Abstract
Purpose
Translational research allowed us to hypothesize that endoscopic surgery performed with new generation 3D systems could improve surgeons’ performance, reducing the learning curve, and the perceived workload. However, there is currently a lack of evidence in randomized clinical trials considering advantages for the surgeon and the patient of using the new 3D systems. This systematic review of literature aims to understand what are the differences when performing an endoscopic surgery with new 3D or 2D systems when it comes to intra-operative, post-operative and surgeons perspective outcomes, and at the same time, understand what were the difficulties encountered when performing research about as different imaging systems for surgeons.
Methods
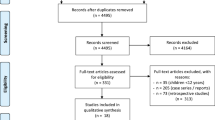
A systematic review of literature was conducted through an online search in databases MEDLINE ©/PubMed © to identify articles published in English, from 1st January 2014 to 31st May 2019, that compared clinical results of 2D and 3D third-generation video-assisted surgery.
Results
A total of 30 articles were included in the qualitative analyses. Of the 30 articles analyzed, 13 were articles in which patients were randomly selected, of which 7 were considered to be at “Low” risk of bias. From the 7 articles, 2 demonstrated an association between lower blood loss and 3D systems. In this selection of low risk randomized articles, no differences were observed in any of the studies when it comes to conversion to open surgery, intra-operative complications, morbidity, length of stay, and oncological outcomes.
Conclusion
In conclusion, this systematic review presents the current knowledge on clinical use of 3D systems for endoscopic surgery. Significant scientific evidence puts 3D technology with advantages in surgeon performance, learning curve, and fatigue.

Similar content being viewed by others
Data Availability
Not applicable.
References
Sakata S, Watson MO, Grove PM, Stevenson ARL. The conflicting evidence of three-dimensional displays in laparoscopy a review of systems old and new. Ann Surg. 2016;263:234–9. https://doi.org/10.1097/SLA.0000000000001504.
Durrani AF, Preminger GM. Three-dimensional video imaging for endoscopic surgery. Comput Biol Med. 1995;25:237–47. https://doi.org/10.1016/0010-4825(95)00001-K.
Stewart L, Way LW. The prevention of laparoscopic Bile duct injuries: An analysis of 300 cases of from a human factors and cognitive psychology perspective. Proc Hum Factors Ergon Soc. 2007;2:617–20. https://doi.org/10.1177/154193120705101103.
Cicione A, Autorino R, Breda A, De Sio M, Damiano R, Fusco F, et al. Three-dimensional vs standard laparoscopy: comparative assessment using a validated program for laparoscopic urologic skills. Urology. 2013;82:1444–50. https://doi.org/10.1016/j.urology.2013.07.047.
Storz P, Buess GF, Kunert W, Kirschniak A. 3D HD versus 2D HD: Surgical task efficiency in standardised phantom tasks. Surg Endosc. 2012;26:1454–60. https://doi.org/10.1007/s00464-011-2055-9.
El Boghdady M, Ramakrishnan G, Tang B, Alijani A. A comparative study of generic visual components of two-dimensional versus three-dimensional laparoscopic images. World J Surg. 2018;42:688–94. https://doi.org/10.1007/s00268-017-4220-3.
Wagner OJ, Hagen M, Kurmann A, Horgan S, Candinas D, Vorburger SA. Three-dimensional vision enhances task performance independently of the surgical method. Surg Endosc. 2012;26:2961–8. https://doi.org/10.1007/s00464-012-2295-3.
Tanagho YS, Andriole GL, Paradis AG, Madison KM, Sandhu GS, Varela JE, et al. 2D versus 3D visualization: impact on laparoscopic proficiency using the fundamentals of laparoscopic surgery skill set. J Laparoendosc Adv Surg Tech. 2012;22:865–70. https://doi.org/10.1089/lap.2012.0220.
