Abstract
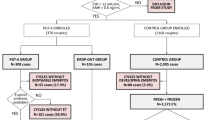
In this retrospective study, the effect of preimplantation genetic testing for aneuploidy (PGT-A) was evaluated in women younger than 38 years with a history of one prior miscarriage and embryonic chromosomal abnormalities were detected in previous products of conception (POCs). Abnormal karyotypes were detected in POCs at our center between January 2014 and December 2017. Of the women included in this analysis, 124 continued with conventional in vitro fertilization/intracytoplasmic sperm injection cycles (non-PGT-A group) and 93 chose PGT-A cycles (PGT-A group), and the pregnancy outcomes in both groups were compared. Although the clinical pregnancy rate per embryo transfer was significantly higher in the PGT-A group (67.23% vs. 51.85%, p-adj = 0.01), no between-group differences were found in the live birth rate or miscarriage rate (45.38% vs. 40.74%, p-adj = 0.59; 16.25% vs. 14.29%, p-adj = 0.15). Women in both groups had comparative cumulative live birth rates (PGT-A vs. non-PGT-A, 58.06% vs. 53.23%, p = 0.48). The main results of this study suggest that PGT-A is not associated with an increased likelihood of a live birth or a decreased rate of miscarriage among women younger than 38 years without recurrent pregnancy loss and with a history of POCs with embryonic chromosomal abnormalities.

Similar content being viewed by others
References
Somigliana E, Busnelli A, Paffoni A, Vigano P, Riccaboni A, Rubio C, et al. Cost-effectiveness of preimplantation genetic testing for aneuploidies. Fertil Steril. 2019;111(6):1169–76. https://doi.org/10.1016/j.fertnstert.2019.01.025.
Sciorio R, Tramontano L, Catt J. Preimplantation genetic diagnosis (PGD) and genetic testing for aneuploidy (PGT-A): status and future challenges. Gynecol Endocrinol. 2019;36:1–6. https://doi.org/10.1080/09513590.2019.1641194.
Vanneste E, Voet T, Le Caignec C, Ampe M, Konings P, Melotte C, et al. Chromosome instability is common in human cleavage-stage embryos. Nat Med. 2009;15(5):577–83. https://doi.org/10.1038/nm.1924.
Baart EB, Martini E, van den Berg I, Macklon NS, Galjaard RJ, Fauser BC, et al. Preimplantation genetic screening reveals a high incidence of aneuploidy and mosaicism in embryos from young women undergoing IVF. Hum Reprod. 2006;21(1):223–33. https://doi.org/10.1093/humrep/dei291.
Rubio C, Simon C, Vidal F, Rodrigo L, Pehlivan T, Remohi J, et al. Chromosomal abnormalities and embryo development in recurrent miscarriage couples. Hum Reprod. 2003;18(1):182–8. https://doi.org/10.1093/humrep/deg015.
van den Berg MM, van Maarle MC, van Wely M, Goddijn M. Genetics of early miscarriage. Biochim Biophys Acta. 2012;1822(12):1951–9. https://doi.org/10.1016/j.bbadis.2012.07.001.
Martinez MC, Mendez C, Ferro J, Nicolas M, Serra V, Landeras J. Cytogenetic analysis of early nonviable pregnancies after assisted reproduction treatment. Fertil Steril. 2010;93(1):289–92. https://doi.org/10.1016/j.fertnstert.2009.07.989.
Ljunger E, Cnattingius S, Lundin C, Anneren G. Chromosomal anomalies in first-trimester miscarriages. Acta Obstet Gynecol Scand. 2005;84(11):1103–7. https://doi.org/10.1111/j.0001-6349.2005.00882.x.
Strom CM, Ginsberg N, Applebaum M, Bozorgi N, White M, Caffarelli M, et al. Analyses of 95 first-trimester spontaneous abortions by chorionic villus sampling and karyotype. J Assist Reprod Genet. 1992;9(5):458–61. https://doi.org/10.1007/BF01204052.
Rubio C, Bellver J, Rodrigo L, Castillon G, Guillen A, Vidal C, et al. In vitro fertilization with preimplantation genetic diagnosis for aneuploidies in advanced maternal age: a randomized, controlled study. Fertil Steril. 2017;107(5):1122–9. https://doi.org/10.1016/j.fertnstert.2017.03.011.
Scott RT Jr, Upham KM, Forman EJ, Zhao T, Treff NR. Cleavage-stage biopsy significantly impairs human embryonic implantation potential while blastocyst biopsy does not: a randomized and paired clinical trial. Fertil Steril. 2013;100(3):624–30. https://doi.org/10.1016/j.fertnstert.2013.04.039.
Sato T, Sugiura-Ogasawara M, Ozawa F, Yamamoto T, Kato T, Kurahashi H, et al. Preimplantation genetic testing for aneuploidy: a comparison of live birth rates in patients with recurrent pregnancy loss due to embryonic aneuploidy or recurrent implantation failure. Hum Reprod. 2019;34:2340–8. https://doi.org/10.1093/humrep/dez229.
Ubaldi FM, Cimadomo D, Capalbo A, Vaiarelli A, Buffo L, Trabucco E, et al. Preimplantation genetic diagnosis for aneuploidy testing in women older than 44 years: a multicenter experience. Fertil Steril. 2017;107(5):1173–80. https://doi.org/10.1016/j.fertnstert.2017.03.007.
Mastenbroek S, Twisk M, van der Veen F, Repping S. Preimplantation genetic screening: a systematic review and meta-analysis of RCTs. Hum Reprod Update. 2011;17(4):454–66. https://doi.org/10.1093/humupd/dmr003.
