Abstracts
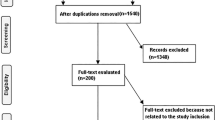
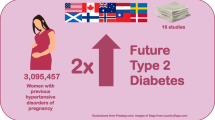
A meta-analysis was performed to evaluate the potential relationship between hypertensive disease during pregnancy and placenta accreta. A systematic literature search in OVID, Embase, Cochrane Library, PubMed, and Google scholar up to May 2021 was done, and 4 studies were found including 47,353 pregnant women at the start of the study; 4283 of them had hypertensive disease during pregnancy and 493 had placenta accreta. They were reporting relationships between hypertensive disease during pregnancy and placenta accreta. The odds ratio (OR) with 95% confidence intervals (CIs) was calculated to assess the potential relationship between hypertensive disease during pregnancy and placenta accreta using the dichotomous with a random or fixed-effect model. Hypertensive disease during pregnancy was significantly related to lower prevalence of placenta accreta (OR, 0.60; 95% CI, .38-.94, p = 0.03) compared with control (no hypertensive disease during pregnancy). When looking at the result comparing the prevalence of hypertensive disease during pregnancy in women with placenta accreta compared with control (no placenta accreta), we found that the placenta accreta was significantly related to lower prevalence of hypertensive disease during pregnancy (OR, 0.59; 95% CI, 0.38–0.94, p = 0.03) compared with control. Hypertensive disease during pregnancy may have a lower prevalence of placenta accreta. Further studies are required to validate these findings.



Similar content being viewed by others
Data Availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- OR:
-
Odds ratio
- CIs:
-
Confidence intervals
References
Dreux S, et al. Second-trimester maternal serum markers and placenta accreta. Prenat Diagn. 2012;32(10):1010–2.
Garmi G, Salim R. Epidemiology, etiology, diagnosis, and management of placenta accreta. Obstet Gynecol Int. 2012;2012:873929. https://doi.org/10.1155/2012/873929.
Orbach A, et al. Peripartum cesarean hysterectomy: critical analysis of risk factors and trends over the years. J Matern Fetal Neonatal Med. 2011;24(3):480–4.
Korejo R, et al. Emergency obstetric hysterectomy. J Pak Med Assoc. 2012;62(12):1322–5.
Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation: twenty-year analysis. Am J Obstet Gynecol. 2005;192(5):1458–61.
Khong T, et al. Pregnancies complicated by retained placenta: sex ratio and relation to pre-eclampsia. Placenta. 1998;19(8):577–80.
Gielchinsky Y, et al. Placenta accreta—summary of 10 years: a survey of 310 cases. Placenta. 2002;23(2–3):210–4.
Usta IM, et al. Placenta previa-accreta: risk factors and complications. Am J Obstet Gynecol. 2005;193(3):1045–9.
Fitzpatrick KE, et al. Incidence and risk factors for placenta accreta/increta/percreta in the UK: a national case-control study. PloS one. 2012;7(12):e52893.
Bowman ZS, et al. Risk factors for placenta accreta: a large prospective cohort. Am J Perinatol. 2014;31(09):799–804.
Eshkoli T, et al. Placenta accreta: risk factors, perinatal outcomes, and consequences for subsequent births. Am J Obstet Gynecol. 2013;208(3):219.e1-219.e7.
Stroup DF, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–12.
Gupta A, et al. Obesity is Independently Associated With Increased Risk of Hepatocellular Cancer–related Mortality. Am J Clin Oncol. 2018;41(9):874–81.
Liberati A, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34.
Collaboration C. RoB 2: A revised Cochrane risk-of-bias tool for randomized trials. Available at (Accessed December 6, 2019): bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials, 2020.
Higgins JP, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Hung T-H, et al. Risk factors for placenta accreta. Obstet Gynecol. 1999;93(4):545–50.
Sheiner E, et al. Placenta previa: obstetric risk factors and pregnancy outcome. J Matern Fetal Med. 2001;10(6):414–9.
Alves E, et al. Impact of risk factors on hypertensive disorders in pregnancy, in primiparae and multiparae. Ann Hum Biol. 2013;40(5):377–84.
Kuklina EV, Ayala C, Callaghan WM. Hypertensive disorders and severe obstetric morbidity in the United States. Obstet Gynecol. 2009;113(6):1299–306.
Tantbirojn P, Crum C, Parast M. Pathophysiology of placenta creta: the role of decidua and extravillous trophoblast. Placenta. 2008;29(7):639–45.
