Key summary points
To investigate whether two factors, malnutrition and cachexia, affect swallowing function, activities of daily living, and death in sarcopenic dysphagia.
AbstractSection FindingsFour percent of patients with sarcopenic dysphagia were found to have cachexia according to the Asian Working Group for Cachexia criteria. No significant difference in changes in the Food Intake Level Scale and Barthel Index between the malnutrition and cachexia group and the other groups, however death increased significantly.
AbstractSection MessageAssessment of both cachexia and malnutrition is important in sarcopenic dysphagia.
Abstract
Purpose
To investigate whether two factors, malnutrition and cachexia, affect swallowing function, activities of daily living (ADL), and death in sarcopenic dysphagia.
Methods
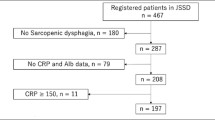
Of 467 patients enrolled in the Japanese Sarcopenic Dysphagia Database, 271 met the study eligibility criteria in a retrospective cohort study. Patients were divided into four groups based on whether they had cachexia according to the Asian Working Group for Cachexia (AWGC) criteria and malnutrition according to the Global Leadership Initiative on Malnutrition (GLIM) criteria. Multivariate analyses were performed to investigate the differences in changes in the Food Intake LEVEL Scale (FILS) and Barthel Index (BI) and death after follow-up between the malnutrition and cachexia group and the other groups.
Results
The mean age was 83.7 ± 8.3 years, 119 (44%) were men and 152 (56%) were women. The median FILS at baseline was 7 and the median BI was 25. A total of 120 (44%) had malnutrition only, 54 (20%) had neither cachexia nor malnutrition, 12 (4%) had cachexia only, and 85 (31%) had both cachexia and malnutrition. Multivariate analyses showed no significant difference between the change in BI (P = 0.688) and the change in FILS (P = 0.928) between the malnutrition and cachexia group and the other groups; however, death increased significantly (P = 0.010).
Conclusion
Some patients diagnosed with cachexia were not malnourished, although many patients with cachexia were malnourished. While patients with both cachexia and malnutrition did not show significant improvement in ADL and swallowing function compared with patients without both conditions, the number of deaths increased significantly.

Similar content being viewed by others
References
Wakabayashi H, Kishima M, Itoda M, Fujishima I, Kunieda K, Ohno T et al (2021) Diagnosis and treatment of sarcopenic dysphagia: a scoping review. Dysphagia 36:523–531. https://doi.org/10.1007/s00455-021-10266-8
Fujishima I, Fujiu-Kurachi M, Arai H, Hyodo M, Kagaya H, Maeda K et al (2019) Sarcopenia and dysphagia: position paper by four professional organizations. Geriatr Gerontol Int 19:91–97. https://doi.org/10.1111/ggi.13591
Bauer J, Morley JE, Schols AMWJ, Ferrucci L, Cruz-Jentoft AJ, Dent E et al (2019) Sarcopenia: a time for action. An SCWD position paper. J Cachexia Sarcopenia Muscle 10:956–961. https://doi.org/10.1002/jcsm.12483
Abu-Ghanem S, Graf A, Govind J (2022) Diagnosis of sarcopenic dysphagia in the elderly: critical review and future perspectives. Dysphagia 37:1093–1102. https://doi.org/10.1007/s00455-021-10371-8
Nagai T, Wakabayashi H, Nishioka S, Momosaki R (2022) Functional prognosis in patients with sarcopenic dysphagia: An observational cohort study from the Japanese sarcopenic dysphagia database. Geriatr Gerontol Int 22:839–845. https://doi.org/10.1111/ggi.14466
Taguchi K, Wakabayashi H, Fujimoto M, Obayashi S, Yamamoto M, Nishioka S et al (2022) Association between Malnutrition severity and swallowing function in convalescent rehabilitation wards: a multi-center cohort study in malnourished patients with sarcopenic dysphagia. J Nutr Health Aging 26:469–476. https://doi.org/10.1007/s12603-022-1782-z
Matsuo H, Sakuma K (2022) Pathophysiology of cachexia and characteristics of dysphagia in chronic diseases. Asia Pac J Oncol Nurs 22(9):100120. https://doi.org/10.1016/j.apjon.2022.100120
Wakabayashi H (2023) Hospital-associated sarcopenia, acute sarcopenia, and iatrogenic sarcopenia: prevention of sarcopenia during hospitalization. J Gen Fam Med 24:146–147. https://doi.org/10.1002/jgf2.625
