Abstract
Background
Poor sleep quality in older adults can lead to poorer quality of life.
Purpose
To identify the predominant factors that best predict sleep quality amongst older adults.
Methods
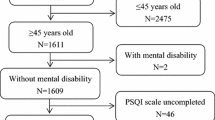
A prospective cross-sectional study was carried out among 310 older adults (≥ 60 years) in the Department of General Medicine of a tertiary care hospital for a duration of 6 months. The Pittsburgh Sleep Quality Index (PSQI) questionnaire and a validated data collection form were used to gather the data and assessed using Statistical Package for Social Sciences (SPSS) version 20.
Results
Out of 310 older adults, 71.3% belonged to the age group 60–69 years, of which 59.0% were males. The prevalence of poor sleep quality (Global Pittsburgh Sleep Quality Index, GPSQI > 5) was 36.8%. There was a significant association between poor sleep quality and factors such as a history of the treatment of medical illness (P = 0.003), present living status such as living with a spouse (P = 0.008) and living alone (P = 0.047), age groups 60–69 (P = 0.019) and 70–79 years (P = 0.028), medical conditions such as hyperlipidemia (P = 0.025), help needed for Activities of daily living (ADL) (P = 0.028), and environmental factors such as noise and light (P = 0.039).
Conclusion
A considerable percentage of older adults in our demographic experience poor sleep. Hence, it is necessary to increase awareness among the public and healthcare providers, encourage healthcare providers to screen for sleep quality and provide education on sleep hygiene and interventions to help resolve problems with sleep.
Similar content being viewed by others
Availability of Data and Material
All data generated or analysed during this study are included in this published article and its supplementary information files.
References
Yaremchuk K. Sleep disorders in the elderly. Clin Geriatr Med. 2018;34(2):205–16. https://doi.org/10.1016/j.cger.2018.01.008.
United Nations Department of Economics and Social Affairs: Population Division. World population ageing: 1950–2050. Accessed 13 Oct 2022
Sharma K, Srivastava S. The effectiveness of sleep hygiene program on sleep quality and stress level in elderly population. J Ment Health Aging. 2018;2(1):29–32. https://doi.org/10.35841/mental-health-aging.2.1.29-32.
Nelson KL, Davis JE, Corbett CF. Sleep quality: an evolutionary concept analysis. Nurs Forum. 2022;57(1):144–51. https://doi.org/10.1111/nuf.12659.
Aliabadi S, Moodi M, Miri MR, Tahergorabi Z, Mohammadi R. Sleep quality and its contributing factors among elderly people: a descriptive-analytical study. Mod Care J. 2017;14(1): e64493. https://doi.org/10.5812/modernc.64493.
Wheaton AG, Shults RA, Chapman DP, Ford ES, Croft JB, Division of Population Health, National Center for Chronic Disease Prevention and Health Promotion. Drowsy driving and risk behaviors -10 States and Puerto Rico, 2011–2012. MMWR Morb Mortal Wkly Rep. 2014;63(26):557–62.
Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, et al. The National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40–3. https://doi.org/10.1016/j.sleh.2014.12.010.
Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843–4. https://doi.org/10.5664/jcsm.4758.
Thichumpa W, Howteerakul N, Suwannapong N, Tantrakul V. Sleep quality and associated factors among the elderly living in rural Chiang Rai, northern Thailand. Epidemiol Health. 2018;40:e2018018. https://doi.org/10.4178/epih.e2018018.
Wang P, Song L, Wang K, Han X, Cong L, Wang Y, et al. Prevalence and associated factors of poor sleep quality among Chinese older adults living in a rural area: a population-based study. Aging Clin Exp Res. 2020;32(1):125–31. https://doi.org/10.1007/s40520-019-01171-0.
Zdanys KF, Steffens DC. Sleep disturbances in the elderly. Psychiatr Clin North Am. 2015;38(4):723–41. https://doi.org/10.1016/j.psc.2015.07.010.
Gulia KK, Kumar VM. Sleep disorders in the elderly: a growing challenge. Psychogeriatrics. 2018;18(3):155–65. https://doi.org/10.1111/psyg.12319. (PMID: 29878472).
Mc Carthy CE. Sleep disturbance, sleep disorders and co-morbidities in the care of the older person. Med Sci. 2021;9(2):31. https://doi.org/10.3390/medsci9020031.
Jaqua EE, Hanna M, Labib W, Moore C, Matossian V. Common sleep disorders affecting older adults. Perm J. 2022;27(1):122–32. https://doi.org/10.7812/TPP/22.114.
Das S, Roy RN, Das DK, Chakraborty A, Mondal R. Sleep Quality and its various correlates: a community-based study among elderly population in a community development block of Purba Bardhaman district, West Bengal. J Family Med Prim Care. 2020;9(3):1510–6. https://doi.org/10.4103/jfmpc.jfmpc_1021_19.
George S, Paul G, Paul N. Study on sleep quality and associated psychosocial factors among elderly in a rural population of Kerala, India. Int J Community Med Public Health. 2018;5:526–31. https://doi.org/10.18203/2394-6040.IJCMPH20180114.
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. https://doi.org/10.1037/t05178-000.
