Abstract
The severity of SARS-CoV-2 virus infection is mainly related to its respiratory complications. However, it can also lead to a large variety of thromboembolic events. Symptoms may include headache, fever, and neurological disorders. Since 2020, the clinical presentation of COVID-19 infection has become increasingly varied, leading in some cases to complex symptom associations, including numerous neurological symptoms. SARS-CoV-2 may lead to neurotropism which could reach the central nervous system and all cranial nerves. Cavernous sinus thrombosis is a rare condition and may occur as a complication of ear, nose, and throat (ENT) or facial infections. A 73-year-old man without personal or family history of thrombosis was referred to the emergency room for a sudden appearance of diplopia and ptosis, 3 days after testing positive for COVID-19 infection. An initial head CT-scan found no signs of stroke. He underwent a cerebral MRI 7 days later, which revealed a thrombosis of his right cavernous sinus. A brain CT scan 7 days later showed regression of the thrombosis with complete recanalization of the cavernous sinus. This was accompanied by a complete regression of diplopia and fever. He was discharged from the hospital 10 days after hospital admission. In this case report, we describe a rare event of cavernous thrombophlebitis following a COVID-19 infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
SARS-CoV-2 infection has been described in multiples studies as a factor which can favor thrombotic events, such as pulmonary embolism, venous thrombosis of the lower limbs, and stroke [1]. Pathophysiological mechanisms may include cytokine storm that precipitates the onset of systemic inflammatory response syndrome and thrombotic processes [1] . Cavernous sinus thrombosis (CST) is a very rare condition, which is mostly of septic origin and usually revealed by symptoms including headaches, fever, and ophthalmological signs.
We here describe the case of a 73-year-old patient who presented to the emergency department with fever and diplopia. He tested positive for an Omicron variant COVID-19 infection. A CT scan showed no stroke. A few days later, he underwent a cerebral MRI, which revealed a CST and thrombosis of the ophthalmic vein, explaining his diplopia. Within 10 days of beginning anticoagulant treatment, the patient’s condition had improved, and he was discharged from the hospital. The rationale of this article is to provide a case report demonstrating the rare event of CST following COVID-19 infection. Oral and written consent was obtained.
Case Report
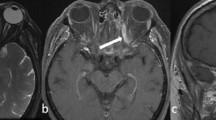
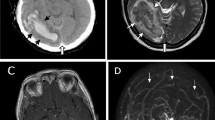
A 73-year-old patient came to the emergency room and reported having fever (39 °C) and chills over the previous 5 days and diplopia for 2 days before arriving at the hospital. His medical history includes a myocardial infarction 7 years prior to the emergency room visit (treated with aspirin and no anticoagulant) and high blood pressure treated with beta-blockers and angiotensin 2 receptor blockers. He has no personal or family history of thrombosis or cancer. He had tested positive for COVID-19 3 days before by polymerase chain reaction (PCR) with a nasal swab. Clinical examination showed hemodynamic stability with an elevated blood pressure of 200/87 mmHg, heart rate of 57 bpm, venous oxygen saturation of 98% when breathing room air, and normal blood sugar. His neuro-ophthalmological examination revealed a right ptosis with an adduction defect of the right eye, which was also found during gaze convergence. There were no sensory or motor deficits and no facial paralysis. He had no significant biological abnormalities, including no ionic disorders or inflammatory syndromes. A brain CT scan was performed, which did not reveal any signs of stroke. He was hospitalized in the COVID medical ward and underwent a cerebral MRI 7 days later, which revealed a venous thrombosis of the right cavernous sinus and the ophthalmic vein (Fig. 1). Following discovery of the venous thrombosis, the patient underwent a clinical broad check-up including a normal ear, nose, and throat (ENT) assessment, which revealed no underlying infection, a normal clinical examination, and no biological abnormality (in particular CRP = 14.3 mg/L). The thrombophilia workup was within normal limits (white blood cells and PTT without abnormality, PT = 79%, PLT: 135 G/L, fibrinogen: 2,8 g/L, protein S discreetly lowered to 56%). A thoracic-abdominal-pelvic CT scan did not reveal any underlying tumoral process or deep infection. A treatment by unfractionated heparin 300 UI/kg using a syringe driver at speed 1.7 was administered (anti-Xa target dose 0,3–0,5). After 24 h, the heparin treatment was replaced by an injection of tinzaparin 0.6 mL each morning for 3 months. The patient did not receive any specific treatment for COVID, just symptomatic treatments. Within 10 days, there was a complete regression of his diplopia and ptosis, and he recovered from his COVID-19 infection.
