Key summary points
To investigate the association between sleep quality and duration and muscle strength among community-dwelling middle-aged and older adults.
AbstractSection FindingsAccording to the present review, it seems that there is an association between sleep quality and duration with handgrip strength among middle-aged and older adults. The results for the gender-specific impact and the different sleep duration (short or long or both) are inconsistent.
AbstractSection MessageHealth professionals should conduct geriatric assessment and consider the possible coexistence of impaired sleep with weak muscle strength, especially in older adults who are at high risk of sarcopenia, frailty or functional limitations.
Abstract
Purpose
To examine the relationship between sleep quality and duration and muscle strength among community-dwelling middle-aged and older adults.
Methods
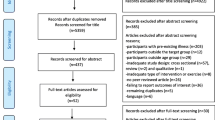
A systematic review was conducted from March 2020 until May 2020. Searches were done for peer-reviewed and English-written articles reporting results of studies in PubMed, Embase, Scopus, Cochrane Library, and in article references lists. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses was used as well as the Newcastle–Ottawa Scale (NOS) to appraise the methodological quality.
Results
Twenty-one cross-sectional, three prospective studies and a total of 92,363 subjects were included. The majority of the included studies are classified as “high quality”. Handgrip strength is the main method of muscle strength assessment. Sleep assessment is usually conducted using subjective measures, such as validated sleep scales or self-reported questionnaires. Actigraphy, as an objective measure, is used less often. Most studies support strong evidence on the association between weak muscle strength and poor sleep quality and duration among middle-aged and older adults; whereas the results for the gender-specific association and the impact of short or long sleep duration were inconclusive.
Conclusion
This review has identified strong evidence on the relationship between sleep quality and duration and muscle strength among middle-aged and older adults. Health professionals should consider this relationship as a component of geriatric assessment in community practice and geriatric settings. Future rigorous research with a combination of subjective and objective measurements is needed to explore whether gender and specific sleep duration are related to muscle strength.

Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Suetta C, Haddock B, Alcazar J, Noerst T, Hansen OM, Ludvig H et al (2019) The Copenhagen Sarcopenia Study: lean mass, strength, power, and physical function in a Danish cohort aged 20–93 years. J Cachexia Sarcopenia Muscle 10:1316–1329. https://doi.org/10.1002/jcsm.12477
Cruz-Jentoft AJ, Bahat G, Bauer JM, Boirie Y, Bruyère O, Cederholm T et al (2019) Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the extended group for EWGSOP2. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 48(1):16–31. https://doi.org/10.1093/ageing/afy169
Beaudart C, McCloskey E, Bruyère O, Cesari M, Rolland Y, Rizzoli R et al (2016) Sarcopenia in daily practice: assessment and management. BMC Geriatrics 16(1):1–10. https://doi.org/10.1186/s12877-016-0349-4
Martien S, Delecluse C, Boen F, Seghers J, Pelssers J, Van Hoecke AS et al (2015) Is knee extension strength a better predictor of functional performance than handgrip strength among older adults in three different settings? Arch Gerontol Geriatr 60(2):252–258. https://doi.org/10.1016/j.archger.2014.11.010
Chen HC, Hsu NW, Chou P ( 2017) The Association between sleep duration and hand grip strength in community-dwelling older adults: the Yilan study, Taiwan. Sleep. 40(4) doi: 10.1093/sleep/zsx021.
