Abstract
Antimicrobial stewardship is essential to reducing antimicrobial resistance, reducing costs, and, crucially, ensuring good patient care. Community-acquired pneumonia (CAP) is a common medical condition, the symptoms of which show a significant overlap with those of COVID-19. Following the COVID-19 outbreak in Ireland, patients presenting to our hospital with features of a respiratory infection were more commonly reviewed within 24 hours (24h) of admission by an infectious disease (ID) or respiratory specialist. We aimed to assess how the change in service provision, involving frequent specialist reviews of patients admitted with features of CAP during the first wave of the COVID-19 pandemic, affected antimicrobial stewardship and prescribing practices. Patients admitted under general medical teams treated for CAP from March–April 2020 were included. Retrospective data including demographics, CURB-65 score, and antimicrobial therapy were collected, as well as information on whether the patient had undergone specialist review by an ID or respiratory physician. Data were compared to a similar cohort treated for CAP between November 2019 and January 2020, though in this cohort, before the era of COVID-19, none of the patients had undergone specialist review. Seventy-six patients were included from the March–April 2020 cohort, with 77 from November 2019–January 2020 for comparison. An ID or respiratory specialist reviewed 35 patients from the March–April cohort within 24 h of admission. There was a higher rate of appropriate escalation, de-escalation, and continuation of antibiotics among those reviewed. Less than 20% of patients were started on antibiotics in accordance with CAP guidelines on admission, though the antibiotics initiated were frequently deemed appropriate in the clinical setting. Specialist review increases rates of appropriate antimicrobial prescribing and adherence with hospital guidelines in patients with CAP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pneumonia is a common infectious cause of morbidity and mortality. It is considered the leading infection causing death in the USA [1], with a significant social and economic cost [2]. Non-compliance with prescribing guidelines is associated with longer hospital stays, increased mortality, and higher costs [3]. It is well documented that infectious disease specialist input reduces the rate of inappropriate prescribing and has been associated with shorter admission and decreased mortality [4].
The usefulness of well-validated scoring systems such as the CURB-65 in assessing severity and predicting mortality in patients admitted with Community-Associated Pneumonia (CAP) is well established [5], and the CURB-65 score is often used to form the basis of prescribing guidelines in hospitalized patients. The CURB-65 score is calculated based on five prognostic indicators, awarding one point for each of the following:
-
Confusion
-
Raised blood urea nitrogen (> 7 mmol/l)
-
Raised respiratory rate (> 30 breaths/minute)
-
Low systolic blood pressure (diastolic < 60 mmHg or systolic < 90 mmHg) and
-
age (65 years or older)
This allows physicians to stratify patients according to mortality risk and guides decision-making in both a community and hospital setting regarding the suitability for outpatient management versus the need for hospitalization [6]. It is also used to guide the optimal choice of antimicrobial therapy.
The diagnosis of superimposed bacterial infections in COVID-19 is challenging, due to overlapping clinical and radiological findings, as well as the added complexities of performing diagnostic procedures in patients with COVID-19 due to the risk to healthcare workers [7]. An international survey of antibiotic use in COVID-19 patients showed high rates of broad-spectrum antibiotic use, concluding that physicians should adhere to antimicrobial stewardship principles in order to reduce negative consequences of antimicrobials [8].
Methods
Patients treated for CAP between March–April 2020 were included. CAP was defined as either radiological evidence of pneumonia or a high clinical suspicion of pneumonia on the basis of history and examination in the absence of radiological findings.
Retrospective data were collected from electronic patient records, including demographics, documentation of CURB-65 score, microbiological and radiological results, and length of stay. Details of each patient’s antimicrobial therapy, including whether the antimicrobials initiated at the time of admission were compliant with hospital guidelines, whether they were appropriate in the clinical context, whether they were escalated or de-escalated during the course of admission (and whether this was appropriate in the clinical context), and the duration of therapy, were all recorded.
The antibiotic initiated by the admitting doctor (typically a non-consultant hospital doctor, often outside of regular working hours) was documented as the initial antibiotic, and changes made thereafter (including changes made on the post-take ward round or later in the admission) were also recorded.
If an antibiotic was administered intravenously, despite hospital guidelines advising oral administration for the CURB-65 score in question, this was recorded as being “non-compliant” with hospital guidelines.
In cases where the choice and route of antibiotic were incongruent with prescribing guidelines, further information was sought to clarify the reason for this. This included the presence of allergies and intolerances, contraindications, recent courses of antibiotics in the community, and information on prior sputum culture sensitivities that might have guided the choice of antibiotics.
