Abstract
The wide use of antifungal agents has led to the development of resistance in the pathogenic yeast strain Candida albicans. Gain-of-function mutations in transcription factors such as Tac1p demonstrated their ability to control expression of the ABC transporter genes CDR1 and CDR2, and mediation of azole resistance. Previously, we obtained a series of azole-resistant isolates with high-level expression of CDR1 or/and CDR2, and identified the novel H741D mutation in Tac1p. In the present study, the TAC1 alleles from isolate C13 were introduced into tac1Δ/Δ mutant. The H741D change was seen in TAC1C13 in addition to several other amino acid differences. Hyperactive alleles TAC1C13 exhibited higher minimum inhibitory concentrations (MICs) of fluconazole and itraconazole than that observed in SN152 containing the wild-type TAC1 allele. And alleles TAC1C13 conferred constitutively high levels of Cdr1p and Cdr2p. Moreover, the importance of H741D in conferring hyperactivity to TAC1 was also confirmed by site-directed mutagenesis. Compared with SN152, the presence of H741D resulted in > 2-fold increase in CDR1 and CDR2 gene and protein expression, > 4-fold increase in fluconazole and itraconazole MICs and higher rates of Rhodamine 6G efflux by 43.24%.
Similar content being viewed by others
Introduction
Opportunistic fungal infections are an increasing threat to human health, especially in immunocompromised patients suffering from AIDs, cancer, acute leukaemia, burns and gastrointestinal disease, and in individuals following bone marrow or organ transplantation, and premature birth [1]. Candida albicans is a major pathogen accounting for approximately 50–60% of candidiasis infections [2, 3]. Antifungal drug resistance is less common in C. albicans but has been reported with long-term treatment or antifungal prophylaxis. Widespread acquired azole resistance was frequently described in patients with recurrent oropharyngeal candidiasis in patients with uncontrolled human immunodeficiency virus infection or with recurrent vaginal candidiasis in women [4].
In C. albicans, reduced intracellular accumulation of azole antifungal drugs due to rapid efflux by multidrug transporters is one prominent mechanism of azole resistance [5]. At least two families of multidrug transporters are involved in resistance to azoles, the ATP-binding cassette (ABC) transporter family and the major facilitator superfamily (MFS) [6]. The genome of C. albicans encodes 28 ABC and 95 MFS transporter proteins [7]. However, only the ABC transporters CaCdr1p and CaCdr2p (Candida drug resistance) and the MFS transporter CaMdr1p (C. albicans multidrug resistance 1) are known to be primary mediators of drug export in resistant strains [8] .
ABC transporters are of greater clinical significance than MFS proteins [9]. In C. albicans isolates, CDR1 and CDR2 play an important role in azole resistance, and deletion of either gene results in increased susceptibility to azoles [10]. Upregulation of CDR1 and CDR2 has been ascribed to amino acid substitutions in the Zn2-Cys6 transcription factor Tac1p. Tac1p binds to cis-acting drug-responsive elements (DRE), and there are two CGG triplets present in the promoters of these genes through which their expression is regulated. In C. albicans azole-resistant clinical isolates, TAC1 hyperactive alleles have been observed that contribute to constitutive overexpression of CDR genes [11]. To date, at least 39 hyperactive alleles harbouring 16 different gain-of-function (GOF) mutations at 12 distinct positions have been identified by large-scale sequencing of TAC1 alleles from C. albicans clinical isolates [12]. GOF mutations in Tac1p, such as N997D, T225A, N972D, A736V, R693K and G980E, were demonstrated to cause constitutive Tac1p activity, resulting in the overexpression of both CDR genes and azole resistance in these clinical C. albicans isolates [13]. In a previous study, we collected a selection of azole-resistant isolates and observed that CDR1 or/and CDR2 genes were upregulated [14]. However, the MDR1 gene was not overexpressed (unpublished data). Genome searches revealed that the Tac1p gene contained the novel H741D mutation in two azole-resistant isolates, suggesting it is a probable GOF mutation. In another recent study [15], several new amino acid substitutions were detected in the TAC1 gene of azole-resistant strains, and S264P (located between the DNA-binding domain and the Middle Homology Region, MHR), similar with T225A, might represent additional novel GOF mutations.
