Abstract
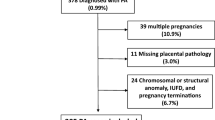
We aimed to study the association between the number of placentas with vascular malperfusion lesions in dichorionic twin pregnancies complicated by preeclampsia and the severity of the disease and pregnancy outcomes. Dichorionic twin pregnancies with preeclampsia (n = 125), from January 2007–June 2018, were reviewed. Affected placenta was defined as the presence of maternal/fetal vascular malperfusion lesions. Maternal demographics, pregnancy characteristics, and neonatal outcomes were compared between three groups: no pathological placentas, one pathological placenta, and two pathological placentas. Composite adverse neonatal outcome was defined as ≥ 1 early neonatal complication. Regression analysis models were used to recognize independent associations with the number of involved placentas. The two pathological placenta group (n = 57 pregnancies), the one pathological placenta group (n = 40 pregnancies), and the no pathological placenta group (n = 28 pregnancies) differed in terms of gestational age (GA) at delivery (p < 0.001, p = 0.008) and the rates of severe features (p = 0.028, p = 0.047). Neonates born to the two pathological placenta group (n = 114), the one pathological placenta group (n = 80), and the no pathological placenta group (n = 56) were characterized by lower birth weights (p < 0.001, p = 0.031), higher rates of small for gestational age (SGA) (p = 0.017, p = 0.748), neonatal intensive care unit admission (p = 0.004, p = 0.013), and composite adverse neonatal outcome (p < 0.001, p = 0.025). By regression analyses, the presence of two pathological placentas was found to be independently associated with severe features (aOR = 5.1), GA at delivery < 32 weeks (aOR = 2.0), SGA (aOR = 2.5), and composite adverse neonatal outcome (aOR = 2.7). In dichorionic twin pregnancies, there is an association between the presences of placental vascular malperfusion lesions in none, one, or both placentas and the development of early and severe preeclampsia, as well as with SGA and adverse neonatal outcome.

Similar content being viewed by others
References
Ananth CV, Keyes KM, Wapner RJ. Pre-eclampsia rates in the United States, 1980–2010: age-period-cohort analysis. BMJ. 2013;347:f6564.
Sibai B, Dekker G, Kupferminc M. Pre-eclampsia. Lancet. 2005;365(9461):785–99.
Bellamy L, et al. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335(7627):974.
McDonald SD, et al. Cardiovascular sequelae of preeclampsia/eclampsia: a systematic review and meta-analyses. Am Heart J. 2008;156(5):918–30.
Simmons RA. Developmental origins of adult disease. Pediatr Clin N Am. 2009;56(3):449–66 Table of Contents.
Hakim J, Senterman MK, Hakim AM. Preeclampsia is a biomarker for vascular disease in both mother and child: the need for a medical alert system. Int J Pediatr. 2013;2013:953150.
Grace T, et al. Maternal hypertensive diseases negatively affect offspring motor development. Pregnancy Hypertens. 2014;4(3):209–14.
Khong Y, Brosens I. Defective deep placentation. Best Pract Res Clin Obstet Gynaecol. 2011;25(3):301–11.
Bustamante Helfrich B, et al. Maternal vascular malperfusion of the placental bed associated with hypertensive disorders in the Boston Birth Cohort. Placenta. 2017;52:106–13.
Falco ML, et al. Placental histopathology associated with pre-eclampsia: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2017;50(3):295–301.
Kalafat E, Thilaganathan B. Cardiovascular origins of preeclampsia. Curr Opin Obstet Gynecol. 2017;29(6):383–9.
American College of, O., Gynecologists, and P. Task force on hypertension in, hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ task force on hypertension in pregnancy. Obstet Gynecol. 2013;122(5):1122–31.
Practice Bulletin No. 169. Summary: Multifetal gestations: twin, triplet, and higher-order multifetal pregnancies. Obstet Gynecol. 2016;128(4):926–8.
Wood SL, et al. Evaluation of the twin peak or lambda sign in determining chorionicity in multiple pregnancy. Obstet Gynecol. 1996;88(1):6–9.
