Abstract
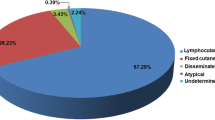
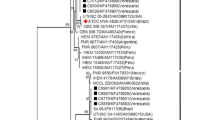
Human sporotrichosis is caused by different Sporothrix species; however, Sporothrix brasiliensis is the main species, usually related to cat transmission in urban areas. A retrospective descriptive study was conducted at the Institute of Infectology Emílio Ribas from 2010 to 2018. Demography, clinical, diagnostic, and therapeutic data were obtained from medical records. Polymerase chain reaction of the calmodulin gene was performed to identify Sporothrix species. In addition, to evaluate the spread of the disease across São Paulo metropolitan region, TerraView version 4.2.2 software was used for geocoding cases according to residence addresses. Kernell’s maps using QGIS software version 2.16.3 were constructed to determine the concentration of cases. Results: 260 cases of sporotrichosis were diagnosed between 2010 and 2018. We observed a 700% increment in the number of human cases in the 2016–2018 triennium compared with the 2013–2015 triennium. Female adults with a median age of 46 years old were the predominant infected group associated with cats’ exposition at home care, although the age range of all patients was 01 to 86 years old. The main epidemiological risk of acquiring sporotrichosis was contact with cats, reported by 96.5% of the patients. Molecular identification showed that most of the tested isolates were Sporothrix brasiliensis. Lymphocutaneous form was observed in 59.2% and fixed cutaneous form in 37.5% of the patients. Regarding treatment, itraconazole was the main drug used (94.2%) with a cure rate of 98.8%. We observed an important spread of human sporotrichosis involving cat transmission caused by Sporothrix brasiliensis in a densely populated area of São Paulo state. These results are important to alert clinicians and dermatologists about the occurrence and progression of a neglected tropical disease in an urban area and the urgent necessity to include sporotrichosis as a differential diagnosis in the clinical investigation routine.






Similar content being viewed by others
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
Orofino-Costa R, Macedo PM, Rodrigues AM, Bernardes-Engemann AR (2017) Sporotrichosis: an update on epidemiology, etiopathogenesis, laboratory and clinical therapeutics. An Bras Dermatol 92(5):606–20. https://doi.org/10.1590/abd1806-4841.2017279
de Beer ZW, Duong TA, Wingfield MJ (2016) The divorce of Sporothrix and Ophiostoma: solution to a problematic relationship. Stud Mycol 83:165–191. https://doi.org/10.1016/j.simyco.2016.07.001
Marimon R, Cano J, Gené J, Sutton DA, Kawasaki M, Guarro J (2007) Sporothrix brasiliensis, S. globosa, and S. mexicana, three new Sporothrix species of clinical interest. J Clin Microbiol 45(10):3198–206. https://doi.org/10.1128/JCM.00808-07
Zhang Y, Hagen F, Stielow B et al (2015) Phylogeography and evolutionary patterns in Sporothrix spanning more than 14 000 human and animal case reports. Persoonia 35:1–20. https://doi.org/10.3767/003158515X687416
Gremião ID, Miranda LH, Reis EG, Rodrigues AM, Pereira AS (2017) Zoonotic Epidemic of Sporotrichosis: Cat to Human Transmission. PLoS Pathog 13(1). https://doi.org/10.1371/journal.ppat.1006077
Tang MM, Tang JJ, Gill P, Chang CC, Baba R (2012) Cutaneous sporotrichosis: a six-year review of 19 cases in a tertiary referral center in Malaysia. Int J Dermatol 51(6):702–708. https://doi.org/10.1111/j.1365-4632.2011.05229.x
Han HS, Kano R (2021) Feline sporotrichosis in Asia. Braz J Microbiol 52(1):125–134. https://doi.org/10.1007/s42770-020-00274-5
Siew HH (2017) The Current Status of Feline Sporotrichosis in Malaysia. Med Mycol J 58(3):E107–E113. https://doi.org/10.3314/mmj.17.014
Poester VR, Mattei AS, Madrid IM et al (2018) Sporotrichosis in Southern Brazil, towards an epidemic? Zoonoses Public Health 65(7):815–821. https://doi.org/10.1111/zph.12504
Macêdo-Sales PA, Souto SRLS, Destefani CA, Lucena RP, Machado RLD, Pinto MR, Rodrigues AM, Lopes-Bezerra LM, Rocha EMS, Baptista ARS (2018) Domestic feline contribution in the transmission of Sporothrix in Rio de Janeiro State, Brazil: a comparison between infected and non-infected populations. BMC Vet Res. Jan 18;14(1):19. https://doi.org/10.1186/s12917-018-1340-4