To elucidate the contribution of these mutations, site-directed mutagenesis of TAC1 was performed to recreate these mutations for expression in tac1Δ/Δ derivatives, and antifungal susceptibility, CDR1/CDR2 mRNA transcript level and Cdr1p/Cdr2p protein were investigated.
Materials and methods
Strains and culture conditions
Clinical and constructed C. albicans strains used in this study are listed in Table 1. All strains were stored as frozen stocks in 25% glycerol at − 80 °C and were routinely grown in YPD medium (1% yeast extract, 2% peptone, 2% glucose) at 30 °C, with 1.5% agar added for growth on solid media. Synthetic Dropout Media plates lacking histidine, leucine or arginine were incubated at 30 °C for 3 days for selection of His+, Leu+ or Arg+ transformants. Escherichia coli DH5a and DMT Chemically Competent cells (TransGen Biotech, Beijing, China) in this study were used to propagate plasmids and generate site-directed mutation strains. Luria-Bertani (LB) broth or LB solid media supplemented with 50 μg/mL kanamycin or 100 μg/mL ampicillin as required was used for growth of these strains [14].
Plasmid and strain construction
Deletion of the TAC1 gene in the parental strain SN152 was carried out as described by Noble and Johnson [16] using PCR-based homologous recombination, resulting in the tac1Δ/Δ mutant JY16. Auxotrophic markers for histidine and leucine were derived from plasmids pSN40 and pSN52, respectively. To evaluate the contribution of the wild-type and mutated TAC1 gene, a set of pCPC20 plasmids were constructed (listed in Table 2). High-fidelity amplification of the full-length TAC1 open reading frame (ORF) in wild-type SC5314 and clinical C. albicans resistant isolates C16 and C13 was performed with primers TAC1-F/-R, and the product linked to the amplified backbone of pCP20 with primers CP19/CP28 using a ClonExpress One-step Cloning Kit (Vazyme Biotech, Nanjing, China) to create plasmids pJY1, pJY2 and pJY3, respectively. Plasmids containing the point mutations TAC1S264P, TAC1A736V and TAC1H741D were constructed using site-directed mutagenesis to generate pJY11, pJY12 and pJY14, respectively, from plasmid pJY1. These plasmids, together with pCP20, were linearized by amplifying with primers CP22/CP23 to facilitate integration at the JY16 ADE2 gene locus, generating strains JY11, JY12, JY14 and JY17. C. albicans strains were transformed using the classical lithium acetate transfection method. To further test the role of TAC1 alleles identified in isolates related to azole resistance, the complementary experiment in which the TAC1 ORF of drug-resistant strains was replaced by C16V736A or C13D741H was also performed. All constructs were verified by PCR analysis and double-direction sequencing using an ABI 3730 sequencer (ABI). Primers used for strain construction are listed in Supplementary Table S2.
Spot and microtiter plate assays
Strains and transfectants were cultivated twice at 35 °C in YPD solid media, and one colony was resuspended in sterile saline solution to a density of 1–5 × 106 CFU/mL. The microtiter plate assay was performed according to the standards of the Clinical and Laboratory Standards Institute (CLSI) M27-S4 [17]. The minimum inhibitory concentration (MIC) of fluconazole (FLC, ≥ 8 mg/L), itraconazole (ITC, ≥ 1 mg/L) and voriconazole (VRC, ≥ 1 mg/L) for resistant isolates was determined for 24–48 h at 35 °C. Meanwhile, spot assays were implemented using a series of 10-fold serial dilutions of yeast suspension and spotting 2 μL of each dilution onto YPD plates with and without fluconazole (5 μg/mL) or itraconazole (2.5 μg/mL) and incubating at 35 °C for 48 h.
Rhodamine 6G efflux
The function of the transporters was measured by the flow cytometric rhodamine 6G (R6G) efflux assay according to the method described previously [18]. Briefly, C. albicans cells were grown overnight at 30 °C to a density of 5 × 107 cells/mL in YPD. Cells were centrifuged at 3000×g for 5 min and washed three times with PBS. Cells were then incubated in PBS for 4 h at 30 °C under continuous shaking (200 rpm) to deprive them of energy. Rhodamine 6G (10 μM) was added and cells were incubated for 2 h at 30 °C. Fluorescence uptake was measured immediately using a Beckman Coulter Epics XL FACScan flow cytometer at 535 nm. Samples of cells (2.5 × 106) from the original culture were washed with PBS and resuspended in 1 mL PBS or 1 mL PBS containing 2 mM glucose. Active efflux was evaluated by measuring the fluorescence of cells following a 30-min incubation at 30 °C with or without glucose under constant agitation (200 rpm). Each experiment was performed in triplicate.