Murphy LA, Seidler EA, Vaughan DA, Resetkova N, Penzias AS, Toth TL, et al. To test or not to test? A framework for counselling patients on preimplantation genetic testing for aneuploidy (PGT-A). Hum Reprod. 2019;34(2):268–75. https://doi.org/10.1093/humrep/dey346.
Mastenbroek S, Repping S. Preimplantation genetic screening: back to the future. Hum Reprod. 2014;29(9):1846–50. https://doi.org/10.1093/humrep/deu163.
Gleicher N, Orvieto R. Is the hypothesis of preimplantation genetic screening (PGS) still supportable? A review. J Ovarian Res. 2017;10(1):21. https://doi.org/10.1186/s13048-017-0318-3.
Practice Committees of the American Society for Reproductive M, the Society for Assisted Reproductive Technology. Electronic address Aao, Practice Committees of the American Society for Reproductive M, the Society for Assisted Reproductive T. The use of preimplantation genetic testing for aneuploidy (PGT-A): a committee opinion. Fertil Steril. 2018;109(3):429–36. https://doi.org/10.1016/j.fertnstert.2018.01.002.
Alteri A, Corti L, Sanchez AM, Rabellotti E, Papaleo E, Vigano P. Assessment of pre-implantation genetic testing for embryo aneuploidies: a SWOT analysis. Clin Genet. 2019;95(4):479–87. https://doi.org/10.1111/cge.13510.
Kang HJ, Melnick AP, Stewart JD, Xu K, Rosenwaks Z. Preimplantation genetic screening: who benefits? Fertil Steril. 2016;106(3):597–602. https://doi.org/10.1016/j.fertnstert.2016.04.027.
Chen M, Wei S, Hu J, Quan S. Can comprehensive chromosome screening technology improve IVF/ICSI outcomes? A meta-analysis. PLoS One. 2015;10(10):e0140779. https://doi.org/10.1371/journal.pone.0140779.
Natesan SA, Bladon AJ, Coskun S, Qubbaj W, Prates R, Munne S, et al. Genome-wide karyomapping accurately identifies the inheritance of single-gene defects in human preimplantation embryos in vitro. Genet Med. 2014;16(11):838–45. https://doi.org/10.1038/gim.2014.45.
Vitez SF, Forman EJ, Williams Z. Preimplantation genetic diagnosis in early pregnancy loss. Semin Perinatol. 2019;43(2):116–20. https://doi.org/10.1053/j.semperi.2018.12.009.
Sacchi L, Albani E, Cesana A, Smeraldi A, Parini V, Fabiani M, et al. Preimplantation genetic testing for aneuploidy improves clinical, gestational, and neonatal outcomes in advanced maternal age patients without compromising cumulative live-birth rate. J Assist Reprod Genet. 2019;36(12):2493–504. https://doi.org/10.1007/s10815-019-01609-4.
Simon AL, Kiehl M, Fischer E, Proctor JG, Bush MR, Givens C, et al. Pregnancy outcomes from more than 1,800 in vitro fertilization cycles with the use of 24-chromosome single-nucleotide polymorphism-based preimplantation genetic testing for aneuploidy. Fertil Steril. 2018;110(1):113–21. https://doi.org/10.1016/j.fertnstert.2018.03.026.
Maheshwari A, McLernon D, Bhattacharya S. Cumulative live birth rate: time for a consensus? Hum Reprod. 2015;30(12):2703–7. https://doi.org/10.1093/humrep/dev263.
Lintsen AM, Braat DD, Habbema JD, Kremer JA, Eijkemans MJ. Can differences in IVF success rates between centres be explained by patient characteristics and sample size? Hum Reprod. 2010;25(1):110–7. https://doi.org/10.1093/humrep/dep358.
Malizia BA, Hacker MR, Penzias AS. Cumulative live-birth rates after in vitro fertilization. N Engl J Med. 2009;360(3):236–43. https://doi.org/10.1056/NEJMoa0803072.
Suzumori N, Sugiura-Ogasawara M. Genetic factors as a cause of miscarriage. Curr Med Chem. 2010;17(29):3431–7. https://doi.org/10.2174/092986710793176302.
Acknowledgments
We thank Yan Li, Tianxiang Ni, and Caiyi Huang for their suggestions regarding this article. Special thanks are given to Jingfu Yang for assisting with clinical data collection.
Funding
This work was supported by the National Key Research and Development Program of China (2016YFC1000202, 2018YFC1002804).
Author information
Authors and Affiliations
Contributions
T.Z. and Y.Z. conceived of the study under the supervision of J.Y. and Z-J.C. T.Z. designed the study and wrote the initial manuscript. J.Z. collected the villus tissue from miscarriage samples. Y.Z. and H.L. acquired the patients’ data. W.J. conducted the genetic analyses. Q.Z. and J.L. revised the manuscript. T.Z., Y.Z., and J.Z. contributed equally to this manuscript as first authors.
Corresponding author
Ethics declarations
Research Ethics
This study protocol was approved by the Institutional Review Board (Center for Reproductive Medicine, Shandong University) on December 12, 2019.
Patient Consent
All patients provided informed consent to participate in the study before their POC samples were collected.
Conflicts of interest
None
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Tingting Zhou, Yueting Zhu and Juan Zhang should be regarded as joint first authors.
Rights and permissions
About this article
Cite this article
Zhou, T., Zhu, Y., Zhang, J. et al. Effects of PGT-A on Pregnancy Outcomes for Young Women Having One Previous Miscarriage with Genetically Abnormal Products of Conception. Reprod. Sci. 28, 3265–3271 (2021). https://doi.org/10.1007/s43032-021-00542-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00542-1