Lecca LO, Paiva MT, de Oliveira CSF, et al (2020) Associated factors and spatial patterns of the epidemic sporotrichosis in a high density human populated area: A cross-sectional study from 2016 to 2018. Prev Vet Med 176 https://doi.org/10.1016/j.prevetmed.2020.104939
Gremião IDF, Rocha EMS, Montenegro H, Carneiro AJB et al (2021) Guideline for the management of feline sporotrichosis caused by Sporothrix brasiliensis and literature revision. Braz J Microbiol 52(1):107–124. https://doi.org/10.1007/s42770-020-00365-3
Cruz ILR, Freitas DFS, de Macedo PM, Gutierrez-Galhardo MC, do Valle ACF, Almeida MA, Coelho RA, Brito-Santos F, Figueiredo-Carvalho MHG, Zancopé-Oliveira RM, Almeida-Paes R (2021) Evolution of virulence-related phenotypes of Sporothrix brasiliensis isolates from patients with chronic sporotrichosis and acquired immunodeficiency syndrome. Braz J Microbiol 52(1):5–18. https://doi.org/10.1007/s42770-020-00297-y
Cruz-Choappa R, Pérez Gaete S, Rodríguez Badilla V, VieilleOyarzo P, Opazo Sanchez H (2016) Virulencia de Sporothrix globosa en modelos murinos [Virulence of Sporothrix globosa in murine models]. Rev Argent Microbiol. 48(3):196–199. https://doi.org/10.1016/j.ram.2016.04.007 (Spanish)
Fernandes GF, dos Santos PO, Rodrigues AM, Sasaki AA, Burger E, de Camargo ZP (2013) Characterization of virulence profile, protein secretion and immunogenicity of different Sporothrix schenckii sensu stricto isolates compared with S. globosa and S. brasiliensis species. Virulence 4(3):241–9. https://doi.org/10.4161/viru.23112
Castro RA, Kubitschek-Barreira PH, Teixeira PA, Sanches GF, Teixeira MM, Quintella LP, Almeida SR, Costa RO, Camargo ZP, Felipe MS, de Souza W, Lopes-Bezerra LM (2013) Differences in cell morphometry, cell wall topography and gp70 expression correlate with the virulence of Sporothrix brasiliensis clinical isolates. PLoS One 8(10):e75656. https://doi.org/10.1371/journal.pone.0075656
Falcão EMM, de Lima Filho JB, Campos DP, et al (2019) Hospitalizations and deaths related to sporotrichosis in Brazil (1992–2015). Cad Saude Publica; 35(4). https://doi.org/10.1590/0102-311X00109218
Mialski R, de Almeida JN, da Silva LH, et al (2018) Chronic Meningitis and Hydrocephalus due to Sporothrix brasiliensis in Immunocompetent Adults: A Challenging Entity. Open Forum Infect Dis 5(5). https://doi.org/10.1093/ofid/ofy081
Almeida-Paes R, de Oliveira MM, Freitas DF, do Valle AC, Zancopé-Oliveira RM, Gutierrez-Galhardo MC (2014) Sporotrichosis in Rio de Janeiro, Brazil: Sporothrix brasiliensis is associated with atypical clinical presentations. PLoS Negl Trop Dis 8(9). https://doi.org/10.1371/journal.pntd.0003094
Silva-Vergara ML, de Camargo ZP, Silva PF et al (2012) Disseminated Sporothrix brasiliensis infection with endocardial and ocular involvement in an HIV-infected patient. Am J Trop Med Hyg 86(3):477–480. https://doi.org/10.4269/ajtmh.2012.11-0441
Gremião IDF, Oliveira MME, Monteiro de Miranda LH, Saraiva Freitas DF, Pereira AS (2020) Geographic Expansion of Sporotrichosis. Brazil Emerg Infect Dis 26(3):621–624. https://doi.org/10.3201/eid2603.190803
Eudes Filho J, Santos IBD, Reis CMS et al (2020) A novel Sporothrix brasiliensis genomic variant in Midwestern Brazil: evidence for an older and wider sporotrichosis epidemic. Emerg Microbes Infect 9(1):2515–2525. https://doi.org/10.1080/22221751.2020.1847001
Caus ALO, Zanotti RL, Faccini-Martínez ÁA, Paterlini GV, Falqueto A (2019) Epidemiological and Clinical Aspects of Sporotrichosis in Espírito Santo State, Southeast Brazil: A Study of Three Decades (1982–2012). Am J Trop Med Hyg 100(3):706–713. https://doi.org/10.4269/ajtmh.18-0667
Benvegnú AM, Dallazzem LND, Chemello RML, Beber AAC, Chemello D (2020) Case series of sporotrichosis at a teaching hospital in Brazil. Rev Soc Bras Med Trop 53:e20190509. https://doi.org/10.1590/0037-8682-0509-2019
Grisolia JC, Santos LA, Coelho LML, Silva RR, de Camargo ZP, Velloso TRG, Coelho LFL, Chavasco JK, Malaquias LCC (2021) Seroepidemiological survey on sporotrichosis-infection in rural areas of the south of Minas Gerais State, Brazil. Braz J Microbiol 52(1):41–47. https://doi.org/10.1007/s42770-020-00279-0
Rossow JA, Queiroz-Telles F, Caceres DH et al (2020) A One Health Approach to Combatting Sporothrix brasiliensis Narrative Review of an Emerging Zoonotic Fungal Pathogen in South America. J Fungi (Basel) 6(4):247. https://doi.org/10.3390/jof6040247