Quantitative real-time RT-PCR
RNA was extracted from mid-log exponential phase cultures grown in YPD medium incubated at 30 °C with shaking at 200 rpm using the Yeast RNAiso reagent kit (TaKaRa, Tokyo, Japan) according to the manufacturer’s recommendations. Total RNA was reverse-transcribed to cDNA using the PrimeScript RT reagent kit (TaKaRa, Tokyo, Japan). RNA expression levels were determined for CDR1 and CDR2 by quantitative RT-PCR analysis performed on a 7300 real-time PCR System (Applied Biosystems, Shanghai, China) with the SYBR Premix Ex Taq Kit (TaKaRa) using previously described conditions [18]. Each sample was processed in triplicate. Gene expression levels in resistant strains and transfectants relative to those in the SN152 strain were determined using the 2-ΔΔCT method, where ΔΔCT [test gene] = ΔCt [test gene of resistant isolate or transfectant] − ΔCt [test gene of the SN152 strain], and ΔCt [test gene] = Ct [test gene] − Ct[18S].
Western blot analysis
The recombinant Cdr1p and Cdr2p protein fragments were generated by PCR with two sets of primers (CDR1-1 and CDR1-2, CDR2-1 and CDR2-2), using C. albicans genomic DNA as a template. The PCR fragments were subcloned using BamH1 and Xho1 restriction sites into the same sites of pet-28a with 6 × His affinity tag. The recombinant protein fragments were purified by Ni-sepharose, and analyzed by electroeluting it from a 12% SDS polyacrylamide gel. Primers used for the amplification of recombinant protein fragments are listed in Table S2.
Six weeks old Female BALB/c mice were immunized subcutaneously with 50 μg Cdr1p or Cdr2p protein fragments in an emulsion of 0.5 mL complete Freund’s adjuvant per mouse, respectively. Mice were boosted again with the same dose of protein fragments in incomplete Freund’s adjuvant interval of 2 weeks. Four days after the final immunization by spleen injection, the mice were sacrificed, and splencytes were harvested. Hybridoma cells were obtained by fusion in polyethylene glycol between sp2/0 cells and splencytes at a 1:5 ratio; clones were selected by enzyme-linked immunosorbent assay (ELISA) and Western blotting. The monoclonal antibody cells were obtained by limiting dilution. The monoclonal antibody was prepared in mice ascites and purified by a protein G column.
The protein was extracted by T-PERTM Tissue Protein Extraction Reagent (Thermo Pierce, code 78510). Strains were homogenized in T-PER Reagent with Halt Protease and Phosphatase Inhibitor Cocktail (Thermo Pierce, code 78440) on ice and centrifuged at 10,000×g for 15 min at 4 °C (5 min each time). The resulting supernatants were collected for protein concentration measurement. Ten micrograms of protein was loaded in separate lanes of a SDS-PAGE gel with 10% separated gel and 5%concentrated gel, and electrophoretically separated in 80 V and 60 V, respectively for about 2 h. The gels were then washed for 30 min in 20 mM Tris-Glycine containing 5% methanol, and the proteins in the gels were blotted onto a polyvinylidene fluoride membrane (Millipore, code: IPVH00010) in 100 V for 2 h. Blotted membranes were incubated in T-TBS containing 5% BSA for 1 h, and then in anti-Cdr1p and anti-Cdr2p antibody diluted 1:800 with T-TBS containing 3% BSA for 1 h. After washing in T-TBS, the membranes were incubated with Goat anti-Mouse IgG (H+L) Secondary antibody (Thermo Pierce, code: 31160) diluted 1:5000 at 25 °C for 1 h. Then, the membranes were washed and incubated with HRP conjugated Rabbit ANTI-Goat (Pierce, code: 31402) diluted 1:5000 at 25 °C for 1 h, after which the bands were visualized by SuperSignal® West Dura Extended Duration Substrate (Thermo Pierce, code: 34075). The expression of β-actin was used as control. Anti-β-actin antibody (HuaAn, Biotechnology Co. China) was diluted 1:10000, and the same detection methods were used as above. And fluphenazine was an inducer to clarify that the hyperactive allele caused constitutively high expression of CDR1 and CDR2.