Sato Y, Yoshimura Y, Abe T, Nagano F, Matsumoto A (2023) Hospital-associated sarcopenia and the preventive effect of high energy intake along with intensive rehabilitation in patients with acute stroke. Nutrition 116:112181. https://doi.org/10.1016/j.nut.2023.112181
Maeda K, Ishida Y, Nonogaki T, Shimizu A, Yamanaka Y et al (2019) Development and predictors of sarcopenic dysphagia during hospitalization of older adults. Nutrients 12:70. https://doi.org/10.3390/nu12010070
Mukundan M, Kashyap K, Dhar M, Muralidharan A, Agarwal D, Saxena Y (2022) Nutritional and functional status as a predictor of short-term mortality in hospitalized elderly patients in a tertiary care hospital. Cureus 24(14):e22576. https://doi.org/10.7759/cureus.22576
Zopf Y, Schink K, Reljic D, Herrmann HJ, Dieterich W, Kiesswetter E et al (2020) Assessing cachexia in older patients: different definitions - But which one is the most practical for clinical routine? Arch Gerontol Geriatr 86:103943. https://doi.org/10.1016/j.archger.2019.103943
Arai H, Maeda K, Wakabayashi H, Naito T, Konishi M, Assantachai P et al (2023) Diagnosis and outcomes of cachexia in Asia: working consensus report from the asian working group for cachexia. J Cachexia Sarcopenia Muscle 14:1949–1958. https://doi.org/10.1002/jcsm.13323
Beaudart C, Sanchez-Rodriguez D, Locquet M, Reginster JY, Lengelé L, Bruyère O (2019) Malnutrition as a strong predictor of the onset of sarcopenia. Nutrients 11:2883. https://doi.org/10.3390/nu11122883
Zhang X, Tang M, Zhang Q, Zhang KP, Guo ZQ, Xu HX et al (2021) The GLIM criteria as an effective tool for nutrition assessment and survival prediction in older adult cancer patients. Clin Nutr 40:1224–1232. https://doi.org/10.1016/j.clnu.2020.08.004
Mizuno S, Wakabayashi H, Fujishima I, Kishima M, Itoda M, Yamakawa M et al (2021) Construction and quality evaluation of the japanese sarcopenic dysphagia database. J Nutr Health Aging 25:926–932. https://doi.org/10.1007/s12603-021-1646-y
Kunieda K, Ohno T, Fujishima I, Hojo K, Morita T (2013) Reliability and validity of a tool to measure the severity of dysphagia: the Food Intake LEVEL Scale. J Pain Symptom Manage 46:201–206. https://doi.org/10.1016/j.jpainsymman.2012.07.020
Wakabayashi H (2014) Presbyphagia and sarcopenic dysphagia: association between aging, sarcopenia, and deglutition disorders. J Frailty Aging 3:97–103. https://doi.org/10.14283/jfa.2014.8
Mori T, Fujishima I, Wakabayashi H et al (2017) Development and reliability of a diagnostic algorithm for sarcopenic dysphagia. JCSM Clinical Reports 2:e00017. https://doi.org/10.17987/jcsm-cr.v2i2.17
Maeda K, Koga T, Nasu T, Takaki M, Akagi J (2017) Predictive accuracy of calf circumference measurements to detect decreased skeletal muscle mass and european society for clinical nutrition and metabolism-defined malnutrition in hospitalized older patients. Ann Nutr Metab 71:10–15. https://doi.org/10.1159/000478707
Maeda K, Akagi J (2015) Decreased tongue pressure is associated with sarcopenia and sarcopenic dysphagia in the elderly. Dysphagia 30:80–87. https://doi.org/10.1007/s00455-014-9577-y
Buehring B, Hind J, Fidler E, Krueger D, Binkley N, Robbins J (2013) Tongue strength is associated with jumping mechanography performance and handgrip strength but not with classic functional tests in older adults. J Am Geriatr Soc 61:418–422. https://doi.org/10.1111/jgs.12124
Jensen GL, Cederholm T, Correia MITD, Gonzalez MC, Fukushima R, Higashiguchi T et al (2019) GLIM criteria for the diagnosis of malnutrition: a consensus report from the global clinical nutrition community. JPEN J Parenter Enteral Nutr 43:32–40. https://doi.org/10.1002/jpen.1440
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel index. Md State Med J 14:61–65
Correia MITD, Tappenden KA, Malone A, Prado CM, Evans DC, Sauer AC, Hegazi R, Gramlich L et al (2022) Utilization and validation of the global leadership initiative on malnutrition (GLIM): a scoping review. Clin Nutr 41:687–697. https://doi.org/10.1016/j.clnu.2022.01.018
Joaquín C, Alonso N, Lupón J, Gastelurrutia P, Pérez-Monstesdeoca A, Domingo M et al (2022) Nutritional status according to the GLIM criteria in patients with chronic heart failure: association with prognosis. Nutrients 14:2244. https://doi.org/10.3390/nu14112244
Bullock AF, Greenley SL, McKenzie GAG, Paton LW, Johnson MJ (2020) Relationship between markers of malnutrition and clinical outcomes in older adults with cancer: systematic review, narrative synthesis and meta-analysis. Eur J Clin Nutr 74:1519–1535. https://doi.org/10.1038/s41430-020-0629-0