Data were compared with a similar cohort of patients treated for CAP between November 2019 and January 2020.
We also recorded whether patients underwent specialist review by ID or respiratory services within 24 h of admission to hospital. This was a common occurrence among the March–April 2020 cohort (due to the outbreak of the COVID-19 pandemic), but did not occur in the November 2019–January 2020 cohort. Among the patients in the November 2019–January 2020 cohort, some had been assessed by the antimicrobial stewardship (AMS) team, but this did not typically occur within 24 h of admission. The AMS team made recommendations based on a virtual review of the patient’s condition and treatment regimen via the electronic patient records.
We used Microsoft Excel 2019® to compile data, with statistical analysis performed using IBM SPSS Statistics v.26.0 (IBM Corp., Armonk, NY). Categorical data was calculated using chi-squared test, while Mann–Whitney U test was used for non-normally distributed nominal data (length of stay, duration of treatment).
Inclusion Criteria
Patients admitted under a medical team with a clinical or radiological diagnosis of CAP, including those who had a suspected or confirmed diagnosis of COVID-19 with a suspected superimposed bacterial pneumonia.
Exclusion Criteria
Patients meeting the criteria for hospital-acquired or healthcare-associated pneumonia were excluded.
Patients with an infective exacerbation of COPD without clinical radiological features of pneumonia were also excluded.
Results
Seventy-six patients were included from March–April 2020, with 77 from November 2019–January 2020 for comparison. Details regarding their demographics, admission details, and antimicrobials initiated are outlined in Table 1. The two groups were similar in terms of age, gender, compliance with hospital guidelines, and treatment duration. There was a difference in the median length of stay, with patients admitted in the period from March–April 2020 staying an average of 2 days longer compared to those admitted between Nov 2019–Jan 2020, and this was statistically significant (9 days vs 7 days, p = 0.03).
Compliance with Hospital Guidelines
We found a low level of compliance with hospital prescribing guidelines (18.4% and 16.9%, respectively), but that the majority of the antimicrobials used were deemed appropriate in the clinical context. The main examples of non-compliance with guidelines included the use of intravenous antibiotics where oral antibiotics were advised, and the use of broad-spectrum antibiotics where narrow-spectrum was advised. The use of co-amoxiclav where amoxicillin was recommended and the use of intravenous co-amoxiclav where oral co-amoxiclav was recommended were the two most common deviations from the guidelines.
Common reasons for deviating from hospital guidelines included prior resistant organisms grown in sputum, unsuitability of the oral route for drug administration, acutely unwell patients deemed to warrant intravenous antibiotics, patients reporting no improvement with oral antibiotics in the community, and concerning features on chest radiography (such as pleural effusion). The reason elicited from medical notes for deviating from the guidelines were typically considered appropriate based on the clinical context (75% and 70.1%, respectively).
Documentation of the CURB-65 score was poor, and while a higher percentage of those with a documented CURB-65 score was initiated on therapy in accordance with the hospital guidelines (33.3 vs 15.6%), this was not statistically significant.
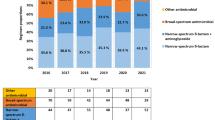
Choices of Antibiotics
The various antibiotics initiated at the time of admission are outlined in Table 2.
Coamoxiclav was the most commonly prescribed antimicrobial in the treatment of CAP, usually with a second agent (typically clarithromycin). The use of oral antibiotics at the time of initiating therapy was uncommon (10.5% and 7.8%, respectively).
A breakdown of CURB-65 scores and compliance with guidelines among all patients (including the Nov 2019–Jan 2020 and March–April 2020 cohorts) is outlined in Table 3. Compliance with hospital guidelines was higher among those with a CURB-65 score of 2 or greater compared with those with a CURB-65 score of 0–1 (55.2 vs 4.2%, p ≤ 0.001).
Assessing the Impact of the Specialist Review on Antibiotic Use
Of the 76 patients in the March–April 2020 cohort, 35 patients were reviewed by a respiratory or ID specialist within 24 h. The changes made to antibiotics following specialist review are outlined in Table 4.
Changes to antimicrobials included “escalation” (addition of another antibiotic or switch to a broader spectrum antibiotic), “de-escalation” (oral switch of an antibiotic, switch to a narrower spectrum antibiotic, or discontinuation of an antibiotic), or “unchanged” (where no change was made).