Statistical analysis
Data were analyzed by IBM SPSS statistics version 22. Statistical significance was determined using Student’s t test. Statistical significance was determined as P < 0.05.
Results
TAC1 mutations contribute to decreased azole susceptibility
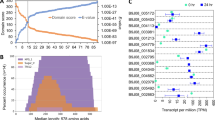
In an attempt to explicate the role of Tac1p in azole-resistant strains, the mutated TAC1 alleles from strains C13 and C16 were introduced into a derivative of the SN152 strain from which the endogenous TAC1 alleles had been deleted (strains TAC1C13 or JY3, and TAC1C16 or JY2). Meanwhile, C. albicans strain JY1 expressing the wild-type TAC1 allele (strain TAC1SC5314) and strain JY17 containing empty vector (strain TAC1empty vector) were also constructed and compared. To further assess the contribution of each of the missense mutations found in the fluconazole-resistant isolates, strains with each of the three-point mutations (strains TAC1S264P or JY11, TAC1A736V or JY12 and TAC1 H741D or JY14) were established by site-directed mutagenesis of the wild-type TAC1 allele. The fluconazole and itraconazole susceptibility of the transformants was tested using broth microdilution reference and spotting assay methods (Fig. 1).
Fluconazole and itraconazole susceptibility of Candida albicans expressing a mutated TAC1 gene. Spotting assays were performed with serial ten-fold dilutions of overnight cultures on YPD (yeast extract-peptone-glucose) medium with or without 5 μg/mL fluconazole and 2.5 μg/mL itraconazole. Plates were incubated for 48 h at 35 °C. Minimum inhibitory concentrations (MICs) of fluconazole and itraconazole were determined using the broth microdilution method according to the guidelines of the Clinical and Laboratory Standards Institute (CLSI)
Disruption of TAC1 alleles in SC5314 (JY16, tac1Δ/Δ mutant) increased fluconazole and itraconazole susceptibility, and re-introduction of the original wild-type TAC1 allele coupled with expression from the ADH1 promoter only conferred a moderate increase in resistance to FLC compared with SN152. TAC1 alleles from strains C16 and C13 conferred higher fluconazole and itraconazole resistance than strains containing the wild-type and the empty vector, and also the S264P, A736V and H741D site-directed mutants. Compared with wild-type alleles, all mutated alleles displayed 4-fold increase in resistance to fluconazole, with MICs ranging from 1 to 4 μg/mL, and a 4- to 8-fold increase in resistance to itraconazole, with MICs ranging from 0.125 to 0.5–1.0 μg/mL (Fig. 1).
TAC1 mutations contribute to constitutive overexpression of CDR1 and CDR2, and stronger efflux pump activity
The mutated TAC1 alleles from C16, C13, TAC1S264P, TAC1A736V and TAC1H741D resulted in at least a 2-fold increase in CDR1 and CDR2 expression compared with the wild-type TAC1 allele from SN152 (Fig. 2a and b). And Western blot also showed the similar data (Fig. 3). Wide-type TAC1 allele did not express high levels of Cdr1p and Cdr2p under normal growth conditions, which are comparable with levels seen in SN152 (Fig. 3). And the TAC1C16 and TAC1C13 alleles were considered to be hyperactive alleles. They conferred constitutively high levels of Cdr1p and Cdr2p under normal growth conditions and exposure of these two allele strains to fluphenazine led to higher Cdr1p and Cdr2p levels. Moreover, the presence of His741 and Ser264 in the modified alleles also resulted in constitutive high levels of Cdr1p and Cdr2p. Meanwhile, the mutated TAC1 alleles from C16, C13, TAC1S264P, TAC1A736V,and TAC1H741D also exhibited higher 6G efflux than SN152. Upon adding glucose, the mean fluorescence intensity clearly declined, and was 2.51- to 6.63-fold higher than that of SN152, and the efflux rates of SN152, transformants with C16, C13, TAC1S264P, TAC1A736V and TAC1H741D, were 6.52%, 17.12%, 17.60%, 16.38%, 37.7% and 43.24%, respectively (Fig. 4).
