies investigating AGD in affected women are scanty. We have set up a case–control study recruiting nulliparous women (aged 18–40 years) with endometriosis between 2017 and 2018. Cases were 90 women with a surgical or with a current nonsurgical diagnosis of endometriosis (n = 45 deep infiltrating endometriosis (DIE), and n = 45 ovarian endometrioma (OMA)). Controls were 45 asymptomatic women referring for periodical gynaecological care and without a previous diagnosis of endometriosis. They were matched to cases for age and BMI. For each woman, two measures were obtained using a digital calliper: AGDAC, from the clitoral surface to the upper verge of the anus, and AGDAF, from the posterior fourchette to the upper verge of the anus. Each distance was derived from the mean of six measurements acquired from two different gynaecologists. The mean ± SD AGDAC in women with DIE, OMA and without a diagnosis of endometriosis was 76.0 ± 12.1, 76.1 ± 11.1 and 77.8 ± 11.4 mm, respectively (p = 0.55). The mean ± SD AGDAF in women with DIE, OMA and without a diagnosis of endometriosis was 22.8 ± 5.0, 21.7 ± 9.0 and 23.7 ± 7.8 mm, respectively (p = 0.38). Our study failed to find an association between AGD and the presence of endometriosis. AGD does not seem to represent a reliable indicator of the presence of endometriosis to be used in clinical practice.
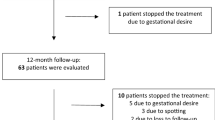
Graphical abstract



Similar content being viewed by others
References
International Working Group of AAGL EE and W, Tomassetti C, Johnson NP, et al. An international terminology for endometriosis, 2021. Hum Reprod Open. 2021;2021:16. https://doi.org/10.1093/HROPEN/HOAB029.
Vercellini P, Viganò P, Somigliana E, Fedele L. Endometriosis: pathogenesis and treatment. Nat Rev Endocrinol. 2014;10:261–75. https://doi.org/10.1038/nrendo.2013.255.
Laganà AS, Vitale SG, Granese R, et al. Clinical dynamics of Dienogest for the treatment of endometriosis: from bench to bedside. Expert Opin Drug Metab Toxicol. 2017;13:593–6. https://doi.org/10.1080/17425255.2017.1297421.
Raffaelli R, Garzon S, Baggio S, et al. Mesenteric vascular and nerve sparing surgery in laparoscopic segmental intestinal resection for deep infiltrating endometriosis. Eur J Obstet Gynecol Reprod Biol. 2018;231:214–9. https://doi.org/10.1016/J.EJOGRB.2018.10.057.
Zondervan KT, Becker CM, Koga K, et al. Endometriosis. Nat Rev Dis Prim. 2018;4:9. https://doi.org/10.1038/s41572-018-0008-5.
Signorile PG, Baldi A. Endometriosis: new concepts in the pathogenesis. Int J Biochem Cell Biol. 2010;42:778–80. https://doi.org/10.1016/j.biocel.2010.03.008.
Signorile PG, Baldi F, Bussani R, et al. Embryologic origin of endometriosis: analysis of 101 human female fetuses. J Cell Physiol. 2012;227:1653–6. https://doi.org/10.1002/jcp.22888.
Buck Louis GM, Hediger ML, Peña JB. Intrauterine exposures and risk of endometriosis. Hum Reprod. 2007;22:3232–6. https://doi.org/10.1093/humrep/dem338.
Rižner TL. Estrogen metabolism and action in endometriosis. Mol Cell Endocrinol. 2009;307:8–18. https://doi.org/10.1016/j.mce.2009.03.022.
Somigliana E, Vigano P, Abbiati A, et al. Perinatal environment and endometriosis. Gynecol Obstet Invest. 2011;72:135–40. https://doi.org/10.1159/000323531.
Wolff EF, Sun L, Hediger ML, et al. In utero exposures and endometriosis, the ENDO study. Fertil Steril. 2013;99:790–5. https://doi.org/10.1158/2326-6066.CIR-13-0034.PD-L1.
Mendiola J, Sánchez-Ferrer ML, JimCrossed Dénez-Velázquez R, et al. Endometriomas and deep infiltrating endometriosis in adulthood are strongly associated with anogenital distance, a biomarker for prenatal hormonal environment. Hum Reprod. 2016;31:2377–83. https://doi.org/10.1093/humrep/dew163.
Ferrero S, Remorgida V, Maganza C, et al. Aromatase and endometriosis: estrogens play a role. Ann N Y Acad Sci. 2014;1317:17–23. https://doi.org/10.1111/nyas.12411.