Govoni B, Mantovani G, Maietti E, Savino E, Brombo G, Bianchi et al. (2019) Hand grip strength assessment in older people: is the supine position valid and reliable?. Eur Geriatr Med. 10:741–745. Doi: 10.1007/s41999-019-00226-9
Norman K, Stobäus N, Gonzalez MC, Schulzke JD, Pirlich M (2011) Hand grip strength: Outcome predictor and marker of nutritional status. Clin Nutr 30(2):135–142. https://doi.org/10.1016/j.clnu.2010.09.010
Bohannon RW (2019) Grip Strength: an indispensable biomarker for older adults. Clin Interv Aging 14:1681–1691. https://doi.org/10.2147/CIA.S1945438
Halaweh H (2020) Correlation between health-related quality of life and hand grip strength among older adults. Exp Aging Res. https://doi.org/10.1080/0361073X.2020.1716157
Bokshan SL, DePasse JM, Daniels AH (2016) Sarcopenia in orthopedic surgery. Orthopedics 39(2):e295–300. https://doi.org/10.3928/01477447-20160222-0210
Nakazono T, Kamide N, Ando M (2014) The reference values for the chair stand test in healthy Japanese older people: determination by meta-analysis. J Phys Ther Sci 26(11):1729–1731. https://doi.org/10.1589/jpts.26.1729
Malinowska KB, Ikezoe T, Ichihashi N, Arai H, Murase K, Chin K et al (2017) Self-reported quality of sleep is associated with physical strength among community-dwelling young-old adults. Geriatr Gerontol Int 17:1808–1813. https://doi.org/10.1111/ggi.12965
Crowley K (2011) Sleep and sleep disorders in older adults. Neuropsychol Rev 21:41–53. https://doi.org/10.1007/s11065-010-9154-6
Stone KL, Blackwell TL, Ancoli-Israel S, Cauley JA, Redline S, Marshall LM, for the Osteoporotic Fractures in Men (MrOS) Study Group et al (2014) Sleep disturbances and increased risk of falls in older community-dwelling men: the outcomes of sleep disorders in older men (MrOS Sleep) Study. J Am Geriatr Soc 62(2):299–305. https://doi.org/10.1111/jgs.12649
Prato SCF, Andrade SM, Cabrera MAS, Dip RM, Santos HG, Dellaroza MSG et al (2017) Frequency and factors associated with falls in adults aged 55 years or more. Rev Saude Publica 51:37. https://doi.org/10.1590/s1518-8787.2017051005409
Fu L, Yu X, Zhang W, Han P, Kang L, Ma Y et al (2019) The relationship between sleep duration, falls, and muscle mass: a cohort study in an elderly Chinese population. Rejuvenation Res 22(5):390–398. https://doi.org/10.1089/rej.2018.2102
Wai JL, Yu DS (2020) The relationship between sleep-wake disturbances and frailty among older adults: a systematic review. J Adv Nurs 76(1):96–108. https://doi.org/10.1111/jan.14231
Schubert CR, Cruikshanks KJ, Dalton DS, Klein BEK, Klein R, Nondahl DM (2002) Prevalence of sleep problems and quality of life in an older population. Sleep 25:48–52. https://doi.org/10.1093/sleep/25.8.48
Choi EPH, Wan EYF, Kwok JYY, Chin WY, Lam CLK (2019) The mediating role of sleep quality in the association between nocturia and health-related quality of life. Health Qual Life Outcomes 17:181. https://doi.org/10.1186/s12955-019-1251-5
Vaz Fragoso CA, Gill TM (2007) Sleep complaints in community-living older persons: a multifactorial geriatric syndrome. J Am Geriatr Soc 55(11):1853–1866. https://doi.org/10.1111/j.1532-5415.2007.01399.x
Spira AP, Chen-Edinboro LP, Wu MN, Yaffe K (2014) Impact of sleep on the risk of cognitive decline and dementia. Curr Opin Psychiatry 27(6):478–483. https://doi.org/10.1097/YCO.0000000000000106
Wennberg AMV, Wu MN, Rosenberg PB, Spira AP (2017) Sleep disturbance, cognitive decline, and dementia: a review. Semin Neurol 37(4):395–406. https://doi.org/10.1055/s-0037-1604351
Van de Berg JF, van Rooij FJA, Vos H, Tulen JHM, Hofman A, Miedema HME et al (2008) Disagreement between subjective and actigraphic measures of sleep duration in a population-based study of elderly persons. J Sleep Res. 17(3):295–302. https://doi.org/10.1111/j.1365-2869.2008.00638.x
Vallières A, Morin CM (2003) Actigraphy in the assessment of insomnia. Sleep 26(7):902–906. https://doi.org/10.1093/sleep/26.7.902
Rubio-Arias JÁ, Rodríguez-Fernández R, Andreu L, Martínez-Aranda LM, Martínez-Rodriguez A, Ramos-Campo DJ (2019) Effect of sleep quality on the prevalence of sarcopenia in older adults: a systematic review with meta-analysis. J Clin Med 8(12):2156. https://doi.org/10.3390/jcm8122156
Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2009. http://www.ohrica/programs/clinical_epidemiology/oxford htm [cited 2009 Oct19]. Accessed 15 May 2020.