As outlined in Table 4, the likelihood of appropriate changes to antimicrobials was increased by respiratory or ID specialist review within 24 h (94.3 vs 68.3%, p < 0.01). The most common escalation of antimicrobials involved switching co-amoxiclav to piperacillin-tazobactam, and this was usually based on a poor clinical response to initial therapy or the results of microbiological investigations. The most common de-escalation involved switching from the intravenous to the oral route or discontinuing the second agent (typically clarithromycin).
In the November 2019–January 2020 cohort, 25 patients were reviewed by the AMS team. Of these, 15/25 (60%) underwent appropriate escalation, de-escalation, or discontinuation of antimicrobials. In 22 of these cases, recommendations were made by the AMS team regarding changes to antimicrobials. In the majority of cases (15/25; 60%), the advice was to de-escalate or discontinue antimicrobials, while in 6/25 (24%) of cases they advised escalation of antimicrobial therapy.
Duration of Therapy
Among the March–April 2020 cohort, 43/76 (56.6%) of patients continued antibiotic therapy for the recommended duration, with 30 continuing antibiotics for longer than advised (though in several cases the presence of clinical deterioration or subsequent hospital-acquired or aspiration pneumonia was a confounding factor), while just one patient had their antibiotics stopped early. Two patients continued on antibiotic therapy for a prolonged period due to the detection of concomitant non-respiratory infections that required further therapy.
There was no statistically significant difference in the likelihood of a patient undergoing an appropriate duration of therapy following specialist review.
Among the November 2019–January 2020 cohort, 33/77 (42.9%) of patients continued antibiotics for the recommended duration. Of the 25 patients reviewed by the AMS team, only six (24%) completed the recommended duration of therapy.
Transfer of Care to a Specialist Team
The care of 29/76 patients admitted during the COVID-19 pandemic was taken over by a specialist respiratory or infectious disease team during the course of their admission with CAP (ten of whom had not been seen within 24 h of admission). This was usually due to a diagnosis of COVID-19, with other reasons including complex infections, or underlying respiratory or infectious diseases. These patients were more likely to undergo appropriate escalation or de-escalation of their antibiotics when compared with those who did not undergo a transfer of care to a specialist team (96.6 vs 70.2%, p = 0.005).
A higher percentage of patients who underwent a transfer of care was continued on antimicrobials for an appropriate duration, though this was not statistically significant (72.4 vs 51%, p = 0.066).
Investigations
Among the March–April 2020 cohort, 100% of patients included in the study had undergone chest radiography upon admission.
Seventeen patients (22.4%) had undergone sputum testing, while 27 (35.5%) had undergone urinary antigen testing.
Among the 32 patients with a CURB-65 score of two or more, only three patients (9.4%) had undergone all three of urinary antigen testing, blood cultures, and sputum cultures. Fourteen had undergone blood cultures, twelve had undergone urinary antigen testing, and five had undergone sputum testing.
Discussion
The results of this service evaluation suggest a low level of adherence to prescribing guidelines in the treatment of community-acquired pneumonia. Adherence rates were similar to the 16.1% demonstrated in an Australian study of 193 patients admitted with CAP [9], but fell well short of the 52.3% compliance found in a similarly sized study in a French teaching hospital [10]. In an Irish setting, an audit of antimicrobial prescribing in 69 hospitalized patients with CAP showed 21.6% compliance with guidelines [11].
We did, however, find that the choice of antibiotic was frequently deemed appropriate in the clinical context. This highlights the importance of physicians’ clinical judgment in conjunction with the CURB-65 scoring system and hospital prescribing guidelines. Indeed, the authors who developed the CURB-65 scoring system emphasized that “overall clinical judgment is crucial” when applying it to clinical practice [6]. It is important to note that co-morbid conditions, failure of community-prescribed antibiotic therapy, and social circumstances are not represented in the CURB-65 scoring system [12]. These variables may have led to the decision to deviate from hospital guidelines.
Those patients with a higher CURB-65 score were more likely to receive antibiotics in accordance with hospital guidelines suggests that non-consultant hospital doctors (NCHDs) are more familiar with hospital guidelines for higher-scoring patients. This may also reflect a hesitancy among NCHDs in the use of oral agents or monotherapy in patients admitted with CAP and a low CURB-65 score.
Our findings suggest that clinicians should ensure that they are familiar with CURB-65 guidelines (including situations where oral agents may be sufficient), while supporting recommendations that guidelines should be interpreted in conjunction with clinical judgment on a case-by-case basis.