Hediger ML, Hartnett HJ, Louis GMB. Association of endometriosis with body size and figure. Fertil Steril. 2005;84:1366–74. https://doi.org/10.1016/j.fertnstert.2005.05.029.
Vannuccini S, Lazzeri L, Orlandini C, et al. Potential influence of in utero and early neonatal exposures on the later development of endometriosis. Fertil Steril. 2016;105:997–1002. https://doi.org/10.1016/j.fertnstert.2015.12.127.
Cano-Sancho G, Ploteau S, Matta K, et al. Human epidemiological evidence about the associations between exposure to organochlorine chemicals and endometriosis: systematic review and meta-analysis. Environ Int. 2019;123:209–23.
Buck Louis GM, Peterson CM, Chen Z, et al. Bisphenol A and phthalates and endometriosis: the endometriosis: natural history, diagnosis and outcomes study. Fertil Steril. 2013;100(162–9):e1-2. https://doi.org/10.1016/j.fertnstert.2013.03.026.
Laganà AS, Salmeri FM, Vitale SG, et al. Stem cell trafficking during endometriosis: may epigenetics play a pivotal role? Reprod Sci. 2018;25:978–9. https://doi.org/10.1177/1933719116687661.
Laganà AS, Salmeri FM, Ban Frangež H, et al. Evaluation of M1 and M2 macrophages in ovarian endometriomas from women affected by endometriosis at different stages of the disease. Gynecol Endocrinol. 2020;36:441–4. https://doi.org/10.1080/09513590.2019.1683821.
García-Peñarrubia P, Ruiz-Alcaraz AJ, Martínez-Esparza M, et al. Hypothetical roadmap towards endometriosis: prenatal endocrine-disrupting chemical pollutant exposure, anogenital distance, gut-genital microbiota and subclinical infections. Hum Reprod Update. 2020;26:214–46. https://doi.org/10.1093/humupd/dmz044.
Greenham LW, Greenham V. Sexing mouse pups. Lab Anim. 1977;11:181–4. https://doi.org/10.1258/002367777780936620.
Kurzrock EA, Jegatheesan P, Cunha GR, Baskin LS. Urethral development in the fetal rabbit and induction of hypospadias: a model for human development. J Urol. 2000;164:1786–92.
Swan SH, Sathyanarayana S, Barrett ES, et al. First trimester phthalate exposure and anogenital distance in newborns. Hum Reprod. 2015;30:963–72. https://doi.org/10.1093/humrep/deu363.
Bornehag CG, Carlstedt F, Jönsson BA, et al. Prenatal phthalate exposures and anogenital distance in swedish boys. Environ Health Perspect. 2015;123:101–7. https://doi.org/10.1289/ehp.1408163.
Dean A, Sharpe RM. Anogenital distance or digit length ratio as measures of fetal androgen exposure: relationship to male reproductive development and its disorders. J Clin Endocrinol Metab. 2013;98:2230–8.
Jain VG, Singal AK. Shorter anogenital distance correlates with undescended testis: a detailed genital anthropometric analysis in human newborns. Hum Reprod. 2013;28:2343–9. https://doi.org/10.1093/humrep/det286.
Sánchez-Ferrer ML, Jiménez-Velázquez R, Mendiola J, et al. Accuracy of anogenital distance and anti-Müllerian hormone in the diagnosis of endometriosis without surgery. Int J Gynecol Obstet. 2019;144:90–6. https://doi.org/10.1002/ijgo.12691.
Sánchez-Ferrer ML, Mendiola J, Jiménez-Velázquez R, et al. Investigation of anogenital distance as a diagnostic tool in endometriosis. Reprod Biomed Online. 2017;34:375–82. https://doi.org/10.1016/j.rbmo.2017.01.002.
Crestani A, Arfi A, Ploteau S, et al. Anogenital distance in adult women is a strong marker of endometriosis: results of a prospective study with laparoscopic and histological findings. Hum Reprod open. 2020;2020:hoaa023. https://doi.org/10.1093/HROPEN/HOAA023.
Buggio L, Barbara G, Dridi D, et al. Anogenital distance and gynaecological diseases: a narrative review. Ital J Obstet Gynaecol. 2020;32:200–7. https://doi.org/10.36129/jog.32.03.06.
Peters HE, Laeven CHC, Trimbos CJMA, et al. Anthropometric biomarkers for abnormal prenatal reproductive hormone exposure in women with Mayer-Rokitanksy-Küster-Hauser syndrome, polycystic ovary syndrome, and endometriosis. Fertil Steril. 2020;114:1297–305. https://doi.org/10.1016/J.FERTNSTERT.2020.06.029.
