Key summary points
We assessed agreement, accuracy, precision, and reliability of retrospectively compared with prospectively and separately attained, retrospective Clinical Frailty Scale (CFS) scoring, respectively.
AbstractSection FindingsCompared to both prospectively and separately retrospectively attained CFS, retrospective CFS scores demonstrated high agreement, accuracy, precision, and reliability in 110 hospitalized patients aged ≥ 80 years.
AbstractSection MessageThe retrospectively attained CFS score is a valid diagnostic instrument to measure frailty in older hospitalized patients.
Abstract
Purpose
There is a considerable need to measure frailty retrospectively in clinical practice and research. We assessed agreement, accuracy, precision, and reliability of retrospectively compared with prospectively, and separately attained, retrospective Clinical Frailty Scale (CFS) scoring, respectively.
Methods
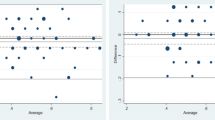
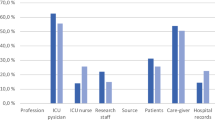
We studied 110 hospitalized patients aged ≥ 80 years, consisting of 70.9% females. Agreement was assessed by bias, accuracy by root mean square error (RMSE) and the percentages of one CFS scores within 20% and 30% of each other (P20 and P30), precision by interquartile ranges of the bias, and reliability by weighted Cohen’s kappa (κ).
Results
Comparison of retrospective and prospective CFS scores demonstrated a modest bias of 0.26. Classification as robust, prefrail, or frail was generally correct in retrospectively compared to prospectively CFS scores. RMSE was low (0.28), while P20 and P30 values were high (90.0% and 96.6%, respectively). Precision of retrospective to predict prospective CFS scores was high with narrow interquartile ranges of 0 and 1. Reliability of retrospective with prospective CFS scores was high (κ = 0.89). Comparing two separately attained retrospective CFS scores demonstrated low bias (0.05) and RMSE (0.24), and a high P30 value (90.0%). Precision and interrater reliability of the comparison of retrospective CFS scores were high with narrow interquartile ranges and κ = 0.85.
Conclusion
The retrospectively attained CFS score is a valid diagnostic instrument to measure frailty in older hospitalized patients with high agreement, accuracy, precision, and reliability compared to both prospective and separately attained CFS scores.



Similar content being viewed by others
Code availability
Not applicable.
References
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K (2013) Frailty in elderly people. Lancet 381:752–762
Sieber CC (2017) Frailty—from concept to clinical practice. Exp Gerontol 87:160–167
Rockwood K, Song X, MacKnight C et al (2005) A global clinical measure of fitness and frailty in elderly people. CMAJ 173:489–495
Basic D, Shanley C (2015) Frailty in an older inpatient population: using the clinical frailty scale to predict patient outcomes. J Aging Health 27:670–685
Wallis SJ, Wall J, Biram RW, Romero-Ortuno R (2015) Association of the clinical frailty scale with hospital outcomes. QJM 108:943–949
Dent E, Kowal P, Hoogendijk EO (2016) Frailty measurement in research and clinical practice: a review. Eur J Intern Med 31:3–10
Hatcher VH, Galet C, Lilienthal M, Skeete DA, Romanowski KS (2019) Association of clinical frailty scores with hospital readmission for falls after index admission for trauma-related injury. JAMA Netw Open 2:e1912409
Cheung A, Haas B, Ringer TJ, McFarlan A, Wong CL (2017) Canadian study of health and aging clinical frailty scale: does it predict adverse outcomes among geriatric trauma patients? J Am Coll Surg 225:658–665
Ekerstad N, Swahn E, Janzon M et al (2011) Frailty is independently associated with short-term outcomes for elderly patients with non-ST-segment elevation myocardial infarction. Circulation 124:2397–2404
Kahlon S, Pederson J, Majumdar SR et al (2015) Association between frailty and 30-day outcomes after discharge from hospital. CMAJ 187:799–804
Fernando SM, McIsaac DI, Rochwerg B et al (2019) Frailty and invasive mechanical ventilation: association with outcomes, extubation failure, and tracheostomy. Intensive Care Med 45:1742–1752
Darvall JN, Bellomo R, Paul E et al (2019) Frailty in very old critically ill patients in Australia and New Zealand: a population-based cohort study. Med J Aust 211:318–323
Wharton C, King E, MacDuff A (2019) Frailty is associated with adverse outcome from in-hospital cardiopulmonary resuscitation. Resuscitation 143:208–211
Ward J, Phillips G, Radotra I et al (2018) Frailty: an independent predictor of burns mortality following in-patient admission. Burns 44:1895–1902
Kimber DE, Kehler DS, Lytwyn J et al (2018) Pre-operative frailty status is associated with cardiac rehabilitation completion: a retrospective cohort study. J Clin Med 7:E560
Lyons A, Romero-Ortuno R, Hartley P (2019) Functional mobility trajectories of hospitalized older adults admitted to acute geriatric wards: a retrospective observational study in an English university hospital. Geriatr Gerontol Int 19:305–310
Davies J, Whitlock J, Gutmanis I, Kane SL (2018) Inter-rater reliability of the retrospectively assigned clinical frailty scale score in a geriatric outreach population. Can Geriatr J 21:1–5
Shears M, Takaoka A, Rochwerg B et al (2018) Assessing frailty in the intensive care unit: a reliability and validity study. J Crit Care 45:197–203
Darvall JN, Boonstra T, Norman J et al (2019) Retrospective frailty determination in critical illness from a review of the intensive care unit clinical record. Anaesth Intensive Care 47:343–348
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW (1963) Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA 185:914–919
Bossuyt PM, Reitsma JB, Bruns DE et al (2015) STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ 2015(351):h5527
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1(8476):307–310
Moreno-Arino M, Torrente Jiménez I, Cartanyà Gutiérrez A, Comet R (2020) Assessing the strengths and weaknesses of the Clinical Frailty Scale through correlation with a frailty index. Aging Clin Exp Res. https://doi.org/10.1007/s40520-019-01450-w
Acknowledgements
The study was funded by the Dr. Werner Jackstädt Foundation.
Funding
The study was funded by the Dr. Werner Jackstädt Foundation. The funding source was informed about the design and conduct and regularly updated on the status of the study but had no role in the analysis, writing, or submission of this report.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Data collection was performed by all the authors, data analysis by KS and SH-R. The first draft of the manuscript was written by SH-R and further versions were revised by all the authors. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures performed in these studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments. The study protocol was approved by the local ethics committee (Medical council Bremen, reference number RA/RE-578).
Consent to participate
The requirement of obtaining informed consent to participate was waived by the local ethics committee as assessment of frailty with the CFS contains information which are routinely gathered on admission in our institution.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stille, K., Temmel, N., Hepp, J. et al. Validation of the Clinical Frailty Scale for retrospective use in acute care. Eur Geriatr Med 11, 1009–1015 (2020). https://doi.org/10.1007/s41999-020-00370-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-020-00370-7