Sakata S, Grove PM, Hill A, Watson MO, Stevenson ARL. Impact of simulated three-dimensional perception on precision of depth judgements, technical performance and perceived workload in laparoscopy. Br J Surg. 2017;104:1097–106. https://doi.org/10.1002/bjs.10528.
Vilaça J, Leite M, Correia-Pinto J, Högemann G, Costa P, Leão P. The influence of 3D in single-port laparoscopy surgery: an experimental study. Surg Laparosc Endosc Percutaneous Tech. 2018;28:261–6. https://doi.org/10.1097/SLE.0000000000000536.
Honeck P, Wendt-Nordahl G, Rassweiler J, Knoll T. Three-dimensional laparoscopic imaging improves surgical performance on standardized ex-vivo laparoscopic tasks. J Endourol. 2012;26:1085–8. https://doi.org/10.1089/end.2011.0670.
Kong SH, Oh BM, Yoon H, Ahn HS, Lee HJ, Chung SG, et al. Comparison of two- and three-dimensional camera systems in laparoscopic performance: a novel 3D system with one camera. Surg Endosc. 2010;24:1131–43. https://doi.org/10.1007/s00464-009-0740-8.
Sahu D, Mathew MJ, Reddy PK. 3D laparoscopy—help or hype; initial experience of a tertiary health centre. J Clin Diagn Res. 2014;8:13–5. https://doi.org/10.7860/JCDR/2014/8234.4543.
Aykan S, Singhal P, Nguyen DP, Yigit A, Tuken M, Yakut E, et al. Perioperative, pathologic, and early continence outcomes comparing three-dimensional and two-dimensional display systems for laparoscopic radical prostatectomy-a retrospective, single-surgeon study. J Endourol. 2014;28:539–43. https://doi.org/10.1089/end.2013.0630.
Kinoshita H, Nakagawa K, Usui Y, Iwamura M, Ito A, Miyajima A, et al. High-definition resolution three-dimensional imaging systems in laparoscopic radical prostatectomy: randomized comparative study with high-definition resolution two-dimensional systems. Surg Endosc. 2015;29:2203–9. https://doi.org/10.1007/s00464-014-3925-8.
Li Z, Li JP, Qin X, B Bin X, Han YD, Da LS, et al. Three-dimensional vs two-dimensional video assisted thoracoscopic esophagectomy for patients with esophageal cancer. World J Gastroenterol. 2015;21:10675–82. https://doi.org/10.3748/wjg.v21.i37.10675.
Velayutham V, Fuks D, Nomi T, Kawaguchi Y, Gayet B. 3D visualization reduces operating time when compared to high-definition 2D in laparoscopic liver resection: a case-matched study. Surg Endosc. 2016;30:147–53. https://doi.org/10.1007/s00464-015-4174-1.
Currò G, La Malfa G, Caizzone A, Rampulla V, Navarra G. Three-dimensional (3D) versus two-dimensional (2D) laparoscopic bariatric surgery: a Single-Surgeon Prospective Randomized Comparative Study. Obes Surg. 2015;25:2120–4. https://doi.org/10.1007/s11695-015-1674-y.
Currò G, Cogliandolo A, Bartolotta M, Navarra G. Three-dimensional versus two-dimensional laparoscopic right hemicolectomy. J Laparoendosc Adv Surg Tech. 2016;26:213–7. https://doi.org/10.1089/lap.2015.0557.
Currò G, La Malfa G, Lazzara S, Caizzone A, Fortugno A, Navarra G. Three-dimensional versus two-dimensional laparoscopic cholecystectomy: Is surgeon experience relevant? J Laparoendosc Adv Surg Tech. 2015;25:566–70. https://doi.org/10.1089/lap.2014.0641.
Tao K, Liu X, Deng M. Three-dimensional against 2-dimensional laparoscopic. 2016;26:324–7.