Magnetic resonance imaging in sagittal, axial, and coronal reconstructions from 3D FLAIR Fat-Sat (a, b, c) and T1 with gadolinium injection in coronal and axial reconstruction (d, e) showing thrombosis of the right cavernous sinus associated with thrombosis and enlargement of the right ophthalmic vein (white arrows). The cranial CT scan after contrast in axial reconstruction (f) allows us to verify the good repermeabilization of the CST (white arrow)
Seven days after his cavernous thrombosis was discovered with an MRI, a follow-up brain scan showed regression of the thrombosis with complete recanalization of the cavernous sinus (Fig. 1). The patient was discharged from hospital 10 days after admission, and his anticoagulant treatment was continued for 3 months. He was symptom-free at both follow-up visits 1 month and 3 months later. Anticoagulants were discontinued after 3 months.
Discussion
The SARS-CoV-2 virus provokes a strong inflammatory response resulting in the release of cytokines, chemokines, and cell activation leading to a hypercoagulable state. Numerous and varied neurological manifestations have been described in association with COVID-19 infection, due to neuro-inflammatory or pro-thrombotic events and can be associated with severe and fatal complications, such as ischemic stroke or encephalitis [2] . COVID-19 infection is often diagnosed through PCR testing on nasopharyngeal specimens and, more recently, through the use of antigenic tests. However, radiological imaging remains informative and contributes to the diagnosis of COVID-19 complications. For example, the SARS-CoV-2 virus may result in neurotropism with neuro-invasive and neuro-inflammatory properties, which can be responsible for the damage of all cranial nerves. Isolated damage to nerve I is not the most commonly suggested pathophysiologic mechanism of olfactory loss in COVID, nor is the cranial nerve the one most commonly affected by the disease (VII, VI, and III). Ocular symptoms related to COVID-19 infection have also been documented, manifesting mainly with keratoconjunctivitis. The isolated impairment of cranial nerves has been described secondarily and mainly explained by neurotropism due to SARS-CoV-2 virus. In the case we presented, the impairment of cranial nerves was responsible for oculomotor paralysis and diplopia.
There is currently little literature on the association between cerebral venous thrombosis and COVID-19 infection. However, a recent multicenter study and review of literature showed that there is an increased risk of cerebral venous thrombosis in patients with COVID-19 infections, especially in cases of neurological symptoms [3] . CST is a rare condition, usually of septic, traumatic, or inflammatory origin [4] . COVID-19 infection frequently includes ENT involvement and symptoms. Nasal congestion and anosmia are common but are not likely to cause CST; paranasal sinus involvement is more likely to be associated with CST. Numerous cases of mucormycosis have been described following COVID-19 infection, in some cases leading to ophthalmological damage and CST [5] .
The case we have described is unusual since it deals with an elderly male patient, whereas cerebral venous thrombosis occurs primarily in young women [6] . Furthermore, the patient did not have any ENT infections, other than COVID-19. The clinical presentation and physical and pathological explanations are original and have received little attention in the literature. This includes symptoms of nerve III damage that did not result from inflammatory damage to the nerve but from thrombosis of a structure through which the nerve passes.
We identified five other cases of CST in the context of COVID-19 infection, but four of them included a concomitant ENT infection or recent dental extraction that could explain the occurrence of thrombosis [7] . Similar to our case, he had no personal or familial thrombotic risk factors [8] . Contrary to other cases described in the literature where most patients presented with a bacterial or mycotic infection of the ENT region [9,10,11,12,13] , the SARS-CoV-2 virus appears to be responsible for the cavernous thrombosis we have described. The rare case we present adds to the literature covering the wide variety of clinical presentations and complications associated with COVID-19 infections, including possible pro-thrombotic states. Radiological imaging was essential for the diagnosis of this rare complication and its follow-up treatment.
Conclusion
Complications associated with COVID-19 infections are becoming increasingly varied and are mainly related to the pro-inflammatory and pro-thrombotic state they can generate. The role of imaging in the management of affected patients remains essential, particularly in the diagnosis of rare complications, as was shown in our case with a CST.