Fold changes in the expression levels of a CDR1 and b CDR2 in the laboratory-constructed Candida albicans containing mutated TAC1 genes relative to the value of C. albicans wild-type strain SN152. Compared with that in SN152, five strains (TAC1C16, TAC1A736V, TAC1S264P, TAC1C13 and TAC1H741D) shown in black bars increased the expression of CDR1 and CDR2 by 2.04-fold and 2.30-fold, 3.24-fold and 2.99-fold, 2.10-fold and 2.67-fold, 2.74-fold and 2.48-fold and 2.01-fold and 4.94-fold, respectively (P < 0.05). Each sample was processed in triplicate. Error bars show the standard deviation of the mean
Immunodetection of Cdr1p and Cdr2p in tac1Δ/Δ mutant and TAC1 revertant strains with different TAC1 alleles. Protein extracts of each strain were separated on SDS-10% polyacrylamide gels and immunoblotted with mouse monoclonal anti-Cdr1p and anti-Cdr2p as described in Materials and methods. The protein of strains is extracted after incubating with(+) or without(−) fluphenazine(10 mg/L) for 6 h
Fluorescence intensity of Rhodamine 6G efflux in the laboratory-constructed Candida albicans containing mutated TAC1 genes relative to that of C. albicans wild-type strain SN152. After incubation in the presence of glucose, the R6G efflux of TAC1A736V and TAC1H741D was significantly higher than that of other strains (P < 0.05). Each sample was processed in triplicate. Error bars show the standard deviation of the mean
Complementary experiment displayed similar resistant mechanisms
Furthermore, the complementary experiment in which the C16 A736V and C13 H741D alleles present in the drug-resistant strains were replaced by C16 V736A and C13 D741H was also performed (Figs. 2, 3 and 4). TAC1 activity profiles for these complementary alleles were similar to those observed for the wild-type strain. The susceptibility of recombinant strain C16 V736A and C13 D741H reverted to the same level as SN152 (Fig. 1). CDR1 and CDR2 mRNA and protein expression levels were similar to those of the wild-type strain, as was the fluorescence intensity of the complementary alleles from C16 V736A C13 D741H, demonstrating that the A736V and H741D mutates did indeed confer TAC1 gene hyperactivity, upregulation of CDR1 and CDR2 and increased levels of azole resistance.
Discussion
The impact of fungal infections on human health is attracting increasing attention worldwide. Among the most deadly fungal pathogens are C. albicans, Cryptococcus neoformans and Aspergillus fumigatus, with C. albicans reigning as the most prevalent invasive fungal pathogen of humans [19]. Currently, there are three major classes of antifungals in clinical use for the treatment of fungal infections in humans: the polyenes, the azoles and the echinocandins. Resistance to azoles is far more prevalent, perhaps as a consequence of their fungistatic activity, which exerts strong selection for resistance on fungal populations that survive drug exposure.
Several mechanisms that contribute to resistance to azole antifungal compounds have been elucidated in C. albicans [15], including (i) reduced accumulation of the compound within the fungal cell, (ii) alteration of the ergosterol biosynthetic pathway to prevent formation of fungistatic sterols and (iii) alteration in the target enzyme resulting in reduced affinity for the azole antifungal compound.
Some advancement in our understanding of the mechanisms that upregulate multidrug-resistant ABC transporters has been achieved. Using a Renilla luciferase reporter system fused to CDR1 and CDR2 promoters from an azole-susceptible strain, De Micheli et al. [20] showed that expression is constitutively upregulated in an azole-resistant strain. The authors further demonstrated that the DRE element in the promoter of the CDR genes was involved not only in their transient upregulation in response to inducers but also in their constitutive high expression in azole-resistant clinical isolates. There are two CGG triplets present in the CDR- genes, and Coste et al. [11] discovered a set of Zn2-Cys6 finger proteins by searching the entire C. albicans and demonstrated that one (Tac1p) is a positive regulator of both CDR1 and CDR2 by disrupting TAC1 alleles. Several researches have since verified that single point mutations leading to single amino acid substitutions confer hyperactivity to TAC1, and these GOF mutations are responsible for upregulation of CDR1 and CDR2 [12]. Most of the identified GOF mutations are located in the C-terminal portion of TAC1, corresponding to a putative transcriptional activation domain, while the remaining mutations are situated in the MHR and the N-terminal portion of the protein which have no known functions [12].
