Abstract
Background
Triglyceride-glucose (TyG) is correlated with cardiovascular events caused by insulin resistance (IR). The aim of this study was to analyze the relationship between TyG and its related indicators and IR among US adults from 2007 to 2018 in the National Health and Nutrition Examination Survey (NHANES) database so as to identify more accurate and reliable predictors of IR.
Methods
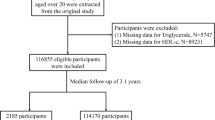
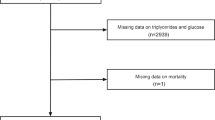
This is a cross-sectional study including 9884 participants (2255 with IR and 7629 without IR). TyG, TyG-body mass index (TyG-BMI), TyG waist circumference (TyG-WC), and TyG waist-to-height ratio (TyG-WtHR) were measured using standard formulas.
Results
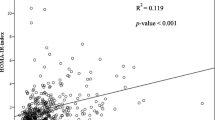
TyG, TyG-BMI, TyG-WC, and TyG-WtHR were significantly correlated with IR in the general population, with TyG-WC being the most strongly correlated, with an odds ratio of 8.00 (95% confidence interval 5.05–12.67) for the fourth quartile of TyG-WC compared with the first quartile in the adjusted model. Receiver operating characteristic (ROC) analysis of the participants showed that the maximum area under the TyG-WC curve was 0.8491, which was significantly higher than that of the other three indicators. Moreover, this trend was stable both among people of both genders and among patients with coronary heart disease (CHD), hypertension, and diabetes.
Conclusions
The present study confirms that the TyG-WC index is more successful than TyG alone in identifying IR. In addition, our findings demonstrate that TyG-WC is a simple and effective marker for screening the general US adult population and those with CHD, hypertension, and diabetes and can be effectively used in clinical practice.



Similar content being viewed by others
Data availability
The data that support the findings of this study are openly available in NHANES at [https://www.cdc.gov/nchs/NHANES/].
References
Kolka CM, Bergman RN (2013) The endothelium in diabetes: its role in insulin access and diabetic complications. Rev Endocr Metab Disord 14:13–19. https://doi.org/10.1007/s11154-012-9233-5
Dimitriadis G, Mitrou P, Lambadiari V, Maratou E, Raptis SA (2011) Insulin effects in muscle and adipose tissue. Diabetes Res Clin Pract 93(Suppl 1):S52–S59. https://doi.org/10.1016/S0168-8227(11)70014-6
Ye J (2021) Mechanism of insulin resistance in obesity: a role of ATP. Front Med 15:372–382. https://doi.org/10.1007/s11684-021-0862-5
Neeland IJ, Poirier P, Després JP (2018) Cardiovascular and Metabolic Heterogeneity of Obesity: Clinical Challenges and Implications for Management. Circulation 137:1391–1406. https://doi.org/10.1161/circulationaha.117.029617
Tam CS, Xie W, Johnson WD, Cefalu WT, Redman LM, Ravussin E (2012) Defining insulin resistance from hyperinsulinemic-euglycemic clamps. Diabetes Care 35:1605–1610. https://doi.org/10.2337/dc11-2339
Zimmet P, Alberti KG, Shaw J (2001) Global and societal implications of the diabetes epidemic. Nature 414:782–787. https://doi.org/10.1038/414782a
da Silva AA, do Carmo JM, Li X, Wang Z, Mouton AJ, Hall JE (2020) Role of Hyperinsulinemia and Insulin Resistance in Hypertension: Metabolic Syndrome Revisited. Can J Cardiol 36:671–682. https://doi.org/10.1016/j.cjca.2020.02.066
Hill MA, Yang Y, Zhang L, Sun Z, Jia G, Parrish AR, Sowers JR (2021) Insulin resistance, cardiovascular stiffening and cardiovascular disease. Metabolism 119:154766. https://doi.org/10.1016/j.metabol.2021.154766