Stang A (2020) Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605. https://doi.org/10.1007/s10654-010-9491-z
Herzog R, Alvarez-Pasquin MJ, Diaz C, Del Barrio JL, Estrada JM, Gil A (2013) Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health 13:154. https://doi.org/10.1186/1471-2458-13-154
Goldman SE, Stone KL, Ancoli-Israel S, Blackwell T, Ewing SK, Boudreau R et al (2007) Poor sleep is associated with poorer physical performance and greater functional limitations in older women. Sleep 30(10):1317–1324. https://doi.org/10.1093/sleep/30.10.1317
Dam TTL, Ewing S, Ancoli-Israel S, Ensrud K, Redline S, Stone K, for the Osteoporotic Fractures in Men Research Group (2008) Association between sleep and physical function in older men: the osteoporotic fractures in men sleep study. J Am Geriatr Soc 56:1665–1673. https://doi.org/10.1111/j.1532-5415.2008.01846.x
Spira AP, Kaufmann CN, Kasper JD, Ohayon MM, Rebok GW, Skidmore E et al (2014) Association between insomnia symptoms and functional status in US older adults. J Gerontol Ser B 69(Suppl 1):S35–S41. https://doi.org/10.1093/geronb/gbu116
Kim M, Yoshida H, Sasai H, Kojima N, Kim H (2015) Association between objectively measured sleep quality and physical function among community-dwelling oldest old Japanese: a cross-sectional study. Geriatrics Gerontol Int 15(1040):1048. https://doi.org/10.1111/ggi.12396
Auyeung TW, Kwok T, Leung J, Lee JSW, Ohlsson C, Vandenput L et al (2015) Sleep duration and disturbances were associated with testosterone level, muscle mass, and muscle strength-A cross-sectional study in 1274 older men. J Am Med Directors Assoc 16(7):630.e1–630.e6. https://doi.org/10.1016/j.jamda.2015.04.006
Vasconcelos K, Dias J, Bastone A, Vieira R, Andrade A, Perracini M et al (2016) Handgrip strength cutoff points to identify mobility limitation in community-dwelling older people and associated factors. J Nutr Health Aging 20:306–315. https://doi.org/10.1007/s12603-015-0584-y
Buchmann N, Spira D, Norman K, Demuth I, Eckardt R, Steinhagen-Thiessen E (2016) Sleep, muscle mass and muscle function in older people—a cross-sectional analysis based on data from the Berlin Aging Study II (BASE-II). Dtsch Arztebl Int 113:523–560. https://doi.org/10.3238/arztebl.2016.0253
Santos-Orlandi AA dos, Ceolim MF, Pavarini SC. Iost, Oliveira-Rossignolo SC de, Pergola-Marconato AM, Neri AL (2016) Factors associated with duration of naps among community-dwelling elderly: data from the multicenter study Fibra. Texto Contexto—Enfermagem 25(1):e1200014. https://doi.org/10.1590/0104-07072016001200014
Moreno-Vecino B, Arija-Blázquez A, Pedrero-Chamizo R, Gómez-Cabello A, Alegre LM, Pérez-López FR et al (2017) on behalf of the EXERNET Group (2017) Sleep disturbance, obesity, physical fitness and quality of life in older women: EXERNET study group. Climacteric 20(1):72–79. https://doi.org/10.1080/13697137.2016.1264934
Fu L, Jia L, Zhang W, Han P, Kang L, Ma Y et al (2017) The association between sleep duration and physical performance in Chinese community-dwelling elderly. PLoS ONE 12(3):e0174832. https://doi.org/10.1371/journal.pone.0174832
Pengpid S, Peltzer K. Hand grip strength and its sociodemographic and health correlates among older adult men and women (50 years and older) in Indonesia. Current Gerontology and Geriatrics Research. 2018 Article ID 3265041; https://doi.org/10.1155/2018/326504
Locquet M, Beaudart C, Delandsheere L, Reginster JY, Bruyère O (2018) Subjective sleep quality among sarcopenic and non-sarcopenic older adults: results from the SarcoPhAge cohort. J Frailty Aging 7(3):176–181. https://doi.org/10.14283/jfa.2018.13
Selvamani Y, Arokiasamy P, Chaudhary M Himanshu (2018) Association of sleep problems and sleep duration with self-rated health and grip strength among older adults in India and China: results from the study on global aging and adult health (SAGE). J Public Health (Berl.) 26:697–707. https://doi.org/10.1007/s10389-018-0906-8
McGregor DE, Carson V, Palarea-Albaladejo J, Dall PM, Tremblay MS, Chastin SFM (2018) Compositional analysis of the associations between 24-h movement behaviours and health indicators among adults and older adults from the canadian health measure survey. Int J Environ Res Public Health 15:1779. https://doi.org/10.3390/ijerph15081779
