Key summary points
To evaluate sarcopenia risk in hospitalized older patients.
AbstractSection FindingsThe percentage of patients at risk of sarcopenia defined by the SARC-F was 48.8%. Sarcopenia risk was associated with unfavorable health care outcomes including dependency, malnutrition, and dysphagia.
AbstractSection MessageSarcopenia risk is related with unfavorable outcomes in hospitalized patients and it is important to recognize sarcopenia at an early stage and to prevent its progression, before dependency develops.
Abstract
Purpose
To investigate the risk of sarcopenia in hospitalized older patients and to assess the associations between sarcopenia risk and health care outcomes including dependency, malnutrition, and dysphagia.
Methods
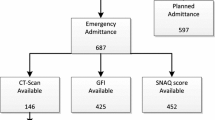
This multicenter cross-sectional study was a part of the annual National Prevalence Measurement of Quality of Care (LPZ) in Turkey. Hospitalized patients age 65 and older were included in the study. The SARC-F was used to assess risk of sarcopenia. Dependency was appraised according to the Care Dependency Scale (CDS). Nutritional status was established with respect to the Malnutrition Universal Screening Tool (MUST). Dysphagia was screened by two structured questions.
Results
A total of 492 patients were included in the analysis. Two hundred and forty patients (48.8%) were at risk of sarcopenia. Sarcopenia risk was more prevalent among women (p = 0.007) and patients with risk of sarcopenia were older (p < 0.001). Hospital stay was longer and malnutrition and dysphagia were more prevalent in patients with sarcopenia risk than without (all p < 0.001). All nutritional interventions were applied mostly to patients with sarcopenia risk than without. In multivariate analysis, advanced age (OR: 1.068, CI 1.032–1.104, p < 0.001), female gender (OR: 2.414, CI 1.510–3.857, p < 0.001), and dependency (OR: 5.022, CI 2.922–8.632, p < 0.001) were independently associated with sarcopenia risk.
Conclusions
Sarcopenia risk is related with unfavorable outcomes in hospitalized patients. Primarily older female patients are at risk for sarcopenia. It is important to recognize sarcopenia at an early stage and to prevent its progression, before dependency develops. The SARC-F may be a useful tool for screening sarcopenia risk in hospitalized patients.




Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Cruz-Jentoft AJ, Baeyens JP, Bauer JM et al (2010) Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing 39:412–423
Cao L, Chen S, Zou C et al (2014) A pilot study of the SARC-F scale on screening sarcopenia and physical disability in the Chinese older people. J Nutr Health Aging 18:277–283
Cao L, Morley JE (2016) Sarcopenia is recognized as an independent condition by an international classification of disease, tenth revision, clinical modification (ICD-10-CM) code. J Am Med Dir Assoc 17:675–677
Borges TC, Gomes TLN, Pimentel GD (2019) Sarcopenia as a predictor of nutritional status and comorbidities in hospitalized patients with cancer: a cross-sectional study. Nutrition 73:110703
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31
Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE (2016) SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle 7:28–36
Bahat G, Yilmaz O, Kılıç C, Oren M, Karan MA (2018) Performance of SARC-F in regard to sarcopenia definitions, muscle mass and functional measures. J Nutr Health Aging 22:898–903
Bastijns S, Bauer J, Cruz-Jentoft AJ et al. Acute sarcopenia in hospitalized elderly: assessment through ultrasound. clinicaltrials.gov
Gariballa S, Alessa A (2013) Sarcopenia: prevalence and prognostic significance in hospitalized patients. Clin Nutr 32:772–776
Morandi A, Onder G, Fodri L et al (2015) The association between the probability of sarcopenia and functional outcomes in older patients undergoing in-hospital rehabilitation. J Am Med Dir Assoc 16:951–956
Vetrano DL, Landi F, Volpato S, Corsonello A, Meloni E, Bernabei R, Onder G (2014) Association of sarcopenia with short- and long-term mortality in older adults admitted to acute care wards: results from the CRIME study. J Gerontol A Biol Sci Med Sci 69:1154–1161
Tang T, Wu L, Yang L et al (2018) A sarcopenia screening test predicts mortality in hospitalized older adults. Sci Rep 8:2923
Yoshimura Y, Wakabayashi H, Bise T, Tanoue M (2018) Prevalence of sarcopenia and its association with activities of daily living and dysphagia in convalescent rehabilitation ward inpatients. Clin Nutr 37:2022–2028
van Nie-Visser NC, Schols JM, Meesterberends E, Lohrmann C, Meijers JM, Halfens RJ (2013) An international prevalence measurement of care problems: study protocol. J Adv Nurs 69:e18-29
