Key summary points
To perform a narrative review aiming at evaluating the applicability and feasibility of occupational therapy in people with delirium.
AbstractSection FindingsIn this article, the current evidence of the role of occupational therapy for the prevention and management of people with delirium across different settings of care (intensive care units, rehabilitation facilities, and nursing homes) is described. Overall, the article summarizes the results of various studies, supporting the feasibility and efficacy of non-pharmacological approaches conducted by occupational therapists.
AbstractSection MessageThough further studies are required to confirm initial evidence, there is reason to believe that occupational therapy may be an effective approach to help the management of delirious people across various settings of care. Occupational therapy may therefore be included in the early stages of rehabilitation management for people with delirium.
Abstract
Purpose
To perform a narrative review of studies on the applicability and feasibility of occupational therapy in persons with delirium by analyzing evaluation and procedural methods in the therapeutic settings.
Methods
Starting from the international classification of disability, the focus was to understand if and how occupational therapy as a multi-component intervention can reduce the duration and intensity of delirium to prevent future disabilities. This review also includes scientific studies demonstrating the benefits of occupational therapy in terms of increased functional and occupational outcomes. Finally, the evaluation modalities and the therapeutic procedures performed by the occupational therapist have been analyzed.
Results
The non-pharmacological treatments occupational therapists perform in people with delirium in intensive care settings are supported by scientific evidence.
Conclusions
There is preliminary evidence of the benefit of including occupational therapy in early stages of rehabilitation in acute care to prevent and treat delirium. Nevertheless, further studies are necessary to define the different aspects of the multidisciplinary approach that is common in geriatric practice, primarily determining the adequate timing, and intensity of interventions as well as its appropriate settings.



Similar content being viewed by others
References
Martinez F, Tobar C, Hill N (2015) Preventing delirium: should non-pharmacological, multicomponent interventions be used? A systematic review and meta-analysis of the literature. Age Ageing 44(2):196–204
Siddiqi N, Harrison JK, Clegg A et al (2016) Interventions for preventing delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev 3:CD005563
Occupational Therapy Europe What is OT?—OT EU. https://www.oteurope.eu/what-is-ot. Accessed 31 July 2019
Kielhofner G (2008) Model of human occupation : theory and application, 3rd edn. Lippincott Williams & Wilkins, Philadelphia
Gitlin LN, Winter L, Dennis MP et al (2010) A biobehavioral home-based intervention and the well-being of patients with dementia and their caregivers. JAMA 304(9):983
World Health Organization ICF Browser. https://apps.who.int/classifications/icfbrowser/Default.aspx. Accessed 10 June 2019
WHO (2018) International classification of functioning, disability and health (ICF). WHO
Somerville E, Smallfield S, Stark S et al (2016) Occupational therapy home modification assessment and intervention. Am J Occup Ther. https://doi.org/10.5014/ajot.2016.705002
National Institute for Health and Care Excellence; Delirium: prevention, diagnosis and management | Guidance | NICE In https://www.nice.org.uk/guidance/cg103. Accessed 12 June 2019
Rains J, Chee N (2017) The role of occupational and physiotherapy in multi-modal approach to tackling delirium in the intensive care. J Intensive Care Soc 18(4):318–322
Inouye SK, Bogardus ST, Charpentier PA et al (1999) A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med 340(9):669–676
Hshieh TT, Yue J, Oh E et al (2015) Effectiveness of multicomponent nonpharmacological delirium interventions. JAMA Intern Med. https://doi.org/10.1001/jamainternmed.2014.7779
Martinez FT, Tobar C, Beddings CI et al (2012) Preventing delirium in an acute hospital using a non-pharmacological intervention. Age Ageing. 41(5):629–634
Marcantonio ER, Flacker JM, Wright RJ et al (2001) Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc 49(5):516–522
Toye C, Kitchen S, Hill A et al (2017) Piloting staff education in Australia to reduce falls in older hospital patients experiencing delirium. Nurs Health Sci 19(1):51–58
Piersol CV, Jensen L, Lieberman D et al (2017) Occupational therapy interventions for people with Alzheimer’s disease. Am J Occup Ther 72(1):72–81
Zaal IJ, Slooter AJC (2012) Delirium in critically ill patients. Drugs 72(11):1457–1471
Van Rompaey B, Elseviers M, Van Drom W et al (2012) The effect of earplugs during the night on the onset of delirium and sleep perception: a randomized controlled trial in intensive care patients. Crit Care. https://doi.org/10.1186/cc11330