Crestani A, Abdel Wahab C, Arfi A, et al. A short anogenital distance on MRI is a marker of endometriosis. Hum Reprod Open. 2021;2021:hoab003. https://doi.org/10.1093/HROPEN/HOAB003.
Eskenazi B, Warner M, Bonsignore L, et al. Validation study of nonsurgical diagnosis of endometriosis. Fertil Steril. 2001;76:929–35.
Vercellini P, Bracco B, Mosconi P, et al. Norethindrone acetate or dienogest for the treatment of symptomatic endometriosis: a before and after study. Fertil Steril. 2016;105:734-743.e3. https://doi.org/10.1016/j.fertnstert.2015.11.016.
Vercellini P, Ottolini F, Frattaruolo MP, et al. Is shifting to a progestin worthwhile when estrogen–progestins are inefficacious for endometriosis-associated pain? Reprod Sci. 2018;25:674–82. https://doi.org/10.1177/1933719117749759.
Vercellini, P., Somigliana, E., Cortinovis, I. et al. "You can't always get what you want": from doctrine to practicability of study designs for clinical investigation in endometriosis. BMC Women's Health 15, 89. 2015. https://doi.org/10.1186/s12905-015-0248-4
Wainstock T, Shoham-Vardi I, Sheiner E, Walfisch A. Fertility and anogenital distance in women. Reprod Toxicol. 2017;73:345–9. https://doi.org/10.1016/j.reprotox.2017.07.009.
Lee D, Kim T-H, Lee H-H, et al. A pilot study of the impacts of menopause on the anogenital distance. J Menopausal Med. 2015;21:41. https://doi.org/10.6118/jmm.2015.21.1.41.
Jain VG, Goyal V, Chowdhary V, et al. Anogenital distance is determined during early gestation in humans. Hum Reprod. 2018;33:1619–27. https://doi.org/10.1093/humrep/dey265.
Domenici L, Musella A, Bracchi C, et al. Comparison of anogenital distance and correlation with vulvo-vaginal atrophy: a pilot study on premenopausal and postmenopausal women. J Menopausal Med. 2018;24:108. https://doi.org/10.6118/jmm.2018.24.2.108.
Holt VL, Weiss NS. Recommendations for the design of epidemiologic studies of endometriosis. Epidemiology. 2000;11:654–9. https://doi.org/10.1097/00001648-200011000-00007.
Chapron C, Marcellin L, Borghese B, Santulli P. Rethinking mechanisms, diagnosis and management of endometriosis. Nat Rev Endocrinol. 2019;15:666–82.
Guerriero S, Ajossa S, Orozco R, et al. Accuracy of transvaginal ultrasound for diagnosis of deep endometriosis in the rectosigmoid: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2016;47:281–9. https://doi.org/10.1002/uog.15662.
Guerriero S, Saba L, Pascual MA, et al. Transvaginal ultrasound vs magnetic resonance imaging for diagnosing deep infiltrating endometriosis: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2018;51:586–95. https://doi.org/10.1002/uog.18961.
Leonardi M, Espada M, Choi S, et al. Transvaginal ultrasound can accurately predict the American Society of Reproductive Medicine stage of endometriosis assigned at laparoscopy. J Minim Invasive Gynecol. 2020. https://doi.org/10.1016/j.jmig.2020.02.014.
Nisenblat V, Bossuyt PMM, Farquhar C, Johnson N, Hull ML. Imaging modalities for the non‐invasive diagnosis of endometriosis. Cochrane Database of Systematic Reviews 2016(2):CD009591. https://doi.org/10.1002/14651858.CD009591.pub2.
Author information
Authors and Affiliations
Contributions
L.B. contributed to the design of the study, recruitment of study participants, interpretation of the data and drafted the manuscript; P.V. and E.S. contributed to the design of the study and critical revision of the manuscript; F.O. and D.D. contributed to the recruitment of study participants; E.S, G.S. contributed to the analysis and interpretation of the data. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The questionnaire and methodology for this study were approved by the local Institutional Review Board (Comitato di Etica Milano Area B). Ethics approval number: 261_2017bis.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
Edgardo Somigliana reports personal fees from THERAMEX and MERCK-SERONO, and grants from FERRING and MERCK-SERONO. All the other authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Buggio, L., Somigliana, E., Sergenti, G. et al. Anogenital Distance and Endometriosis: Results of a Case–Control Study. Reprod. Sci. 29, 3508–3515 (2022). https://doi.org/10.1007/s43032-022-01009-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-022-01009-7