Xu H, Shi J, Shen C, Liu Y, Liu JM, Zheng XY (2019) Sarcopenia-related features and factors associated with low muscle mass, weak muscle strength, and reduced function in Chinese rural residents: a cross-sectional study. Arch Osteoporos 14:2. https://doi.org/10.1007/s11657-018-0545-2
Peng X, Liu N, Zhang X, Bao X, Xie Y, Huang J et al (2019) Associations between objectively assessed physical fitness levels and sleep quality in community-dwelling elderly people in South China. Sleep Breath 23:679–685. https://doi.org/10.1007/s11325-018-1749-9
Yang CW, Li CI, Li TC, Liu CS, Lin CH, Lin WY et al (2019) Combined effects of having sleep problems and taking sleeping pills on the skeletal muscle mass and performance of community-dwelling elders. Sci Rep 9:13760. https://doi.org/10.1038/s41598-019-50295-w
Aparicio VA, Marín-Jiménez N, Coll-Risco I, de la Flor-Alemany M, Baena-García L, Acosta-Manzano P et al (2019) Doctor, ask your perimenopausal patient about her physical fitness; association of self-reported physical fitness with cardiometabolic and mental health in perimenopausal women. Menopause 26(10):1146–1153. https://doi.org/10.1097/GME.0000000000001384
Lee PF, Ho CC, Yeh DP, Hung CT, Chang YC, Liu CC et al (2020) Cross-sectional associations of physical fitness performance level and sleep duration among older adults: results from the national physical fitness survey in Taiwan. Int J Environ Res Public Health 17:388. https://doi.org/10.3390/ijerph17020388
Spira AP, Covinsky K, Rebok GW, Punjabi NM, Stone KL, Hillier TA et al (2012) Poor sleep quality and functional decline in older women. J Am Geriatr Soc 60:1092–1098. https://doi.org/10.1111/j.1532-5415.2012.03968.x
Wang TY, Wu Y, Wang T, Li Y, Zhang D (2018) A prospective study on the association of sleep duration with grip strength among middle-aged and older Chinese. Exp Gerontol 103:88–93. https://doi.org/10.1016/j.exger.2018.01.009
Hughes JM, Song Y, Fung CH, Dzierzewsk JM, Mitchell MN, Jouldjian S et al (2018) Measuring sleep in vulnerable older adults: a comparison of subjective and objective sleep measures. Clin Gerontol 41(2):145–157. https://doi.org/10.1080/07317115.2017.1408734
Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP (2003) The role of actigraphy in the study of sleep and circadian rhythms. Sleep 26(3):342–392. https://doi.org/10.1093/sleep/26.3.342
Piovezan RD, Abucham J, dos Santos RVT, Mello MT, Tufik S, Poyares D (2015) The impact of sleep on age-related sarcopenia: possible connections and clinical implications. Ageing Research Reviews 23:210–220. https://doi.org/10.1016/j.arr.2015.07.003
Dattilo M, Antunes HKM, Medeiros A, Mônico Neto M, Souza HS, Tufik S et al (2011) Sleep and muscle recovery: endocrinological and molecular basis for a new and promising hypothesis. Med Hypotheses 77(2):220–222. https://doi.org/10.1016/j.mehy.2011.04.017
Irwin MR, Wang M, Ribeiro D, Cho HJ, Olmstead R, Crabb Breen E et al (2008) Sleep loss activates cellular inflammatory signaling. Biol Psychiat 64(6):538–540. https://doi.org/10.1016/j.biopsych.2008.05.004
Chatterjee S, Ma K (2016) Circadian clock regulation of skeletal muscle growth and repair [version 1; peer review: 3 approved]. F1000 Research. 5:1549. https://doi.org/10.12688/f1000research.9076.1
Merellano-Navarro E, Collado-Mateo D, García-Rubio J, Gusi N, Olivares PR (2017) Validity of the International Fitness Scale “IFIS” in older adults. Exp Gerontol 95:77–81. https://doi.org/10.1016/j.exger.2017.05.001
Funding
None declared.
Author information
Authors and Affiliations
Contributions
AP conceived the idea for the study. AP and VSV performed the literature search and the data analysis. The manuscript was drafted by AP and VSV. All authors finalized, provided critical review, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no conflict of interest.
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent to participate
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pana, A., Sourtzi, P., Kalokairinou, A. et al. Association between muscle strength and sleep quality and duration among middle-aged and older adults: a systematic review. Eur Geriatr Med 12, 27–44 (2021). https://doi.org/10.1007/s41999-020-00399-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-020-00399-8