Abstract
Purpose
Large-scale nationwide comparative studies of older adults with cognitive impairment (CI) in long-term care institutions (LTCI) hardly exist in Poland. This paper compares the prevalence of CI and its symptoms in residents of nursing homes (NHs) and residential homes (RHs) in Poland.
Methods
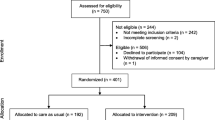
A cross-sectional survey of a country-representative sample of 23 LTCIs was conducted in the years 2015–2016. In total, 1587 residents were included: 626 residents in 11 NHs and 961 residents in 12 RHs. All individuals were assessed with a Cognitive Performance Scale (CPS) using a cutoff of ≥ 2 points to define the presence of CI. Descriptive statistics and Chi square test were used.
Results
The median age was 80 years, 67.7% were women. Overall, 65.2% of residents (n = 1035) were identified as having CI, ranging from 59.2% in RHs to 74.5% in NHs, after excluding residents in a coma. Furthermore, the prevalence of severe CI was significantly higher in NHs than in RHs (respectively, 41.2 and 20.5%). It concerned specifically impairment of memory: procedural (72.3 vs 55.2%), long-term (56.5 vs 32.1%), short-term (46.8 vs 33.4%), and situational one (40.2 vs 26.4%), as well as problems with being understood by others (44.6 vs 24.7%) and severely impaired capacity of daily decision making (44.7 vs 21.5%).
Conclusions
A high prevalence of CI was found in both LTCI types, but its severity differed, with statistically significantly higher rates in NHs compared to RHs. Therefore, we call for more attention to be paid to better recognition of CI in LTCI residents, regardless of the facility type.


Similar content being viewed by others
Abbreviations
- ADL:
-
Activities of daily living
- BI:
-
Barthel Index
- CI:
-
Cognitive impairment
- CPS:
-
Cognitive Performance Scale
- EAPC:
-
European Association of Palliative Care
- LTC:
-
Long-term care
- LTCI:
-
Long-term care institution
- MMSE:
-
Mini-Mental State Examination
- NH:
-
Nursing home
- OECD:
-
Organisation for Economic Co-operation and Development
- RH:
-
Residential home
References
OECD (2017) Health at a glance 2017: OECD Indicators. OECD Publ 2017. https://doi.org/10.1787/health_glance-2013-en
OECD (2013) Health at a glance 2013: OECD Indicators. Paris: 2013. https://doi.org/10.1787/health_glance-2013-en
Główny Urząd Statystyczny (2016) Pomoc społeczna i opieka nad dzieckiem i rodziną w 2015 roku (eng. Social assistance, child and family services in 2015). Warszawa: 2016
Główny Urząd Statystyczny (2017) Zdrowie i ochrona zdrowia w 2016 roku (eng. Health and health care in 2016). Warszawa: 2017
Wagster MV, King JW, Resnick SM, Rapp PR (2012) The 87%: guest editorial. J Gerontol A Biol Sci Med Sci 67:739–740. https://doi.org/10.1093/gerona/gls140
Wang S-Y, Shamliyan TA, Talley KMC, Ramakrishnan R, Kane RL (2013) Not just specific diseases: systematic review of the association of geriatric syndromes with hospitalization or nursing home admission. Arch Gerontol Geriatr 57:16–26. https://doi.org/10.1016/j.archger.2013.03.007
Banaszak-Holl J, Fendrick AM, Foster NL, Herzog AR, Kabeto MU, Kent DM et al (2004) Predicting nursing home admission: estimates from a 7-year follow-up of a nationally representative sample of older Americans. Alzheimer Dis Assoc Disord 18:83–89
Mansbach WE, Mace RA, Clark KM, Firth IM (2017) A comparison of cognitive functioning in long-term care and short-stay nursing home residents. Ageing Soc 37:1–13. https://doi.org/10.1017/S0144686X15000926
Björk S, Juthberg C, Lindkvist M, Wimo A, Sandman PO, Winblad B et al (2016) Exploring the prevalence and variance of cognitive impairment, pain, neuropsychiatric symptoms and ADL dependency among persons living in nursing homes. A cross-sectional study. BMC Geriatr 16:154. https://doi.org/10.1186/s12877-016-0328-9
Stange I, Poeschl K, Stehle P, Sieber CC, Volkert D (2013) Screening for malnutrition in nursing home residents: comparison of different risk markers and their association to functional impairment. J Nutr Health Aging 17:357–363. https://doi.org/10.1007/s12603-013-0021-z
