Abstract
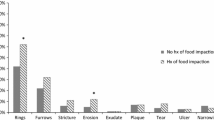
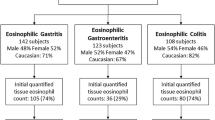
We describe 101 EoE patients with dysphagia, with food impaction (EoE-FI) and without food impaction (EoE-NoFI). Compare clinical features, endoscopy, histology and 10 additional histological features (AHF), and outcomes. Clinical features, dysphagia score, and endoscopic findings were captured. Eosinophils and 10 AHF at diagnosis and follow-up were done. Two hundred seven patients were seen with EoE, 101 patients with dysphagia enrolled; Follow period was; EoE-FI, and 71 EoE-NoFI and mean ages of 10.9 and 10.4 years, respectively (p = 0.27). Clinical features, EGD, and biopsies were almost similar in both groups. EoE-FI, 1.7 years (mean), range 1/12–8 years, and EoE-NoFI, 1.1 years (1/12–7 years). Dysphagia score improved from 3 to 1.25 in EoE-FI and 1.21 to 0.71 in EoE-NoFI (p < 0.001). Composite score improved from 3.3 to 1.45 and 2.49 to 1.48 (p < 0.001) in EoE-FI and EoE-NoFI; 15/30 (EoE-FI) and 45/71(EoE-NoFI) patients had repeat EGD. Peak eosinophils in EoE-FI improved from 60 to 27 (p = 0.03), and in EoE-NoFI from 47.6 to 33 (p = 0.001). Mean eosinophils in EoE-FI improved from 42 to 27.5 (p = 0.03), and EoE-NoFI from 39.3 to 22.1(p < 0.001). Comparison of the 10 AHF at diagnosis and follow-up showed minimal numerical (%) differences, and none were significant. During follow-up, none had recurrence or occurrence of FI in both groups. There were no significant differences in the clinical features and outcomes of dysphagia in EoE-FI and EoE-NoFI groups. Endoscopy including strictures and histologic findings of eosinophils and the 10 AHF were similar in both groups at diagnosis and follow-up.
Similar content being viewed by others
References
Dellon E, Liacouras C, Molina-Infante J, et al. Updated international consensus diagnostic criteria for eosinophilic esophagitis: proceedings of the AGREE Conference. Gastroenterology. 2018;155:1022–33.
Liacouras C, Furuta GA, Hirano I, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011;128:1–41.
Furuta GT, Liacouras CA, Collins MH, et al. Eosinophilic esophagitis in children and adults: a systematic review and consensus recommendations for diagnosis and treatment. Gastroenterology. 2007;133:1342–63.
Gunasekaran T, Prabhakar G, Schwartz A, et al.. Eosinophilic esophagitis (EoE) in children and adolescents with abdominal pain. Comparison with EoE-Dysphagia and Functional Abdominal Pain. Can J Gastroenterol Hepatol 2016 https://www.hindawi.com/journals/cjgh/2016/4123692/cta/.
Gunasekaran T, Chu C, Chennuri R, et al. Detailed histologic evaluation of eosinophilic esophagitis in pediatric patients presenting with dysphagia or abdominal pain and comparison of the histology between the two groups. Can J Gastroenterol Hepatol. 2017:3709254. https://doi.org/10.1155/2017/3709254.
Al-Hussaini A. Savary dilation is safe and effective treatment for esophageal narrowing related to pediatric eosinophilic esophagitis. J Pediatr Gastroenterol Nutr. 2016;63:474–80.
Dohil R, Newbury R, Fox, et al. Oral viscous budesonide is effective in children with eosinophilic esophagitis in a randomized, placebo-controlled trial. Gastroenterology. 2010;139:418–29.
Eskian M, Khorasanizadeh M. Assa’ad AH et al Monoclonal antibodies for treatment of eosinophilic esophagitis. Clin Rev Allergy Immunol. 2018;55:88–98.
Longstreth GF, Longstreth KJ, Yao JF. Esophageal food impaction: epidemiology and therapy. A retrospective, observational study. Gastrointest Endosc. 2001;53:193–208.
Ko HH, Enns R. Review of food bolus management. Can J Gastroenterol. 2008;22:805–8.
Hiremath GS, Hameed F, Pacheco A, et al. Esophageal food impaction and eosinophilic esophagitis: a retrospective study, systematic review, and meta-analysis. Dig Dis Sci. 2015;60:3181–93.
Diniz LO, Towbin AJ. Causes of esophageal food bolus impaction in pediatric population. Dig Dis Sci. 2012;57:690–3.
Desai TK, Stecevic V, Chang CH, et al. Association of eosinophilic inflammation with esophageal food impaction in adults. Gastrointest Endosc. 2005;61:795–801.
El-Matary W, El-Hakim H, Popel J. Eosinophilic esophagitis in children needing emergency endoscopy for foreign body and food bolus impaction. Pediatr Emerg Care. 2012;28:611–3.