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, Chen J, He J (2016) Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation 134:441–450. https://doi.org/10.1161/circulationaha.115.018912
GBD (2017) DALYs and HALE Collaborators (2018) Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392:1859–1922. https://doi.org/10.1016/s0140-6736(18)32335-3
Caballero B (2019) Humans against Obesity: Who Will Win? Adv Nutr 10:S4–S9. https://doi.org/10.1093/advances/nmy055
DeFronzo RA, Tobin JD, Andres R (1979) Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol 237:E214-223. https://doi.org/10.1152/ajpendo.1979.237.3.E214
Du T, Yuan G, Zhang M, Zhou X, Sun X, Yu X (2014) Clinical usefulness of lipid ratios, visceral adiposity indicators, and the triglycerides and glucose index as risk markers of insulin resistance. Cardiovasc Diabetol 13:146. https://doi.org/10.1186/s12933-014-0146-3
Miller WG, Thienpont LM, Van Uytfanghe K, Clark PM, Lindstedt P, Nilsson G, Steffes MW (2009) Toward standardization of insulin immunoassays. Clin Chem 55:1011–1018. https://doi.org/10.1373/clinchem.2008.118380
He J, He S, Liu K, Wang Y, Shi D, Chen X (2014) The TG/HDL-C Ratio Might Be a Surrogate for Insulin Resistance in Chinese Nonobese Women. Int J Endocrinol 2014:105168. https://doi.org/10.1155/2014/105168
Lu YW, Chang CC, Chou RH, Tsai YL, Liu LK, Chen LK, Huang PH, Lin SJ (2021) Gender difference in the association between TyG index and subclinical atherosclerosis: results from the I-Lan Longitudinal Aging Study. Cardiovasc Diabetol 20:206. https://doi.org/10.1186/s12933-021-01391-7
Park K, Ahn CW, Lee SB, Kang S, Nam JS, Lee BK, Kim JH, Park JS (2019) Elevated TyG Index Predicts Progression of Coronary Artery Calcification. Diabetes Care 42:1569–1573. https://doi.org/10.2337/dc18-1920
Alizargar J, Bai CH, Hsieh NC, Wu SV (2020) Use of the triglyceride-glucose index (TyG) in cardiovascular disease patients. Cardiovasc Diabetol 19:8. https://doi.org/10.1186/s12933-019-0982-2
Chen TC, Clark J, Riddles MK, Mohadjer LK, Fakhouri THI (2020) National Health and Nutrition Examination Survey, 2015–2018: Sample Design and Estimation Procedures. Vital Health Stat 2:1–35. https://pubmed.ncbi.nlm.nih.gov/33663649/. Accessed April 2020
Ehrampoush E, MirzayRazzaz J, Arjmand H, Ghaemi A, RaeisiShahraki H, EbrahimBabaei A, Osati S, Homayounfar R (2021) The association of vitamin D levels and insulin resistance. Clin Nutr ESPEN 42:325–332. https://doi.org/10.1016/j.clnesp.2021.01.012
Lamprea-Montealegre JA, Staplin N, Herrington WG, Haynes R, Emberson J, Baigent C, de Boer IH, SHARP Collaborative Group (2020) Apolipoprotein B, Triglyceride-Rich Lipoproteins, and Risk of Cardiovascular Events in Persons with CKD. Clin J Am Soc Nephrol 15:47–60. https://doi.org/10.2215/CJN.07320619
Zhao J, Fan H, Wang T, Yu B, Mao S, Wang X, Zhang W, Wang L, Zhang Y, Ren Z, Liang B (2022) TyG index is positively associated with risk of CHD and coronary atherosclerosis severity among NAFLD patients. Cardiovasc Diabetol 21:123. https://doi.org/10.1186/s12933-022-01548-y
Zheng S, Shi S, Ren X, Han T, Li Y, Chen Y, Liu W, Hou PC, Hu Y (2016) Triglyceride glucose-waist circumference, a novel and effective predictor of diabetes in first-degree relatives of type 2 diabetes patients: cross-sectional and prospective cohort study. J Transl Med 14:260. https://doi.org/10.1186/s12967-016-1020-8
Song S, Son DH, Baik SJ, Cho WJ, Lee YJ (2022) Triglyceride Glucose-Waist Circumference (TyG-WC) Is a Reliable Marker to Predict Non-Alcoholic Fatty Liver Disease. Biomedicines 10:2251. https://doi.org/10.3390/biomedicines10092251