Selbæk G, Kirkevold Ø, Engedal K (2007) The prevalence of psychiatric symptoms and behavioural disturbances and the use of psychotropic drugs in Norwegian nursing homes. Int J Geriatr Psychiatry 22:843–849. https://doi.org/10.1002/gps.1749
Onder G, Carpenter I, Finne-Soveri H, Gindin J, Frijters D, Henrard JC et al (2012) Assessment of nursing home residents in Europe: the Services and Health for Elderly in Long TERm care (SHELTER) study. BMC Health Serv Res 12:5. https://doi.org/10.1186/1472-6963-12-5
Cahill S, Diaz-Ponce AM, Coen RF, Walsh C (2010) The underdetection of cognitive impairment in nursing homes in the Dublin area. The need for on-going cognitive assessment. Age Ageing 39:128–131. https://doi.org/10.1093/ageing/afp198
Kinley J, Hockley J, Stone L, Dewey M, Hansford P, Stewart R et al (2014) The provision of care for residents dying in UK nursing care homes. Age Ageing 43:375–379. https://doi.org/10.1093/ageing/aft158
Hockley J, Watson J, Oxenham D, Murray SA (2010) The integrated implementation of two end-of-life care tools in nursing care homes in the UK: an in-depth evaluation. Palliat Med 24:828–838. https://doi.org/10.1177/0269216310373162
Helvik A-S, Engedal K, Benth JŠ, Selbæk G (2015) Prevalence and severity of dementia in nursing home residents. Dement Geriatr Cogn Disord 40:166–177. https://doi.org/10.1159/000433525
OECD/European Commission (2013) A good life in old age? Monitoring and improving quality in long-term care. http://dx.doi.org/10.1787/9789264194564-enIS
Bońkowski K, Klich-Rączka A (2007) Ciężka niesprawność czynnościowa osób starszych wyzwaniem dla opieki długoterminowej severe functional impairment in the elderly as a challenge at long-term care. Gerontol Pol 15:97–103
Pytka D, Doboszyńska A, Syryło A (2012) Ocena stanu psychofizycznego pacjentów Zakładu Opiekuńczo—Leczniczego “Caritas” Archidiecezji Warszawskiej (eng. Evaluation of psychophysical condition of patients attending the “Caritas” Health Care Centre of the Roman Catholic Archdiocese of Warsaw). Zdr Publ 122:155–159
Wdowiak L, Stanisławek D, Stanisławek A (2009) Jakość życia w stacjonarnej opiece długoterminowej. Med Rodz 12:49–63
Wróblewska I, Iwaneczko A (2012) Jakość życia pensjonariuszy Domu Pomocy Społecznej ‘Złota Jesień’ w Raciborzu—Badania własne. Fam Med Prim Care Rev 14:573–576
Jóźwiak A, Guzik P, Wysocki H (2004) Niski wynik testu Mini Mental State Examination jako czynnik ryzyka zgonu wewnątrzszpitalnego u starszych chorych z niewydolnością serca. Psychogeriatria Pol 1:85–94
Górska-Ciebiada M, Saryusz-Wolska M, Ciebiada M, Loba J (2015) Łagodne zaburzenia funkcji poznawczych u chorych na cukrzycę typu 2 w wieku podeszłym (eng. Mild cognitive impairment in elderly patients with type 2 diabetes). Geriatria 9:102–108
Pawlak A (2015) Jakość świadczonej opieki w ośrodkach całodobowego pobytu dla osób w wieku podeszłym. Fam Med Prim Care Rev 17:197–201
Kowalska J, Szczepańska-Gieracha J, Piątek J (2010) Zaburzenia poznawcze i emocjonalne a długość pobytu osób starszych w Zakładzie Opiekuńczo-Leczniczym o Profilu Rehabilitacyjnym. Psychogeriatria Pol 7:61–70
Kowalska J, Rymaszewska J, Szczepańska-Gieracha J (2013) Occurrence of cognitive impairment and depressive symptoms among the elderly in a nursing home facility. Adv Clin Exp Med 22:111–117
Kuźmicz I, Brzostek T, Górkiewicz M (2014) Występowanie odleżyn a sprawność psychoruchowa osób z zaburzeniami funkcji poznawczych, objętych stacjonarną opieką długoterminową. Probl Pielęgniarstwa 22:307–311
Reitinger E, Froggatt K, Brazil K, Heimerl K, Hockley J, Kunz R, Parker D, Husebo BS (2013) Palliative care in long-term care settings for older people: findings from an EAPC taskforce. Eur J Palliative Care 20(5):251–253
Morris JN, Fries BE, Mehr DR, Hawes C, Phillips C, Mor V et al (1994) MDS Cognitive Performance Scale. J Gerontol 49:M174–M182
Frederiksen K, Tariot P, De Jonghe E (1996) Minimum data set plus (MDS +) scores compared with scores from five rating scales. J Am Geriatr Soc 44:305–309. https://doi.org/10.1111/j.1532-5415.1996.tb00920.x
Snowden M, McCormick W, Russo J, Srebnik D, Comtois K, Bowen J et al (1999) Validity and responsiveness of the minimum data set. J Am Geriatr Soc 47:1000–1004
