Abstract
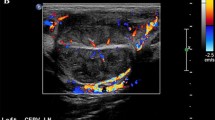
Cervical lymphadenopathy is a common clinical entity with varied causes. The current study aims to evaluate the diagnostic performance of sonography, sonoelastography, and their combination for differentiation between benign and malignant causes of cervical lymphadenopathy. After approval of study protocol by the hospital review board and written informed consent, 70 neck nodes in 70 patients were evaluated with grayscale ultrasound and color Doppler followed by ultrasound strain elastography (USE). The final diagnosis was based on ultrasound-guided fine-needle aspiration cytology (FNAC)/histopathological examination (HPE). Various ultrasound features observed were nodal size, shape, presence of echogenic hilum, intranodal necrosis, and pattern of vascularity. Score was given for each feature and the sum was used for calculation of diagnostic accuracy of sonography. Ultrasound elastography was interpreted by obtaining color-coded elastogram and strain ratio. Cut-offs for all the parameters were determined from receiver operating characteristic (ROC) curve. The diagnostic performance of conventional ultrasound and sonoelastography was evaluated individually as well as in combination against cytological or histopathological diagnosis. Out of 70 nodes examined, 36 were malignant and 34 were benign on histopathology. Among all ultrasound features, pattern of vascularity on color Doppler showed maximum sensitivity, i.e., 94%, while intranodal necrosis had maximum specificity, i.e., 70%, for differentiation between benign and malignant cervical lymphadenopathy. Sensitivity, specificity, and accuracy were 68.6%, 60%, and 64.3%, respectively, for ultrasound with Doppler; 77.15, 92.3%, and 85.7% for sonoelastography; and 60%, 97.1%, and 77.1% for combined evaluation. Strain ratio had highest specificity (94.3%) and diagnostic accuracy (85.7%) among all ultrasound and elastographic parameters. Combined ultrasound and ultrasound elastographic evaluation shows better diagnostic accuracy compared to conventional ultrasound evaluation. Ultrasound evaluation should be followed by elastography in all cases of cervical lymphadenopathy wherever possible.







Similar content being viewed by others
Data Availability
Analyzed data is included in the article. Dataset used for the current study is available with the corresponding author and available on request.
References
Som PM. Detection of metastasis in cervical nodes: CT and MR criteria and differential diagnosis. Am J Roentgenol. 1992;158:961–9.
Dudea SM, Lenghel M, Botor-Jid C, Vassilescu D, Duma M. Ultrasonography of superficial lymph nodes: benign vs malignant. Med Ultrason. 2012;4:294–306.
Ying M, Bhatia KSS, Lee YP, et al. Review of ultrasonography of malignant neck nodes: grayscale, Doppler, contrast enhancement, and elastography. Cancer Imaging. 2013;13:658–69.
Sigrist RMS, Liau J, Kaffas AE, Chammas MC, Willmann JK. Ultrasound elastography: review of techniques and clinical applications. Theranostics. 2017;7:1303–29.
Desmots F, Fakhry N, Mancini J, Reyre A, Vidal V, Jacquier A, et al. Shear wave elastography in head and neck lymph node assessment: image quality and diagnostic impact compared with B-mode and Doppler ultrasonography. Ultrasound Med Biol. 2016;42:387–98.
Choi YJ, Lee JH, Baek JH. Ultrasound elastography for evaluation of cervical lymph nodes. Ultrasonography. 2015;34:157–64.
AlamF NK, Horiguchi J, Fukuda H, Tachikake T, Ito K. Accuracy of sonographic elastography in the differential diagnosis of enlarged cervical lymph nodes: comparison with conventional B-mode sonography. Am J Roentgenol. 2008;191:604–10.
Moharram MA, Maboud NMA, Ahmed HAE. Evaluation of the role of sono-elastography in diagnosis of enlarged cervical lymph nodes, The Egyptian Journal of Radiology and Nuclear Medicine. 2017;48:381–91.
Lyshchik A, Higashi T, Asato R, et al. Cervical lymph node metastasis: diagnosis at sonoelastography-initial experience. Radiology. 2007;243:258–67.
AJCC. American Joint Committee on Cancer Staging Manual. 5th ed. Philadelphia, PA: Lippincott-Raven; 1997.
Prativadi R, Dahiya N, Kamaya A, Bhatt S. Ultrasound characteristics of benign vs. malignant cervical lymph nodes. SeminUltrasound CT and MRI. 2017;38:506–15.