Lara-Domínguez MD, López-Jiménez A, Grabowski JP, Arjona-Berral JE, Zapardiel I. Prospective observational study comparing traditional laparoscopy and three-dimensional laparoscopy in gynecologic surgery. Int J Gynecol Obstet. 2017;136:320–4. https://doi.org/10.1002/ijgo.12078.
Raspagliesi F, Bogani G, Martnelli F, Signorelli M, Scaffa C, Sabatucci I, et al. 3D vision improves outcomes in early cervical cancer treated with laparoscopic type B radical hysterectomy and pelvic lymphadenectomy. Tumori. 2017;103:76–80. https://doi.org/10.5301/tj.5000572.
Agrusa A, di Buono G, Chianetta D, Sorce V, Citarrella R, Galia M, et al. Three-dimensional (3D) versus two-dimensional (2D) laparoscopic adrenalectomy: A case-control study. Int J Surg. 2016;28:S114–7. https://doi.org/10.1016/j.ijsu.2015.12.055.
Tang FJ, Qi L, Jiang HC, Tong SY, Li Y. Comparison of the clinical effectiveness of 3D and 2D imaging systems for laparoscopic radical cystectomy with pelvic lymph node dissection. J Int Med Res. 2016;44:613–9. https://doi.org/10.1177/0300060515621445.
Fanfani F, Rossitto C, Restaino S, Ercoli A, Chiantera V, Monterossi G, et al. How technology can impact surgeon performance: a randomized trial comparing 3-dimensional versus 2-dimensional laparoscopy in gynecology oncology. J Minim Invasive Gynecol. 2016;23:810–7. https://doi.org/10.1016/j.jmig.2016.03.020.
Kanaji S, Suzuki S, Harada H, Nishi M, Yamamoto M, Matsuda T, et al. Comparison of two- and three-dimensional display for performance of laparoscopic total gastrectomy for gastric cancer. Langenbeck's Arch Surg. 2017;402:493–500. https://doi.org/10.1007/s00423-017-1574-9.
Leon P, Rivellini R, Giudici F, Sciuto A, Pirozzi F, Corcione F. 3D vision provides shorter operative time and more accurate intraoperative surgical performance in laparoscopic hiatal hernia repair compared with 2D vision. Surg Innov. 2017;24:155–61. https://doi.org/10.1177/1553350616687434.
Zheng CH, Lu J, Zheng HL, Li P, Xie JW, Bin WJ, et al. Comparison of 3D laparoscopic gastrectomy with a 2D procedure for gastric cancer: a phase 3 randomized controlled trial. Surg (United States). 2018;163:300–4. https://doi.org/10.1016/j.surg.2017.09.053.
Lui MW, Cheung VYT. Three-dimensional versus two-dimensional laparoscopy for ovarian cystectomy: a prospective randomised study. Hong Kong Med J. 2018;24:245–51. https://doi.org/10.12809/hkmj176846.
Yoon J, Il KS, Kim MH, Kim MJ, Oh HK, Kim DW, et al. Comparison of short-term outcomes between 3D and 2D imaging laparoscopic colectomy with D3 lymphadenectomy for colon cancer. J Laparoendosc Adv Surg Tech. 2019;29:340–5. https://doi.org/10.1089/lap.2018.0317.
Wang Y, Chen W, Xia S, Wang T, Wang S, Zhang F, et al. Three-dimensional versus two-dimensional laparoscopic-assisted transanal pull-through for hirschsprung’s disease in children: preliminary results of a prospective cohort study in a tertiary hospital. J Laparoendosc Adv Surg Tech. 2019;29:557–63. https://doi.org/10.1089/lap.2018.0537.
Yang C, Mo L, Ma Y, Peng G, Ren Y, Wang W, et al. A comparative analysis of lung cancer patients treated with lobectomy via three-dimensional video-assisted thoracoscopic surgery versus two-dimensional resection. J Thorac Dis. 2015;7:1798–805. https://doi.org/10.3978/j.issn.2072-1439.2015.10.59.