In one previous study, we collected a series of azole-resistant clinical C. albicans isolates and explored their azole resistance mechanisms [14]. We observed that CDR1 and CDR2 genes were upregulated, and also detected missense mutations in TAC1. We found six isolates containing the A736V mutation, two containing the H741D mutation, and two containing the R693K in TAC1. A736V and R693K were confirmed as GOF mutations in previous research [13, 21]. The newly identified H741D mutation is located in a putative transcriptional activation domain, similar to A736V and R693K, and could therefore be a novel GOF mutation. In this study, we aimed to verify this hypothesis and also elucidate the role of the S264P mutation in mediating resistance to azole agents.
By reintroducing the mutated TAC1 allele from C13 containing the H741D mutation and another seven amino acid changes, which were also identified in fluconazole-susceptible clinical isolates of C. albicans, the transfectant exhibited reduced azole susceptibility, higher 6G efflux and increased CDR1 and CDR2 mRNA and protein expression, as did the mutated TAC1 allele from C16 containing the A736V mutation. When the H741D or A736V amino acid substitutions were reversed, the strains reverted to the phenotype of the SN152 parent strain. Furthermore, mutated strains were generated with single point mutations. Compared with that in SN152, all three mutated TAC1 alleles (TAC1S264P, TAC1A736V and TAC1H741D) conferred the same degree of increase in the MIC of fluconazole by 4-fold. And TAC1A736V showed the highest increase in expression of CDR1 mRNA by 3.24-fold and TAC1H741D displayed the highest increase in expression of CDR2 mRNA by 4.94-fold. After incubation in the presence of glucose, the R6G efflux rates of TAC1A736V and TAC1H741D displayed 37.7% and 43.24%, respectively, significantly higher than that of TAC1S264P (16.38%). These results indicated the role of H741D allele causing fluconazole resistance might be equivalent to that of A736V allele.
In summary, the H741D and S264P mutations in Tac1p are associated with increased antifungal drug resistance by causing constitutively high expression of the ABC transporters CDR1 and CDR2. With the identification of increasing numbers of GOF mutations in hyperactive TAC1 alleles in clinical isolates, it will be possible to identify regions that are critical for the transcriptional activation of this protein.
Change history
13 August 2020
Unfortunately, an error occurred in the author affiliations.
References
Geehan SMD, George J, Alangaden MD (2016) Nosocomial fungal infections: epidemiology, infection control, and prevention. Infect Dis Clin N Am 30(4):1023–1052
Guinea J (2014) Global trends in the distribution of Candida species causing candidemia. Clin Microbiol Infect 20(Suppl 6):5–10
Lockhart SR (2014) Current epidemiology of Candida infection. Clin Microbiol Newsl 36(17):131–136
Arendrup MC, Patterson TF (2017) Multidrug-resistant Candida: epidemiology, molecular mechanisms, and treatment. J Infect Dis 216(suppl_3):S445–S451
Morschhauser J (2002) The genetic basis of fluconazole resistance development in Candida albicans. Biochim Biophys Acta 1587(2–3):240–248
Morio F, Loge C, Besse B, Hennequin C, Le Pape P (2010) Screening for amino acid substantiation in the Candida albicans Erg11 protein of azole-susceptible andazole-resistant clinical isolates: new substitutions and a review of the literature. Diagn Microbiol Infect Dis 66:373–384
Prasad R, Sharma M, Rawal MK (2011) Functionally relevant residues of Cdr1p: a multidrug ABC transporter of human pathogenic Candida albicans. J Amino Acids 2011:531412
Dunkel N, Blass J, Rogers PD, Morschhäuser J (2008a) Mutations in the multidrug resistance regulator MRR1, followed by loss of heterozygosity, are the main causeof MDR1 overexpression in fluconazole-resistant Candida albicans strains. Mol Microbiol 69(4):827–840