Fan D, Li S, Wu S, Wang W, Ye S, Xia Q, Liu L, Feng J, Wu S, Guo X, Liu Z. Prevalence of abnormally invasive placenta among deliveries in mainland China. Medicine. 2017;96(16):e6636. https://doi.org/10.1097/MD.0000000000006636.
Basta P, et al. The frequency of CD25+ CD4+ and FOXP3+ regulatory T cells in ectopic endometrium and ectopic decidua. Reprod Biol Endocrinol. 2010;8(1):1–7.
Schwede S, Alfer J, Von Rango U. Differences in regulatory T-cell and dendritic cell pattern in decidual tissue of placenta accreta/increta cases. Placenta. 2014;35(6):378–85.
Yliniemi A, et al. Combination of PAPPA, fhCGβ, AFP, PIGF, sTNFR1, and maternal characteristics in prediction of early-onset preeclampsia. Clin Med Insights Reprod Health. 2015;9:CMRH. S21865.
Desai N, et al. Elevated first trimester PAPP-A is associated with increased risk of placenta accreta. Prenat Diagn. 2014;34(2):159–62.
Lash GE, Ernerudh J. Decidual cytokines and pregnancy complications: focus on spontaneous miscarriage. J Reprod Immunol. 2015;108:83–9.
Feldman DR, et al. Phase I trial of bevacizumab plus escalated doses of sunitinib in patients with metastatic renal cell carcinoma. J Clin Oncol. 2009;27(9):1432.
McMahon K, et al. Does soluble fms-like tyrosine kinase-1 regulate placental invasion? Insight from the invasive placenta. Am J Obstet Gynecol. 2014;210(1):68.e1-68.e4.
Moustafa IO, et al. Clinical outcome associated with the use of different inhalation method with and without humidification in asthmatic mechanically ventilated patients. Pulm Pharmacol Ther. 2017;45:40–6.
Moustafa IO, et al. Lung deposition and systemic bioavailability of different aerosol devices with and without humidification in mechanically ventilated patients. Heart Lung. 2017;46(6):464–7.
Ali AMA, Abdelrahim MEA. Modeling and optimization of terbutaline emitted from a dry powder inhaler and influence on systemic bioavailability using data mining technology. J Pharm Innov. 2014;9(1):38–47.
Abdelrahim M, Assi KH, Chrystyn H. Dose emission and aerodynamic characterization of the terbutaline sulphate dose emitted from a Turbuhaler at low inhalation flow. Pharm Dev Technol. 2013;18(4):944–9.
Elgendy MO, Abdelrahim ME, Eldin RS. Potential benefit of repeated MDI inhalation technique counselling for patients with asthma. Eur J Hosp Pharm. 2015;22(6):318–22.
Szymusik I, et al. Perinatal outcome of in vitro fertilization singletons – 10 years’ experience of one center. Arch Med Sci. 2019;15(3):666–72.
Li Y, et al. Pregnancy-associated plasma protein A as a predictor of all-cause mortality and cardiovascular events in patients with chronic kidney disease: a meta-analysis of prospective studies. Arch Med Sci. 2020;16(1):8–15.
Fijałkowska A, et al. Pregnancy as a predictor of deviations from the recommended diagnostic pathway in women with suspected pulmonary embolism: ZATPOL registry data. Arch Med Sci. 2018;14(4):838–45.
Hao Y, Sun X, Wen N, Song D, Li H. Effects of n-3 polyunsaturated fatty acid supplementation on pregnancy outcomes: a systematic review and meta-analysis. Arch Med Sci. 2021. https://doi.org/10.5114/aoms/141577.
Wang W, et al. Association between hypertensive disorders complicating pregnancy and risk of placenta accreta: a meta-analysis and systematic review. Hypertens Pregnancy. 2018;37(3):168–74.
Acknowledgements
We appreciate the help of Miss Nada Mohamed A Elkamel for her help in improving the quality of our figures.
Author information
Authors and Affiliations
Contributions
(1) Conception and design: Lingli Li.
(2) Administrative support: All authors.
(3) Provision of study materials or subjects: All authors.
(4) Collection and assembly of data: Luping Liu, YuYue Xu.
(5) Data analysis and interpretation: All authors.
(6) Manuscript writing: All authors.
(7) Final approval of manuscript: All authors.
All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Li, L., Liu, L. & Xu, Y. Placenta Accreta has a Low Association with Hypertensive Disease During Pregnancy: A Systematic Review Incorporating a Network Meta-analysis. Reprod. Sci. 29, 2119–2126 (2022). https://doi.org/10.1007/s43032-022-00938-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-022-00938-7