Specialist review by an ID or respiratory specialist increased rates of appropriate antimicrobial prescribing, but the impact on appropriate treatment duration was not statistically significant. Statistical significance might have been achieved with a bigger sample size. Only 56.6% of patients completed an appropriate duration of therapy, and the median duration of therapy specifically targeting CAP was 7 days. This compared favorably with a nationwide study performed in the USA, which found a median total length of therapy of 9.5 days [13].
At a time when infectious disease services are being expanded across Irish hospitals, this study highlights a potential benefit of the expansion of these services in the optimal management of patients hospitalized with CAP. These findings are in keeping with prior studies that demonstrate the positive impact of ID specialist input on antibiotic prescribing practices internationally. A review article analyzing 31 studies carried out in multiple centers worldwide, predominantly across Europe and the USA, found that ID specialist input improves prescribing practices, while also reducing the length of stay and mortality [4].
The CURB-65 scoring system does appear to be valid when used in low- and middle-income countries (LMICs) [14]. However, the significance of our findings to LMICs may be hindered by a lack of trained specialists in the area. In South Africa, for example, the first ID specialists graduated in 2004, and the majority of their workload is focused on the management of patients with human immunodeficiency virus (HIV) and tuberculosis [15]. Expansion of services, closing knowledge gaps, expansion of diagnostics, and improved access to antimicrobials are all issues that must be addressed in order to combat the threat of antimicrobial resistance in LMICs [16].
From a public health perspective, multi-drug-resistant bacteria pose a major challenge in the community as well as in healthcare settings. Myriad organisms traditionally associated with the healthcare setting are now emerging as causes of CAP, so that we now consider healthcare-associated pneumonia (HCAP) as a different entity to CAP [17]. This will add to the challenge of providing effective guidelines for the treatment of CAP, both in the community and hospital setting. Having highlighted the role of specialist input in improving antibiotic prescribing in a hospital setting, we suggest a potential role for collaboration between ID and public health specialists to seek to address these challenges.
There are no large-scale analyses of the specific impact of ID or respiratory input on prescribing practices in CAP, and this study highlights the need for further research in this area.
Limitations of this study include the relatively small sample size and the potential influence of seasonal variation. Furthermore, a lack of data regarding the optimal treatment of COVID-19 at a time of great concern and uncertainty within the medical community may have influenced antibiotic prescribing practices among general medical physicians and ID/respiratory specialists alike. Finally, the difference between average lengths of stay in each cohort was statistically significant. This may reflect increased uncertainty regarding the appropriate duration of therapy, duration of isolation, and availability of facilities for patients to self-isolate upon discharge with a diagnosis of COVID-19. Ultimately, a large-scale study is required to analyze the impact of COVID-19 on prescribing practices in CAP, and a repeat study outside of the pandemic setting would be valuable for comparison.
Another limitation was that as ID and respiratory specialists were not regularly involved in the care of patients with CAP in the patient cohort from November 2019–December 2020 (i.e., before the COVID-19 pandemic), there was no equivalent group for direct comparison. We have included patients from the November 2019–December 2020 cohort who had been reviewed by the AMS team as a surrogate. However, as the AMS team often reviewed patients more than 24 h into their admission, and did not perform a physical clinical assessment or provide ongoing recommendations regarding patient care, they are not truly comparable.
In summary, this service evaluation demonstrates the value of ID and respiratory specialist input in prescribing practices in CAP. Overall, compliance with prescribing guidelines is low, but the choice of antibiotic can often be deemed appropriate in the clinical context.
Our findings may reflect a lack of familiarity or a lack of confidence in following prescribing guidelines (particularly in prescribing oral antibiotics) in patients requiring hospitalization, especially when treating patients with a low CURB-65 score. This suggests a need for increased awareness and education of prescribing guidelines, particularly among NCHDs, who are commonly the ones initiating therapy at the time of hospital admission.
Data Availability
Data and materials are available upon reasonable request from the corresponding author.
Code Availability
Available upon reasonable request
References
Restrepo MI, Faverio P, Anzueto A. Long-term prognosis in community-acquired pneumonia. Curr Opin Infect Dis. 2013;26(2):151–8.
Triantafyllidis C, Kapordelis V, Papaetis GS, et al. Guidelines adherence for patients with community acquired pneumonia in a Greek hospital. Eur Rev Med Pharmacol Sci. 2012;16(1):1–9.
Delaney F, Jackson A. An audit of empiric antibiotic choice in the inpatient management of community-acquired pneumonia. Ir Med J. 2017;110(4):545.