Yang CL, Wang W, Mo LL, Zhang L, Peng GL, Yu ZW, et al. Short-term outcome of three-dimensional versus two-dimensional video-assisted thoracic surgery for benign pulmonary diseases. Ann Thorac Surg. 2016;101:1297–302. https://doi.org/10.1016/j.athoracsur.2015.10.042.
Jiao P, Wu QJ, Sun YG, Ma C, Tian WX, Yu HB, et al. Comparative study of three-dimensional versus two-dimensional video-assisted thoracoscopic two-port lobectomy. Thorac Cancer. 2017;8:3–7. https://doi.org/10.1111/1759-7714.12387.
Dong S, Yang XN, Zhong WZ, Nie Q, Liao RQ, Lin JT, et al. Comparison of three-dimensional and two-dimensional visualization in video-assisted thoracoscopic lobectomy. Thorac Cancer. 2016;7:530–4. https://doi.org/10.1111/1759-7714.12361.
Padin EM, Santos RS, Fernández SG, Jimenez AB, Fernández SE, Dacosta EC, et al. Impact of Three-Dimensional Laparoscopy in a Bariatric Surgery Program: Influence in the Learning Curve. Obes Surg. 2017;27:2552–6. https://doi.org/10.1007/s11695-017-2687-5.
Bagan P, De Dominicis F, Hernigou J, Dakhil B, Zaimi R, Pricopi C, et al. Complete thoracoscopic lobectomy for cancer: comparative study of three-dimensional high-definition with two-dimensional high-definition video systems. Interact Cardiovasc Thorac Surg. 2015;20:820–4. https://doi.org/10.1093/icvts/ivv031.
Komatsuda A, Matsumoto K, Miyajima A, Kaneko G, Mizuno R, Kikuchi E, et al. Technical improvement using a three-dimensional video system for laparoscopic partial nephrectomy. Asian Pac J Cancer Prev. 2016;17:2475–8. https://doi.org/10.7314/APJCP.2016.17.5.2475.
Abou-Haidar H, Al-Qaoud T, Jednak R, Brzezinski A, El-Sherbiny M, Capolicchio JP. Laparoscopic pyeloplasty: initial experience with 3D vision laparoscopy and articulating shears. J Pediatr Urol. 2016;12:426.e1–5. https://doi.org/10.1016/j.jpurol.2016.08.027.
Patankar SB, Padasalagi RG. Three-dimensional versus two-dimensional laparoscopy in urology: A randomized study. Indian J Urol. 2017;33:207–14. https://doi.org/10.4103/iju.IJU.
Bove P, Iacovelli V, Celestino F, De Carlo F, Vespasiani G, Agrò EF. 3D vs 2D laparoscopic radical prostatectomy in organ-confined prostate cancer: Comparison of operative data and pentafecta rates: A single cohort study. BMC Urol. 2015;15:4–11. https://doi.org/10.1186/s12894-015-0006-9.
Ruan Y, hai WX, Wang K, yang ZY, jie XS, D liang X. Clinical evaluation and technical features of three-dimensional laparoscopic partial nephrectomy with selective segmental artery clamping. World J Urol. 2016;34:679–85. https://doi.org/10.1007/s00345-015-1658-5.
Code Availability
Not applicable.
Funding
This study received no funding.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the design of this study, acquisition, and analysis of data. All the authors participated in revising it critically for intellectual content and for final version to be published.
Corresponding author
Ethics declarations
Ethics Approvals and Consent to Participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to Publication
The authors consent this study publication.
Conflicts of Interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Surgery
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Vilaça, J., de Azevedo, J.M., Louro, H.C. et al. Clinical Use of Third-Generation 3D Imaging Systems in Endoscopic Surgery—a Systematic Review. SN Compr. Clin. Med. 3, 879–896 (2021). https://doi.org/10.1007/s42399-021-00774-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-021-00774-x