Straumann A, Bussmann C, Zuber M, et al. Eosinophilic esophagitis: analysis of food impaction and perforation in 251 adolescent and adult patients. Clin Gastroenterol Hepatol. 2008;6:598–600.
Dellon ES, Jensen ET, Martin CF, Shaheen NJ, Kappelman MD. Prevalence of eosinophilic esophagitis in the United States. Clin Gastro Hepatology. 2014;12:589–96.
Gawron AJ, Hirano I. Eosinophilic esophagitis—emerging epidemic or misdiagnosed malady? Clin Gastro Hepatology. 2014;12:597–8.
Mittal RK. Esophageal function testing: beyond manometry and impedance. Gastrointest Endosc Clin N Am. 2014;24:667–85.
Mittal RK. Longitudinal muscle of the esophagus; its role in the esophageal health and disease. Curr Opin Gastroenterol. 2013 Jul;29(4):421–30. https://doi.org/10.1097/MOG.0b013e3283622b57.
Korsapati H, Babaei A, Bhargava V, et al. Dysfunction of the longitudinal muscles of the esophagus in eosinophilic esophagitis. Gut. 2009;58:1056–62.
Kwiatek MA, Hirano I, Kahrillas PJ, et al. Mechanical properties of the esophagus in eosinophilic esophagitis. Gastroenterology. 2011;140:82–90.
Maheen H, Aceves S, Dohil R, et al. Esophageal compliance quantifies epithelial remodeling in pediatric patients with eosinophilic esophagitis. J Pediatr Gastroenterol Nutr. 2019;68:559–68.
Menard-Katcher C, Benitez AJ, Pan Z, et al. Influence of age and eosinophilic esophagitis on esophageal distensibility in a pediatric cohort. Am J Gastroenterol. 2017;112:1466–73.
Menard-Katcher C, Benitez AJ, Ahmed F, et al. Esophageal distensibility provides measure of remodeling in pediatric eosinophilic esophagitis. Gastroenterology. 2016;150:S17–8.
Murch S, Allen KJ, Chong SKF, et al. Potential for improving therapy and defining new research targets in eosinophilic esophagitis based on understanding of immunopathogenesis. J Pediatr Gastroenterol Nutr. 2013;57:529–34.
de Boer RE, Brouwer F, Zaagsma J. The beta-adrenoceptors mediating relaxation of rat esophageal muscularis mucosae are predominantly of the beta 3-, but also of the beta 2-subtype. Br J Pharmacol. 1993;110:442–6.
Crowell MD, Zayat EN, Lacy BE, et al. The effects of an inhaled beta-2 adrenergic agonist on lower esophageal function: a dose-response study. Chest. 2001;120:1184–9.
Okamura S, Oshimoto H, Sakamoto T, et al. Beta-adrenoreceptor agonists for diffuse esophageal spasm. J Gastroenterol. 2002;37:229–30.
Dias JA, Fernandes S, Corujeira S, et al. Salbutamol therapy for food impaction in eosinophilic esophagitis. J Pediatr Gastroenterol Nutr. 2017;65:e97. https://doi.org/10.1097/MPG.0000000000001661.
Schoepfer AM, Safroneeva E, Bussmann C, et al. Delay in diagnosis of eosinophilic esophagitis increases risk for stricture formation in a time–dependent manner. Gastroenterology. 2013;145:1230–6.
Collins MH, Martin LJ, Alexander ES, et al.. Newly developed and validated eosinophilic esophagitis histology scoring system and evidence that it outperforms peak eosinophil count for disease diagnosing and monitoring. Dis Esophagus 2016; Feb 9. doi:10.1111/dote.12470.
Acknowledgements
The authors thank Henry Mangurten, MD, for the editorial revision of the manuscript.
Availability of Data and Materials
N/A
Code Availability
N/A
Author information
Authors and Affiliations
Contributions
Thirumazhisai S. Gunasekaran, MD — study concept and design, drafting of the manuscript, final approval, and study supervision and administrative. Vijayalakshmi Kory, MBBS — data collection, analysis, and administrative. Snehal S. Sonawane, MBBS, MD — study design and interpretation of the histology. Mohamed Rizwan Haroon Al Rasheed, MBBS, MD — study design and interpretation of the histology. Brian Adley, MD — study design and supervision/interpretation of the histology. Alan Schwartz, PhD — statistical analysis and interpretation of data. James Berman, MD — critical revision of the manuscript for important intellectual.
Corresponding author
Ethics declarations
Ethics Approval
Institutional Review Board approval for this study was obtained through Advocate Health Care, Oak Brook, IL, USA.
Consent to Participate
This is a retrospective study, and as per the above IRB, no consent was needed.
Consent for Publication
The authors give consent for publication of the manuscript if approved for publication.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
About this article
Cite this article
Gunasekaran, T.S., Kory, V., Sonawane, S.S. et al. Comprehensive Comparison of Dysphagia Predominant Eosinophilic Esophagitis: With and Without Food Impaction. SN Compr. Clin. Med. 3, 2134–2140 (2021). https://doi.org/10.1007/s42399-021-00889-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-021-00889-1