Key summary points
To use a clustering method with no preconceived ideas to identify older fallers living in the community and thus to suggest appropriate treatment plans.
AbstractSection Findingswe found three different functional clusters: (i) a low-mobility cluster of individuals who had difficulty getting up from the floor unaided and needed a mobility aid for walking, (ii) an intermediate group of rather sedentary individuals with a high body mass index and a gait speed of ~ 0.6 m s-1, and (iii) active participants who performed well in physical tests.
AbstractSection MessageThe population of older fallers referred for a multidisciplinary geriatric consultation is heterogeneous; when combined with simple tests, the presence of certain clinical characteristics can contribute to determine the most appropriate pathways.
Abstract
Objectives
The population of older adults is particularly heterogeneous with regard to frailty and the risk of falling, the two of which are linked. We conducted an exploratory, analysis (with no preconceived ideas) of data collected during multidisciplinary falls consultations (MFCs), to identify people with similar profiles.
Materials and methods
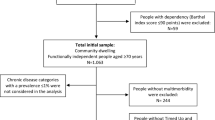
We performed an observational, multicentre study of older patients (aged 75 and over) having been evaluated in an MFC. We excluded adults with a Mini Mental State Examination score < 14/30, an activities of daily living score < 4/6, or an unstable medical condition. Each participant underwent a clinical interview, impedancemetry, and a physical activity assessment (a questionnaire, and use of an activity tracker on 5 consecutive days). The K-means method and ascending hierarchical clustering were used to identify clusters of people with common characteristics.
Results
Of the 106 participants, the median [IQR] mean number of falls in the previous 6 months was 1 [2]. Three functional clusters were identified: (i) fallers with poor mobility, difficulty getting up off the ground after a fall, and using a mobility aid for walking; (ii) an intermediate sedentary group with a gait speed of ~ 0.6 m s−1, and (iii) active people with a timed “up and go” test time below 15 s and a gait speed above 0.8 m s−1.
Conclusions
The population of older fallers referred for an MFC is heterogeneous. The presence of certain clinical characteristics enabled the definition of three patient clusters, which might help physicians to determine the most appropriate care objectives and pathways.

Similar content being viewed by others
Data availability
The data are available by contacting the principal author as the data are at the Orléans hospital centre.
References
Montero-Odasso M, Van der Velde N, Martin FC et al (2022) World guidelines for falls prevention and management for older adults: a global initiative. Age Ageing 51:1–36. https://doi.org/10.1093/ageing/afac205
Blain H, Bloch F, Borel L et al (2015) Activité physique et prévention des chutes chez les personnes âgées. Doctoral dissertation, Institut national de la santé et de la recherche médicale (INSERM), Paris: Inserm: Editions EDP Sciences (ISSN: 1264-1782)/518.p.ffinserm-02102899f
Ensrud K, Ewing S, Taylor B et al (2007) Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci 62(7):744–751
Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society (2011) Summary of the updated American geriatrics society/British geriatrics society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 59(1):148–157
Clemson L, Cumming RG, Kendig H et al (2004) The effectiveness of a community-based program for reducing the incidence of falls in the elderly: a randomized trial. J Am Geriatr Soc 52(9):1487–1494
Tinetti M-E, Baker D, Mcavay G et al (1994) A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med 331(13):821–827
Hogan D, Macdonald F, Betts J et al (2001) A randomized controlled trial of a community-based consultation service to prevent falls. CMAJ 165(5):537–543
Chang J, Morton S, Rubenstein L et al (2004) Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. BMJ 328:680–687
Folstein MF, Folstein S, Mc Huth PR (1975) Mini mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Katz S (1983) Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc 31(12):721–727
Delbaere K, Hauer K, Lord SR (2010) Evaluation of the incidental and planned activity questionnaire (IPEQ) for older people. Br J Sports Med 44:1029–1034
Beauchet O, Berrut G (2006) Marche et double tâche: définition, intérêts et perspectives chez le sujet âgé. Psychol Neuropsychiatr Vieil 4(3):215–225
Podsialo D, Richardson S (1991) The timed up and go: a test of basic functionnal mobility for frail elderly persons. J Am Geriatr Soc 39:142–148
Guralnik JM, Simonsick EM, Ferrucci L et al (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49:M85-94
Hamer M, Stamatakis E (2013) Screen-based sedentary behavior, physical activity, and muscle strength in the English longitudinal study of ageing. PLoS ONE 8(6):e66222
Clement J, Nassif R, Leger J et al (1997) Development and contribution to the validation of a brief French version of the yesavage geriatric depression scale. L’encephale 23(2):91–99
Vellas B, Guigoz Y, Garry PJ et al (1999) The Mini Nutritional assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition 15(2):116–122
Charlson M, Szatrowski TP, Peterson J et al (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251
Inouye S, Studenski S, Tinetti M et al (2007) Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc 55(5):780–791
R Core Team (2021) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Dargent-Molina P, Breart G (1995) Epidemiology of falls and fall-related injuries in the aged. Rev Epidemiol Sante Publique 43(1):72–83
Tinetti M, Liu WI, Noel EB (1993) Predictors and prognosis of inability to get up after falls among elderly persons. JAMA 269(1):65–70
Tournadre A, Vial G, Capel F et al (2019) La sarcopénie. Rev Rhum 86(1):39–45
Rashedi V, Iranpour A, Mohseni M et al (2019) Risk factors for fall in elderly with diabetes mellitus type 2. Diabetes Metab Syndr 13(4):2347–2351
Schwartz A, Hillier T, Sellmeyer D et al (2002) Older women with diabetes have a higher risk of falls: a prospective study. Diabetes Care 25(10):1749–1754
Clegg A, Young J, Iliffe S et al (2013) Frailty in elderly people. Lancet 381(9868):752–762
Castelle MV, Sanchez M, Julian R et al (2013) Frailty prevalence and slow walking speed in persons age 65 ans older, implication for primary care. BMC Fam Pract 19(14):86
Author information
Authors and Affiliations
Contributions
All authors conceived and designed the study. Dr MP, Dr JBG and Dr AV prepared material and collected and analyzed data. The first draft of the manuscript was written by Dr MP, and all authors commented on and revised subsequent versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest with regard to the present study.
Ethical approval
The protocol was approved by the independent ethics committee at Orleans University Hospital (Orléans, France; reference: 2016-02, dated April 26, 2001) and the French National Consultative Committee on Information Processing in Medical Research at the French Ministry of Research (Paris, France; reference: 16.522, dated July 12, 2016).
Informed consent
All participants were given comprehensive written and verbal information on the study’s objectives and procedures, the right to refuse to participate, and the ability to withdraw from the study at any time.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pambet, M., Gauvain, J.B., Valery, A. et al. Use of a clustering method to describe the clinical profiles of older fallers: the value of a multidisciplinary consultation. Eur Geriatr Med 14, 1097–1104 (2023). https://doi.org/10.1007/s41999-023-00829-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-023-00829-3