Silva EA, Bernardi F, Mendes MCNC, et al. (2015) Surto de esporotricose em gatos – investigação e ações de controle, município de São Paulo/SP. Vol. 113. Boletim Epidemiológico Paulista, 1–16 (article in Portuguese)
Montenegro H, Rodrigues AM, Dias MA, da Silva EA, Bernardi F, de Camargo ZP (2014) Feline sporotrichosis due to Sporothrix brasiliensis: an emerging animal infection in São Paulo. Brazil BMC Vet Res 10:269. https://doi.org/10.1186/s12917-014-0269-5
Rodrigues AM, Najafzadeh MJ, de Hoog GS, de Camargo Z (2015) Rapid Identification of Emerging Human-Pathogenic Sporothrix Species with Rolling Circle Amplification. Front Microbiol 6:1385. https://doi.org/10.3389/fmicb.2015.01385
Lopes-Bezerra LM, Mora-Montes HM, Zhang Y et al (2018) Sporotrichosis between 1898 and 2017: The evolution of knowledge on a changeable disease and on emerging etiological agents. Med Mycol 56:126–143. https://doi.org/10.1093/mmy/myx103
Marques GF, Martins AL, Sousa JM, Brandão LS, Wachholz PA, Masuda PY (2015) Characterization of sporotrichosis cases treated in a dermatologic teaching unit in the state of São Paulo - Brazil, 2003–2013. An Bras Dermatol 90(2):273–275. https://doi.org/10.1590/abd1806-4841.20153447
Marques SA, Franco SR, de Camargo RM, Dias LD, Haddad Júnior V, Fabris VE (1993) Sporotrichosis of the domestic cat (Felis catus): human transmission. Rev Inst Med Trop Sao Paulo 35(4):327–30 ((article in Portuguese))
Barros MB, Schubach AO, do Valle AC et al (2004) Cat-transmitted sporotrichosis epidemic in Rio de Janeiro, Brazil: description of a series of cases. Clin Infect Dis 38(4):529–535. https://doi.org/10.1086/381200
Schubach A, Schubach TM, Barros MB, Wanke B (2005) Cat-transmitted sporotrichosis, Rio de Janeiro. Brazil Emerg Infect Dis 11(12):1952–1954. https://doi.org/10.3201/eid1112.040891
Silva MB, Costa MM, Torres CC et al (2012) Urban sporotrichosis: a neglected epidemic in Rio de Janeiro, Brazil. Cad Saude Publica 28(10):1867–80 ((article in Portuguese))
Brandolt TM, Madrid IM, Poester VR et al (2018) Human sporotrichosis: A zoonotic outbreak in southern Brazil, 2012–2017. Med Mycol. https://doi.org/10.1093/mmy/myy082
Veasey JV, Neto MFN, Ruiz LRB, Zaitz C (2021) Clinical and laboratory profile of urban sporotrichosis in a tertiary hospital in the city of São Paulo. An Bras Dermatol 96(2):245–248. https://doi.org/10.1016/j.abd.2020.07.010
Ramos-e-Silva M, Vasconcelos C, Carneiro S, Cestari T (2007) Sporotrichosis. Clin Dermatol 25(2):181–187. https://doi.org/10.1016/j.clindermatol.2006.05.006
Mahajan VK (2014) Sporotrichosis: an overview and therapeutic options. Dermatol Res Pract. https://doi.org/10.1155/2014/272376
Author information
Authors and Affiliations
Contributions
AAB contributed with conception, design, data collection and writing. LKMO contributed with data collection and patient assessment. RFC contributed with geocoding of human cases and epidemiological data. RNP contributed with histopathological analysis. GB, LMLB, and RB contributed with writing and review. VMFG, GMBDN, LPMS, and RSFX contributed with microbiology and molecular biology tests. JALL contributed with conception, design, data collection, writing and review.
All authors read and approved the final and reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The Research Ethics Committee of the Instituto de Infectologia Emílio Ribas, São Paulo, Brazil, approved this study under the protocol number 36/2018.
Consent to participate
The informed consent form was applied to the participant and, when the subject was not available, the consent was waived, and a researcher responsibility and confidentiality term were used for all cases.
Consent for publications
Not applicable for that section.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Responsible Editor: Luiz Henrique Rosa
Rights and permissions
About this article
Cite this article
Bittencourt, A.A., Oyafuso, L.K.M., Cavalin, R.F. et al. A neglected disease. Human sporotrichosis in a densely populated urban area in São Paulo, Brazil: clinical–epidemiological and therapeutic aspects. Braz J Microbiol 53, 739–748 (2022). https://doi.org/10.1007/s42770-022-00713-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42770-022-00713-5