Pulcini C, Botelho-Nevers E, Dyar OJ, et al. The impact of infectious disease specialists on antibiotic prescribing in hospitals. Clin Microbiol Infect. 2014;20(10):963–72. https://doi.org/10.1111/1469-0691.12751.
Shindo Y, Sato S, Maruyama E, et al. Comparison of severity scoring systems A-DROP and CURB-65 for community-acquired pneumonia. Respirology. 2008;13(5):731–5. https://doi.org/10.1111/j.1440-1843.2008.01329.x.
Lim WS, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58:377–82.
Ginsburg AS, Klugman KP. COVID-19 pneumonia and the appropriate use of antibiotics. Lancet Glob Health. 2020;8(12):e1453–4. https://doi.org/10.1016/S2214-109X(20)30444-7.
Beović B, Doušak M, Ferreira-Coimbra J, et al. Antibiotic use in patients with COVID-19: a ‘snapshot’ Infectious Diseases International Research Initiative (ID-IRI) survey. J Antimicrob Chemother. 2020;75(11):3386–90. https://doi.org/10.1093/jac/dkaa326.
Almatar MA, Peterson GM, Thompson A, et al. Community-acquired pneumonia: why aren’t national antibiotic guidelines followed? Int J Clin Pract. 2015;69(2):259–66. https://doi.org/10.1111/ijcp.12538.
Martinez JS, Le Falher G, Corne P, et al. Audit des prescriptions d’antibiotiques dans les pneumonies aiguës communautaires de l’adulte dans un centre hospitalier universitaire [adherence to antibiotherapy guidelines for acute community-acquired pneumonia in adults, in a teaching hospital]. Med Mal Infect. 2010;40(8):468–75. https://doi.org/10.1016/j.medmal.2010.01.009 (French).
O’Kelly B, Rueda-Benito A, O’Regan M, et al. An audit of community-acquired pneumonia antimicrobial compliance using an intervention bundle in an Irish hospital. J Glob Antimicrob Resist. 2020;23:38–45. https://doi.org/10.1016/j.jgar.2020.07.021.
Adler N, Weber H, Gunadasa I, et al. Adherence to therapeutic guidelines for patients with community-acquired pneumonia in Australian hospitals. Clin Med Insights Circ Respir Pulm Med. 2014;8:17–20. https://doi.org/10.4137/CCRPM.S17978 (Published 2014 Sep 14).
Yi SH, Hatfield KM, Baggs J, et al. Duration of antibiotic use among adults with uncomplicated community-acquired pneumonia requiring hospitalization in the United States. Clin Infect Dis. 2018;66(9):1333–41. https://doi.org/10.1093/cid/cix986.
Al Hussain SK, Kurdi A, Abutheraa N, et al. Validity of pneumonia severity assessment scores in Africa and South Asia: a systematic review and meta-analysis. Healthcare (Basel). 2021;9(9):1202. https://doi.org/10.3390/healthcare9091202.
Richards L, Spencer DC, Nel JS, et al. Infectious disease consultations at a South African academic hospital: a 6-month assessment of inpatient consultations. S Afr J Infect Dis. 2020;35(1):169. https://doi.org/10.4102/sajid.v35i1.169.
Pierce J, Apisarnthanarak A, Schellack N, et al. Global antimicrobial stewardship with a focus on low- and middle-income countries. Int J Infect Dis. 2020;96:621–9. https://doi.org/10.1016/j.ijid.2020.05.126.
Falcone M, Tiseo G, Menichetti F. Community-acquired pneumonia owing to multidrug-resistant pathogens: a step toward an early identification. Ann Am Thorac Soc. 2021;18(2):211–3. https://doi.org/10.1513/AnnalsATS.202009-1207ED.
Author information
Authors and Affiliations
Contributions
All authors made significant contributions to the concept, design, and writing of this service evaluation project.
Corresponding author
Ethics declarations
Ethics Approval
This service evaluation project was approved by the Research and Innovation Office at St James’s Hospital.
Consent to Participate
Consent to participate was waived in view of the observative nature of this service evaluation project.
Consent for Publication
The corresponding author grants consent for publication on behalf of all authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Covid-19
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Howley, F., Keating, D., Kelly, M. et al. A Service Evaluation of Adherence with Antimicrobial Guidelines in the Treatment of Community-Acquired Pneumonia Before and During the SARS-CoV-2 Outbreak. SN Compr. Clin. Med. 4, 225 (2022). https://doi.org/10.1007/s42399-022-01311-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-022-01311-0