Dijkstra A, Hakverdioğlu G, Korhan EA, Muszalik M, Kędziora-Kornatowska K, Suzuki M (2012) The care dependency scale for measuring basic human needs: an international comparison. J Adv Nurs 68:2341–2816
Stratton RJ, Hackston A, Longmore D et al (2004) Malnutrition in hospital outpatients and inpatients: prevalence, concurrent validity and ease of use of the ‘malnutrition universal screening tool’ (‘MUST’) for adults. Br J Nutr 92:799–808
Huppertz VAL, Halfens RJG, van Helvoor A et al (2018) Association between oropharyngeal dysphagia and malnutrition in Dutch nursing home residents: results of the national prevalence measurement of quality of care. J Nutr Health Aging 22:1246–1252
Tanaka S, Kamiya K, Hamazaki N et al (2017) Utility of SARC-F for assessing physical function in elderly patients with cardiovascular disease. J Am Med Dir Assoc 18:176–181
Ozsurekci C, Arslan SS, Demir N et al (2020) Timing of dysphagia screening in Alzheimer’s dementia. JPEN J Parenter Enter Nutr 44:516–524
Lee WJ, Liu LK, Peng LN, Lin MH, Chen LK, ILAS Research Group et al (2013) Comparisons of sarcopenia defined by IWGS and EWGSOP criteria among older people: results from the I-Lan longitudinal aging study. J Am Med Dir Assoc 14:528.e1–7
Ishii S, Tanaka T, Shibasaki K et al (2014) Development of a simple screening test for sarcopenia in older adults. Geriatr Gerontol Int 14:93–101
Wu CH, Chen KT, Hou MT et al (2014) Prevalence and associated factors of sarcopenia and severe sarcopenia in older Taiwanese living in rural community: the Tianliao Old People study 04. Geriatr Gerontol Int 14:69–75
Wu Y-H, Hwang A-C, Liu L-K et al (2016) Sex differences of sarcopenia in Asian populations: the implications in diagnosis and management. J Clin Gerontol Geriatr 7:37–43
Kingston A, Wohland P, Wittenberg R et al (2017) Is late-life dependency increasing or not? A comparison of the Cognitive Function and Ageing Studies (CFAS). Lancet 390:1676–1684
Yoshimura Y, Wakabayashi H, Bise T et al (2019) Sarcopenia is associated with worse recovery of physical function and dysphagia and a lower rate of home discharge in Japanese hospitalized adults undergoing convalescent rehabilitation. Nutrition 61:111–118
Janssen I, Shepard DS, Katzmarzyk PT, Roubenoff R et al (2004) The healthcare costs of sarcopenia in the United States. J Am Geriatr Soc 52:80–85
Fırat Ozer F, Akın S, Soysal T, Gokcekuyu BM, Erturk ZG (2021) Relationship between dysphagia and sarcopenia with comprehensive geriatric evaluation. Dysphagia 36:140–146
Cerri AP, Bellelli G, Mazzone A, Pittella F, Landi F, Zambon A, Annoni G (2015) Sarcopenia and malnutrition in acutely ill hospitalized elderly: prevalence and outcomes. Clin Nutr 34:745–751
Jyväkorpi SK, Ramel A, Strandberg TE et al (2021) The sarcopenia and physical frailty in older people: multi-component treatment strategies (SPRINTT) project: description and feasibility of a nutrition intervention in community-dwelling older Europeans. Eur Geriatr Med. https://doi.org/10.1007/s41999-020-00438-4
Martínez-Velilla N, Casas-Herrero A, Zambom-Ferraresi F et al (2019) Effect of exercise intervention on functional decline in very elderly patients during acute hospitalization: a randomized clinical trial. JAMA Intern Med 179:28–36
Kera T, Kawai H, Hirano H et al (2020) Limitations of SARC-F in the diagnosis of sarcopenia in community-dwelling older adults. Arch Gerontol Geriatr 87:103959
Li M, Kong Y, Chen H, Chu A, Song G, Cui Y (2019) Accuracy and prognostic ability of the SARC-F questionnaire and Ishii’s score in the screening of sarcopenia in geriatric inpatients. Braz J Med Biol Res 52:e8204
Yu SC, Khow KS, Jadczak AD, Visvanathan R (2016) Clinical screening tools for sarcopenia and its management. Curr Gerontol Geriatr Res 2016:5978523
Acknowledgements
We would like to thank Prof. FehmiAkcicek (Division of Geriatrics, Department of Internal Medicine, School of Medicine, Ege University, Izmir, Turkey), Prof. TeslimeAtlı (Guven Hospital, Department of Geriatrics, Ankara, Turkey), and Meftun Fırtına (Medical Manager, Nutricia, Turkey) for their support.
Funding
This work was supported by Nutricia Turkey. The funding played no role in study design, collection, analysis, interpretation of data, writing the manuscript, or the decision to submit for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Study protocol was approved by the Ethical Committee of the Faculty of Medicine-Istanbul University. ((Decision no: 02/Date:22.01.2016/No:153).
Informed consent
All participants or their proxies signed the informed consent form.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ozer, F.F., Akin, S., Tasci, İ. et al. Risk of sarcopenia in hospitalized patients and related clinical factors: a multicenter study from Turkey. Eur Geriatr Med 12, 863–870 (2021). https://doi.org/10.1007/s41999-021-00499-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-021-00499-z