American College of, O. and B.-O. Gynecologists Committee on Practice. ACOG Practice Bulletin No. 118: antiphospholipid syndrome. Obstet Gynecol. 2011;117(1):192–9.
American College of, O. and P. Gynecologists Women’s Health Care, ACOG Practice Bulletin No. 138. Inherited thrombophilias in pregnancy. Obstet Gynecol. 2013;122(3):706–17.
Committee on Obstetric, P. ACOG committee opinion: antenatal corticosteroid therapy for fetal maturation. Obstet Gynecol. 2002;99(5 Pt 1):871–3.
Dollberg S, et al. Birth weight standards in the live-born population in Israel. Isr Med Assoc J. 2005;7(5):311–4.
Redline RW. Classification of placental lesions. Am J Obstet Gynecol. 2015;213(4 Suppl):S21–8.
Khong TY, et al. Sampling and definitions of placental lesions: Amsterdam placental workshop group consensus statement. Arch Pathol Lab Med. 2016;140(7):698–713.
Weiner E, et al. The placental component and obstetric outcome in severe preeclampsia with and without HELLP syndrome. Placenta. 2016;47:99–104.
Pinar H, et al. Reference values for singleton and twin placental weights. Pediatr Pathol Lab Med. 1996;16(6):901–7.
Parks WT. Placental hypoxia: the lesions of maternal malperfusion. Semin Perinatol. 2015;39(1):9–19.
Brosens I, et al. The “Great Obstetrical Syndromes” are associated with disorders of deep placentation. Am J Obstet Gynecol. 2011;204(3):193–201.
Redline RW. Clinical and pathological umbilical cord abnormalities in fetal thrombotic vasculopathy. Hum Pathol. 2004;35(12):1494–8.
Redline RW, et al. Placental diagnostic criteria and clinical correlation--a workshop report. Placenta. 2005;26(Suppl A):S114–7.
Salafia CM, et al. Clinical correlations of patterns of placental pathology in preterm pre-eclampsia. Placenta. 1998;19(1):67–72.
Vinnars MT, et al. The severity of clinical manifestations in preeclampsia correlates with the amount of placental infarction. Acta Obstet Gynecol Scand. 2011;90(1):19–25.
Kovo M, et al. The placental component in early-onset and late-onset preeclampsia in relation to fetal growth restriction. Prenat Diagn. 2012;32(7):632–7.
Ogge G, et al. Placental lesions associated with maternal underperfusion are more frequent in early-onset than in late-onset preeclampsia. J Perinat Med. 2011;39(6):641–52.
Weiner E, et al. The role of placental histopathological lesions in predicting recurrence of preeclampsia. Prenat Diagn. 2016;36(10):953–60.
Mosca L, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women--2011 update: a guideline from the American Heart Association. J Am Coll Cardiol. 2011;57(12):1404–23.
White WM, et al. A history of preeclampsia is associated with a risk for coronary artery calcification 3 decades later. Am J Obstet Gynecol. 2016;214(4):519–e1–519 e8.
Heyborne KD, Porreco RP. Selective fetocide reverses preeclampsia in discordant twins. Am J Obstet Gynecol. 2004;191(2):477–80.
Hagay ZJ, et al. Single fetal demise in twin gestation resulting in the resolution of severe pre-eclampsia. Eur J Obstet Gynecol Reprod Biol. 1994;56(2):137–8.
Sarhanis P, Pugh DH. Resolution of pre-eclampsia following intrauterine death of one twin. Br J Obstet Gynaecol. 1992;99(2):159–60.
Weiner E, et al. Placental component and pregnancy outcome in singleton versus twin pregnancies complicated by preeclampsia. Fetal Diagn Ther. 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Approval for the study was obtained from the local ethics committee (decision number 0102-15-WOMC dated 6.8.2015).
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Weiner, E., Feldstein, O., Schreiber, L. et al. None, One, or Both Placentas Involved with Malperfusion Lesions in Twin Pregnancies Complicated by Preeclampsia—Does It Matter?. Reprod. Sci. 27, 845–852 (2020). https://doi.org/10.1007/s43032-019-00087-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-019-00087-4