Kuna SK, Bracic I, Tesic V, Kuna K, Herceg GH, Dodig D. Ultrasonographic differentiation of benign from malignant neck lymphadenopathy in thyroid cancer. J Ultrasound Med. 2006;25:1531–7.
Evans RM, Ahuja A, Metreweli C. The linear echogenic hilus in cervical lymphadenopathy—a sign of benignity or malignancy? Clin Radiol. 1993;47:262–4.
Ahuja A, Ying M, King W, Metreweli C. A practical approach to ultrasound of cervical lymph nodes. J Laryngol Otol. 1997;111:245–56.
Giacomini CP, Jeffrey RB, Shin LK. Ultrasonographic evaluation of malignant and normal cervical lymph nodes. Semin Ultrasound CT MRI. 2013;34:236–47.
Wu CH, Chang YL, Hsu WC, Ko JY, Hsieh FS. Usefulness of Doppler spectral analysis and power Doppler sonography in differentiation of cervical lymphadenopathies. Am J Roentgenol. 1998;171:503–9.
DangoreSB DSS, Bhowate RR. Evaluation of the efficacy of color Doppler ultrasound in diagnosis of cervical lymphadenopathy. Dentomaxillofacial Radiol. 2008;37:205–12.
Wu CH, Chang YL, Hsu WC, Ko JY, Hsieh FS. Usefulness of Doppler spectral analysis and power Doppler sonography in differentiation of cervical lymphadenopathies. Am J Roentgenol. 1998;171:503–9.
Lo WC, Cheng PW, Wang CT, Liao LJ. Real time ultrasound elastography: an assessment of enlarged cervical lymph nodes. EurRadiol. 2013;23:2351–7.
Zakaria OM, Mousa A, AlSadhan R, et al. Reliability of sonoelastography in predicting pediatric cervical lymph node malignancy. Pediatr Surg Int. 2018;34:885–90.
Kanagaraju V, Rakshith AV, Devanand B, Rajakumar R. Utility of ultrasound elastography to differentiate benign from malignant cervical lymph nodes. J Med Ultrasound. 2020;28:92–8.
Tan R, Xiao Y, He Q. Ultrasound elastography: its potential role in assessment of cervical lymphadenopathy. AcadRadiol. 2010;17:849–55.
Zhang Y, Lv Q, Yin Y, et al. The value of ultrasound elastography in differential diagnosis of superficial lymph nodes. Front Med China. 2009;3:368–74.
Lenghel LM, Bolboaca SD, Botar-Jid C. The value of a new score for sonoelastographic differentiation between benign and malignant cervical lymph nodes. Med Ultrason. 2012;14:271–7.
Ying L, Hou Y, Zheng HM, et al. Real time elastography for the differentiation of benign and malignant superficial lymph nodes: a meta-analysis. Eur J Radiol. 2012;81:2576–84.
Teng DK, Wang H, Lin YQ, Sui GQ, Guo F, Sun LN. Value of ultrasound elastography in assessment of enlarged cervical lymph nodes. Asian Pac J Cancer Prev. 2012;13:2081–5.
Eldine AM, El-Gazzar N, Mashaly EM, Alarabawy RA, Abd-EISalam S. Differentiating benign from malignant cervical lymph nodes with sonoelastography. Int J Med Imaging. 2017;5(4):42–6.
Chae SY, Jung HN, Ryoo I, et al. Differentiating cervical metastatic lymphadenopathy and lymphoma by shear wave elastography. Sci Rep. 2019;9:12396.
Author information
Authors and Affiliations
Contributions
Each author contributed substantially to the design of work. RY and AM collected, analyzed, and interpreted the patient data generated from sonographic and sonoelastographic examination in cervical lymphadenopathy. RP performed the histopathological examination of FNAC/biopsy slides. RY and AM were major contributors in manuscript writing. All authors have read and approved the final manuscript and take full accountability of the work and data given.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The study was approved by the ethical committee of Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India, 110029, with approval number IEC/VMMC/SJH/Thesis/November - 2014/411. Written informed consent was obtained from all study subjects before enrolling into study
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Imaging
Rights and permissions
About this article
Cite this article
Yadav, R., Malik, A. & Prasad, R. Utility of Sonoelastography Beyond Sonography for Differentiation Between Benign and Malignant Lymphadenopathy. SN Compr. Clin. Med. 3, 2116–2126 (2021). https://doi.org/10.1007/s42399-021-00980-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-021-00980-7