Jones K, Perlman CM, Hirdes JP, Scott T (2010) Screening cognitive performance with the resident assessment instrument for mental health Cognitive Performance Scale. Can J Psychiatry 55:736–740. https://doi.org/10.1177/070674371005501108
Hartmaier SL, Sloane PD, Guess HA, Koch GG, Mitchell CM, Phillips CD (1995) Validation of the minimum data set Cognitive Performance Scale: agreement with the Mini-Mental State Examination. J Gerontol A Biol Sci Med Sci 50:M128–M133
Paquay L, De Lepeleire J, Schoenmakers B, Ylieff M, Fontaine O, Buntinx F (2007) Comparison of the diagnostic accuracy of the Cognitive Performance Scale (minimum data set) and the mini-mental state exam for the detection of cognitive impairment in nursing home residents. Int J Geriatr Psychiatry 22:286–293. https://doi.org/10.1002/gps.1671
Bula CJ, Wietlisbach V (2009) Use of the cognitive performance scale (CPS) to detect cognitive impairment in the acute care setting: concurrent and predictive validity. Brain Res Bull 80:173–178. https://doi.org/10.1016/j.brainresbull.2009.05.023
Landi F, Tua E, Onder G, Carrara B, Sgadari A, Rinaldi C et al (2000) Minimum data set for home care: a valid instrument to assess frail older people living in the community. Med Care 38:1184–1190
Morris JN, Belleville-Taylor P, Fries BE, Hawes C, Murphy K, Mor V et al (2009) InterRAI long-term care facilities (LTCF) assessment form and user’s manual. Version 9.1. interRAI, Washington, DC
Jorm AF, Jolley D (1998) The incidence of dementia: a meta-analysis. Neurology 51:728–733
Unverzagt FW, Gao S, Baiyewu O, Ogunniyi AO, Gureje O, Perkins A et al (2001) Prevalence of cognitive impairment: data from the Indianapolis study of health and aging. Neurology 57:1655–1662
Rosenthal T (2009) Przewlekłe zaburzenia pamięci. In: Rosenthal TC, Williams MENB (eds) Geriatria. Wyd Czelej, Lublin, pp 291–313
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CRJ, Kawas CH et al (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7:263–269. https://doi.org/10.1016/j.jalz.2011.03.005
Gutierrez Rodriguez J, Jimenez Muela F, Alonso Collada A, de Santa Maria Benedet LS (2009) Prevalence and therapeutic management of dementia in nursing homes in Asturias (Spain). Rev Esp Geriatr Gerontol 44:31–33. https://doi.org/10.1016/j.regg.2008.10.002
Bergh S, Holmen J, Saltvedt I, Tambs K, Selbaek G (2012) Dementia and neuropsychiatric symptoms in nursing-home patients in Nord-Trondelag County. Tidsskr Nor Laegeforen 132:1956–1959. https://doi.org/10.4045/tidsskr.12.0194
Najwyższa Izba Kontroli (2010) Informacja o wynikach kontroli funkcjonowania zakładów opiekuńczoleczniczych (eng. Report on the results of the control of the functioning of long-term care institutions in Poland). Number KPZ-410-09/2009, p 63–66. Warszawa
Acknowledgments
The authors would like to thank the managers of long-term care institutions in Poland who allowed the study to be conducted in their settings and to the facilities’ nursing staff for participating in collecting the data.
Funding
This work was supported by the Jagiellonian University Medical College (Grant No. K/DSC/003080). Grant recipient: Violetta Kijowska, MPH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
The authors declare that the study has been registered and accepted by the Jagiellonian University Ethics Committee (Agreement No. 122.6120.31.2015) and it was conducted in line of the current laws, meeting the standard requirements.
Informed consent
Based on the Jagiellonian University Ethics Committee approval, informed consent was obtained from all settings where the study was conducted. Data collected in the study were analyzed anonymously by researchers without any possibility of identification of individual residents.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kijowska, V., Szczerbińska, K. Prevalence of cognitive impairment among long-term care residents: a comparison between nursing homes and residential homes in Poland. Eur Geriatr Med 9, 467–476 (2018). https://doi.org/10.1007/s41999-018-0062-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-018-0062-2