Cannon RD, Lamping E, Holmes AR, Niimi K, Baret PV, Keniya MV, Tanabe K, Niimi M, Goffeau A, Monk BC (2009) Efflux-mediated antifungal drug resistance. Clin Microbiol Rev 22(2):291–321
Sanglard D, Ischer F, Monod M, Bille J (1997) Cloning of Candida albicans genes conferring resistance to azole antifungal agents: characterization of CDR2, a new multidrug ABC transporter gene. Microbiology 143(Pt 2):405–416
Coste AT, Karababa M, Ischer F, Bille J, Sanglard D (2004) TAC1, transcriptional activator of CDR genes, is a new transcription factor involved in the regulation of Candida albicans ABC transporters CDR1 and CDR2. Eukaryot Cell 3(6):1639–1652
Morschhauser J (2010) Regulation of multidrug resistance in pathogenic fungi. Fungal Genet Biol 47(2):94–106
Coste A, Turner V, Ischer F, Morschhauser J, Forche A, Selmecki A, Beman J, Bille J, Sanglard D (2006) A mutation in Tac1p, a transcription factor regulating CDR1 and CDR2, is coupled with loss of heterozygosity at chromosome 5 to mediate antifungal resistance in Candida albicans. Genetics 172(4):2139–2156
Wang Y, Liu JY, Shi C, Li WJ, Zhao Y, Yan L, Xiang MJ (2015) Mutations in transcription factor Mrr2p contribute to fluconazole resistance in clinical isolates of Candida albicans. Int J Antimicrob Agents 46(5):552–559
Morio F, Pagniez F, Besse M, Gay-andrieu F, Miegeville M, Le Pape P (2013) Deciphering azole resistance mechanisms with a focus on transcription factor-encoding genes TAC1, MRR1 and UPC2 in a set of fluconazole-resistant clinical isolates of Candida albicans. Int J Antimicrob Agents 42(5):410–415
Noble SM, Johnson AD (2005) Strains and strategies for large-scale gene deletion studies of the diploid human fungal pathogen Candida albicans. Eukaryot Cell 4(2):298–309
CLSI (2012) Reference method for broth dilution antifungal susceptibility testing of yeasts. 4th Informational Supplement, CLSI Document M27-S4, Clinical and Laboratory Standards Institute, Wayne, PA
Li WJ, Liu JY, Shi C, Zhao Y, Meng LN, Wu F, Xiang MJ (2019) FLO8 deletion leads to azole resistance by upregulating CDR1 and CDR2 in Candida albicans. Res Microbiol 170(6–7):272–279
Xie JL, Polvi EJ, Shekhar-Guturja T, Cowen LE (2014) Elucidating drug resistance in human fungal pathogens. Future Microbiol 9(4):523–542
de Micheli M, Bille J, Schueller C, Sanglard D (2002) A common drug-responsive element mediates the upregulation of the Candida albicans ABC transporters CDR1 and CDR2, two genes involved in antifungal drug resistance. Mol Microbiol 43(5):1197–1214
Coste AT, Crittin J, Bauser C, Rohde B, Sanglard D (2009) Functional analysis of cis- and trans-acting elements of the Candida albicans CDR2 promoter with a novel promoter reporter system. Eukaryot Cell 8(8):1250–1267
Funding
This work was financed by grants from the Program of National Natural Science Fund Project [#81871706], the Program of Shanghai Municipal Commission of Health and Family Planning [#201840227 and #201740069], the Program of Shanghai Natural Science Foundation [#15ZR1426900], the Program of Shanghai Key Specialty [#ZK2012A21] and Program of Shanghai Municipal Huangpu District Commission of Health and Family Planning [#HKM201702].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Responsible Editor: Rosana Puccia.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 21 kb)
Rights and permissions
About this article
Cite this article
Liu, JY., Wei, B., Wang, Y. et al. The H741D mutation in Tac1p contributes to the upregulation of CDR1 and CDR2 expression in Candida albicans. Braz J Microbiol 51, 1553–1561 (2020). https://doi.org/10.1007/s42770-020-00336-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42770-020-00336-8