Collinsworth AW, Priest EL, Campbell CR et al (2016) A review of multifaceted care approaches for the prevention and mitigation of delirium in intensive care units. J Intensive Care Med. 31(2):127–141
Sáez de Asteasu ML, Martínez-Velilla N, Zambom-Ferraresi F et al (2019) Assessing the impact of physical exercise on cognitive function in older medical patients during acute hospitalization: secondary analysis of a randomized trial. PLoS Med. https://doi.org/10.1371/journal.pmed.1002852
Resnick B, Beaupre L, McGilton KS et al (2016) Rehabilitation interventions for older individuals with cognitive impairment post-hip fracture: a systematic review. J Am Med Dir Assoc 17(3):200–205
Rogers AT, Bai G, Lavin RA et al (2017) Higher hospital spending on occupational therapy is associated with lower readmission rates. Med Care Res Rev. https://doi.org/10.1177/1077558716666981
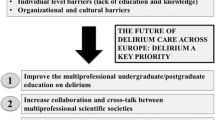
Morandi A, Pozzi C, Milisen K et al (2019) An interdisciplinary statement of scientific societies for the advancement of delirium care across Europe (EDA, EANS, EUGMS, COTEC, IPTOP/WCPT). BMC Geriatr 19(1):253
Tobar E, Alvarez E, Garrido M (2017) Cognitive stimulation and occupational therapy for delirium prevention. Rev Bras Ter Intensiva 29(2):248–252
Álvarez EA, Garrido MA, Tobar EA et al (2017) Occupational therapy for delirium management in elderly patients without mechanical ventilation in an intensive care unit: a pilot randomized clinical trial. J Crit Care 37:85–90
Schweickert WD, Pohlman MC, Pohlman AS et al (2009) Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 373(9678):1874–1882
Pozzi C, Lucchi E, Lanzoni A et al (2017) Preliminary evidence of a positive effect of occupational therapy in patients with delirium superimposed on dementia. J Am Med Dir Assoc 18(12):1091–1092
Pozzi C, Lanzoni A, Lucchi E et al (2019) Activity-based occupational therapy intervention for delirium superimposed on dementia in nursing home setting: a feasibility study. Aging Clin Exp Res. https://doi.org/10.1007/s40520-019-01422-0
Parkinson S, Chester A, Cratchley S et al (2008) Application of the model of human occupation screening tool (MOHOST assessment) in an acute psychiatric setting. Occup Ther Health Care 22(2–3):63–75
Bellelli G, Morandi A, Davis DHJ et al (2014) Validation of the 4AT, a new instrument for rapid delirium screening: a study in 234 hospitalised older people. Age Ageing 43(4):496–502
Morandi A, Han JH, Meagher D et al (2016) Detecting delirium superimposed on dementia: evaluation of the diagnostic performance of the Richmond agitation and sedation scale. J Am Med Dir Assoc 17(9):828–833
Marcantonio ER, Ngo LH, O’Connor M et al (2014) 3D-CAM: derivation and validation of a 3-minute diagnostic interview for CAM-defined delirium: a cross-sectional diagnostic test study. Ann Intern Med 161(8):554–561
Ward G, Jagger C, Harper W (1996) The Canadian occupational performance measure: what do users consider important? Br J Ther Rehabil 3(8):448–452
Brown WC (2011) Book review: the pool activity level (PAL) instrument for occupational profiling: a practical resource for carers of people with cognitive impairment, 3rd edition, by Jackie Pool. London: Jessica Kingsley Publishers, 173 pp. ISBN: 978-1-84310-594-7. Dementia 10(2):272–273
Fisher AG (2009) Occupational therapy intervention process model : a model for planning and implementing top-down, client-centered, and occupation-based interventions. Three Star Press Inc, Fort Collins
De las Heras CG (1998) A User’s Manual for the Volitional Questionnaire—Carmen Gloria de las Heras—Google Libros. University of Illinois at Chicago, Chicago
Strong S, Rigby P, Stewart D et al (1999) Application of the person–environment–occupation model: a practical tool. Can J Occup Ther 66(3):122–133
British Geriatrics Society. SIGN 157: Risk reduction and management of delirium. 2019. https://www.bgs.org.uk/resources/sign-157-risk-reduction-and-management-of-delirium. Accessed 29 Aug 2019
Young Y, Fan M-Y, Hebel JR et al (2009) Concurrent validity of administering the functional independence measure (FIM) instrument by interview. Am J Phys Med Rehabil 88(9):766–770
MacDermid J, Solomon G, Valdes K (2015) Clinical assessment recommendations. American Society of Hand Therapists, Mount Laurel
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
All procedures performed in the study were in accordance with the ethical standards of the 1964 Helsinki declaration.
Informed consent
Informed consent was obtained from patients’ authorized surrogates at study enrollment.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to special issue Delirium, Vol 11, Issue 1, February 2020, https://link.springer.com/journal/41999/11/1.
Rights and permissions
About this article
Cite this article
Pozzi, C., Tatzer, V.C., Álvarez, E.A. et al. The applicability and feasibility of occupational therapy in delirium care. Eur Geriatr Med 11, 209–216 (2020). https://doi.org/10.1007/s41999-020-00308-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-020-00308-z