Nkemjika S, Ifebi E, Cowan LT, Chun-Hai Fung I, Twum F, Liu F, Zhang J (2020) Association between serum folate and cardiovascular deaths among adults with hypertension. Eur J Clin Nutr 74:970–978. https://doi.org/10.1038/s41430-019-0533-7
Taylor R (2013) Type 2 diabetes: etiology and reversibility. Diabetes Care 36:1047–1055. https://doi.org/10.2337/dc12-1805
Ren X, Chen ZA, Zheng S, Han T, Li Y, Liu W, Hu Y (2016) Association between Triglyceride to HDL-C Ratio (TG/HDL-C) and Insulin Resistance in Chinese Patients with Newly Diagnosed Type 2 Diabetes Mellitus. PLoS One 11:e0154345. https://doi.org/10.1371/journal.pone.0154345
Kang HT, Yoon JH, Kim JY, Ahn SK, Linton JA, Koh SB, Kim JK (2012) The association between the ratio of triglyceride to HDL-C and insulin resistance according to waist circumference in a rural Korean population. Nutr Metab Cardiovasc Dis 22:1054–1060. https://doi.org/10.1016/j.numecd.2011.01.013
Irace C, Carallo C, Scavelli FB, De Franceschi MS, Esposito T, Tripolino C, Gnasso A (2013) Markers of insulin resistance and carotid atherosclerosis. A comparison of the homeostasis model assessment and triglyceride glucose index. Int J Clin Pract 67:665–672. https://doi.org/10.1111/ijcp.12124
Hukportie DN, Li FR, Zhou R, Zheng JZ, Wu XX, Wu XB (2021) Anthropometric Measures and Incident Diabetic Nephropathy in Participants With Type 2 Diabetes Mellitus. Front Endocrinol (Lausanne) 12:706845. https://doi.org/10.3389/fendo.2021.706845
Raghavan S, Pachucki MC, Chang Y, Porneala B, Fox CS, Dupuis J, Meigs JB (2016) Incident Type 2 Diabetes Risk is Influenced by Obesity and Diabetes in Social Contacts: a Social Network Analysis. J Gen Intern Med 31:1127–1133. https://doi.org/10.1007/s11606-016-3723-1
Matsuda M, Shimomura I (2013) Increased oxidative stress in obesity: implications for metabolic syndrome, diabetes, hypertension, dyslipidemia, atherosclerosis, and cancer. Obes Res Clin Pract 7:e330–e341. https://doi.org/10.1016/j.orcp.2013.05.004
Ashwell M, Gunn P, Gibson S (2012) Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev 13:275–286. https://doi.org/10.1111/j.1467-789X.2011.00952.x
Petermann-Rocha F, Ulloa N, Martínez-Sanguinetti MA, Leiva AM, Martorell M, Villagrán M, Troncoso-Pantoja C, Ho FK, Celis-Morales C, Pizarro A (2020) Is waist-to-height ratio a better predictor of hypertension and type 2 diabetes than body mass index and waist circumference in the Chilean population? Nutrition 79–80:110932. https://doi.org/10.1016/j.nut.2020.110932
Lim J, Kim J, Koo SH, Kwon GC (2019) comparison of triglyceride glucose index, and related parameters to predict insulin resistance in korean adults: an analysis of the 2007–2010 korean national health and nutrition examination survey. PLoS One 14:e0212963. https://doi.org/10.1371/journal.pone.0212963
Lee DH, Keum N, Hu FB, Orav EJ, Rimm EB, Willett WC, Giovannucci EL (2018) Predicted lean body mass, fat mass, and all cause and cause specific mortality in men: prospective US cohort study. Bmj 362:k2575. https://doi.org/10.1136/bmj.k2575
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval
As the data were obtained from a public database, ethical approval was waived.
Informed consent
Not applicable to this study as the data source for this study is a public database.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yan, S., Wang, D. & Jia, Y. Comparison of insulin resistance-associated parameters in US adults: a cross-sectional study. Hormones 22, 331–341 (2023). https://doi.org/10.1007/s42000-023-00448-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-023-00448-4