Code Availability (Software Application or Custom Code)
Not applicable.
Data availability
Yes.
Abbreviations
- ENT:
-
Ear, nose, and throat
- CST:
-
Cavernous sinus thrombosis
- CT scan:
-
Computed tomography scanner
- MRI:
-
Magnetic resonance imaging
References
Gómez-Mesa JE, Galindo-Coral S, Montes MC, Muñoz Martin AJ. Thrombosis and coagulopathy in COVID-19. Curr Probl Cardiol mars. 2021;46(3):100742.
Kremer S, Lersy F, Anheim M, Merdji H, Schenck M, Oesterlé H, et al. 2020 Neurologic and neuroimaging findings in patients with COVID-19: a retrospective multicenter study. Neurology 29 95(13):186882
Abdalkader M, Shaikh SP, Siegler JE, Cervantes-Arslanian AM, Tiu C, Radu RA, et al. Cerebral venous sinus thrombosis in COVID-19 patients: a multicenter study and review of literature. Journal of Stroke and Cerebrovascular Diseases. juin 2021;30(6):105733.
Matthew TJH, Hussein A. Atypical cavernous sinus thrombosis: a diagnosis challenge and dilemma. Cureus. 2018;10(12):3685.
Nagalli S, Kikkeri NS. Mucormycosis in COVID-19: a systematic review of literature. Infez Med. 10 déc 2021;29(4):504‑12.
Alet M, Ciardi C, Alemán A, Bandeo L, Bonardo P, Cea C, et al. Cerebral venous thrombosis in Argentina: clinical presentation, predisposing factors, outcomes and literature review. J Stroke Cerebrovasc Dis. 2020;29(10):105145.
aljanabi KS kasim, almaqbali T, alkilidar A asaad H. A covid-19 patient with cavernous sinus thrombosis post dental extraction a diagnostic dilemma. Indian J Otolaryngol Head Neck Surg [Internet]. 26 févr 2021 [cité 2 août 2022]; Disponible sur: http://link.springer.com/10.1007/s12070-021-02460-9
Khacha A, Bouchal S, Ettabyaoui A, Haloua M, Lamrani YA, Boubbou M, et al. Cavernous sinus thrombosis in a COVID-19 patient: a case report. Radiology Case Reports mars. 2021;16(3):480–2.
Shukhrat BA, Dar-Odeh N, Dilnoza BT, Dildora RA, Matluba KA, Yokub KK, et al. Radiographic and clinical analysis of cranio-maxillofacial complications of cavernous sinus thrombosis among 256 COVID-19 patients. J Craniofac Surg. 2022;33(5):1549–53.
LoBue SA, Park R, Giovane R, DeLury J, Hodgson N. Bilateral cavernous sinus thrombosis in presumed COVID-19 infection. Cureus. 2022;14(11):e31986.
Khacha A, Bouchal S, Ettabyaoui A, Haloua M, Lamrani YA, Boubbou M, et al. Cavernous sinus thrombosis in a COVID-19 patient: a case report. Radiol Case Rep mars. 2021;16(3):480–2.
Aljanabi KSK, Almaqbali T, Alkilidar AAH. A covid-19 patient with cavernous sinus thrombosis post dental extraction a diagnostic dilemma. Indian J Otolaryngol Head Neck Surg. 2022;74(Suppl 2):2887–90.
Abdalkader M, Shaikh SP, Siegler JE, Cervantes-Arslanian AM, Tiu C, Radu RA, et al. Cerebral venous sinus thrombosis in COVID-19 patients: a multicenter study and review of literature. J Stroke Cerebrovasc Dis juin. 2021;30(6):105733.
Author information
Authors and Affiliations
Contributions
C. Duvillard managed the patient and P. Boureille performed the imaging. B. Geoffroy, R. Grange, and S. Grange wrote the manuscript. All authors corrected and approved the manuscript. S. Grange is the corresponding author.
Corresponding author
Ethics declarations
Ethics Approval
Oral and written consent has been obtained from the patient.
Consent to Participate
Yes.
Consent for Publication (include Appropriate Statements).
Yes.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Geoffroy, B., Grange, R., Boureille, P. et al. Cavernous Sinus Thrombosis Linked to COVID-19 Infection: a Case Report. SN Compr. Clin. Med. 5, 111 (2023). https://doi.org/10.1007/s42399-023-01450-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-023-01450-y