Arends J, Strasser F, Gonella S, Solheim TS, Madeddu C, Ravasco P et al (2021) Cancer cachexia in adult patients: ESMO clinical practice guidelines. ESMO Open 6:100092. https://doi.org/10.1016/j.esmoop.2021.100092
Campo-Rivera N, Ocampo-Chaparro JM, Carvajal-Ortiz R, Reyes-Ortiz CA (2022) Sarcopenic dysphagia is associated with mortality in institutionalized older adults. J Am Med Dir Assoc 23:1720.e11-1720.e17. https://doi.org/10.1016/j.jamda.2022.06.016
Matsuo H, Sakuma K (2022) Pathophysiology of cachexia and characteristics of dysphagia in chronic diseases. Asia Pac J Oncol Nurs 9:100120. https://doi.org/10.1016/j.apjon.2022.100120
Morishita T, Uzui H, Sato Y, Mitsuke Y, Tada H (2021) Associations between cachexia and metalloproteinases, haemodynamics and mortality in heart failure. Eur J Clin Invest 51:e13426. https://doi.org/10.1111/eci.13426
Wakabayashi H, Takahashi R, Murakami T (2019) The prevalence and prognosis of sarcopenic dysphagia in patients who require dysphagia rehabilitation. J Nutr Health Aging 23:84–88. https://doi.org/10.1007/s12603-018-1117-2
Shimizu A, Fujishima I, Maeda K, Wakabayashi H, Nishioka S, Ohno T et al (2021) Nutritional management enhances the recovery of swallowing ability in older patients with sarcopenic dysphagia. Nutrients 13:596. https://doi.org/10.3390/nu13020596
Kakehi S, Isono E, Wakabayashi H, Shioya M, Ninomiya J, Aoyama Y et al (2023) Sarcopenic dysphagia and simplified rehabilitation nutrition care process: an update. Ann Rehabil Med 47:337–347. https://doi.org/10.5535/arm.23101
Hansen T, Nielsen RL, Houlind MB, Tavenier J, Rasmussen LJH, Jørgensen LM et al (2021) Dysphagia prevalence, time course, and association with probable sarcopenia, inactivity, malnutrition, and disease status in older patients admitted to an emergency department: a secondary analysis of cohort study Data. Geriatrics 6(2):46. https://doi.org/10.3390/geriatrics6020046
Maeda K, Ishida Y, Nonogaki T, Shimizu A, Yamanaka Y, Matsuyama R et al (2020) Development and predictors of sarcopenic dysphagia during hospitalization of older adults. Nutrients 12:70. https://doi.org/10.3390/nu12010070
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T et al (2019) Writing group for the european working group on sarcopenia in older people 2 (EWGSOP2), and the extended group for EWGSOP2. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31. https://doi.org/10.1093/ageing/afy169
Mori T, Wakabayashi H, Kishima M, Itoda M, Fujishima I, Kunieda K et al (2022) Association between Inflammation and functional outcome in patients with sarcopenic dysphagia. J Nutr Health Aging 26:400–406. https://doi.org/10.1007/s12603-022-1769-9
Ueshima J, Momosaki R, Shimizu A, Motokawa K, Sonoi M, Shirai Y et al (2021) Nutritional assessment in adult patients with dysphagia: a scoping review. Nutrients 13:778. https://doi.org/10.3390/nu13030778
Homem SG, Moreira EAM, da Silva AF, Barni GC, da Rosa JS, Oliveira DL et al (2020) Relationship between oropharyngeal dysphagia, nutritional status, antioxidant vitamins and the inflammatory response in adults and elderly: a cross-sectional study. Clin Nutr ESPEN 38:211–217. https://doi.org/10.1016/j.clnesp.2020.04.011
Acknowledgements
We thank the Rehabilitation Nutrition Database Committee of the Japanese Association of Rehabilitation Nutrition and the Japanese Working Group on Sarcopenic Dysphagia that constructed the Japanese sarcopenic dysphagia database used in this study.
Funding
This work was supported by JSPS KAKENHI (19H03979).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
The study was approved by the Ethics Committee of Yokohama City University Medical Center (B190700074) and was conducted in accordance with the ethical standards of the Declaration of Helsinki of 1964 and its subsequent amendments.
Informed consent
All participants provided informed consent prior to enrollment or were given the right to opt out of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yamanaka, M., Wakabayashi, H., Nishioka, S. et al. Malnutrition and cachexia may affect death but not functional improvement in patients with sarcopenic dysphagia. Eur Geriatr Med (2024). https://doi.org/10.1007/s41999-024-00984-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s41999-024-00984-1