Wang YM, Chen HG, Song M, Xu SJ, Yu LL, Wang L, et al. Prevalence of insomnia and its risk factors in older individuals: a community-based study in four cities of Hebei Province. China Sleep Med. 2016;19:116–22. https://doi.org/10.1016/j.sleep.2015.10.018.
Chu HS, Oh J, Lee K. The relationship between living arrangements and sleep quality in older adults: Gender differences. Int J Environ Res Public Health. 2022;19(7):3893. https://doi.org/10.3390/ijerph19073893.
Tribl GG, Schmeiser-Rieder A, Rosenberger A, Saletu B, Bolitschek J, Kapfhammer G, et al. Sleeping habits in the Austrian population. Sleep Med. 2002;3(1):21–8. https://doi.org/10.1016/S1389-9457(01)00117-4.
Njawe P. Sleep and rest in patients undergoing cardiac surgery. Nurs Stand. 2003;18(12):33–7. https://doi.org/10.7748/ns2003.12.18.12.33.c3513.
Dogan O, Ertekin S, Dogan S. Sleep quality in hospitalized patients. J Clin Nurs. 2005;14:107–13. https://doi.org/10.1111/j.1365-2702.2004.01011.x.
Wang TJ, Lee SC, Tsay SL, Tung HH. Factors influencing heart failure patients› sleep quality. J Adv Nurs. 2010;66:1730–40. https://doi.org/10.1111/j.1365-2648.2010.05342.x.
Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep. 1995;18(6):425–32. https://doi.org/10.1093/sleep/18.6.425.
Mystakidou K, Parpa E, Tsilika E, et al. The relationship of subjective sleep quality, pain, and quality of life in advanced cancer patients. Sleep. 2007;30(6):737–42. https://doi.org/10.1093/sleep/30.6.737.
McLay L, Jamieson HA, France KG, Schluter PJ. Loneliness and social isolation is associated with sleep problems among older community dwelling women and men with complex needs. Sci Rep. 2021;11(1):4877. https://doi.org/10.1038/s41598-021-83778-w.
World Health Organization: Coronavirus disease (COVID-19) pandemic. (2020). Accessed 25 May 2020.
Sepúlveda-Loyola W, Rodríguez-Sánchez I, Pérez-Rodríguez P, et al. Impact of social isolation due to COVID-19 on health in older people: mental and physical effects and recommendations. J Nutr Health Aging. 2020;24(9):938–47. https://doi.org/10.1007/s12603-020-1500-7.
Chien MY, Chen HC. Poor sleep quality is independently associated with physical disability in older adults. J Clin Sleep Med. 2015;11(03):225–32. https://doi.org/10.5664/jcsm.4532.
Dehghankar L, Ghorbani A, et al. Association of sleep quality with socio-demographic characteristics in elderly referred to health centers in Qazvin. Iran. 2018;20(3):227–32. https://doi.org/10.5350/Sleep.Hypn.2017.19.0154.
Kumar S, Wong PS, Hasan SS, Kairuz T. The relationship between sleep quality, inappropriate medication use and frailty among older adults in aged care homes in Malaysia. PloS One. 2019;14(10):e0224122. https://doi.org/10.1371/journal.pone.0224122.
Zhang C, Xiao S, Lin H, et al. The association between sleep quality and psychological distress among older Chinese adults: a moderated mediation model. BMC Geriatr. 2022;22:35. https://doi.org/10.1186/s12877-021-02711-y.
Xie LQ, Yang BX, Liao YH, Gao GX, Jiang N, Zhou J, et al. Sleep disturbance in older adults with or without mild cognitive impairment and its associated factors residing in rural area. China J Geriatr Psychiatry Neurol. 2021;34(6):632–41. https://doi.org/10.1177/0891988720964249.
Avcı A, Gün M. The effect of activities of daily living and depression symptom level on sleep quality in the elderly with heart failure. Pak Heart J. 2021;54(01):64–72. https://doi.org/10.47144/phj.v54i1.2067.
Pakpour V, Moqaddam M, Hosseiny RS, Salimi S. Quality of Sleep and Daily Activity of the Elderly in Zanjan. J Res Dev Nurs Midwifery. 2016;13(1):62–8. https://doi.org/10.18869/acadpub.jgbfnm.13.1.62.
Wang D, Chen J, Zhou Y, Ma J, Zhou M, Xiao L, et al. Association between sleep duration, sleep quality and hyperlipidemia in middle-aged and older Chinese: The Dongfeng-Tongji Cohort Study. Eur J Prev Cardiol. 2019;26(12):1288–97. https://doi.org/10.1177/2047487319843068.
Chiang GSH, Sim BLH, Lee JJM, Quah JHM. Determinants of poor sleep quality in elderly patients with diabetes mellitus, hyperlipidemia and hypertension in Singapore. Primary Health care Res Dev. 2018;19(6):610–5. https://doi.org/10.1017/S146342361800018X.
Tallo Manafe DR, Rambu Kareri DG, Sasputra IN. A correlation study of quality of sleep with total cholesterol level in the elderly at Budi Agung Elderly Social Welfare Unit, Kupang city, Indonesia. Aujst.com. Accessed 30 Apr 2022.
Adib-Hajbaghery M, Izadi-Avanji F, Akbari H. Quality of sleep and its related risk factors in hospitalized older patients in Kashan’s Hospitals, Iran 2009. Iran J Nurs Midwifery Res. 2012;17(6):414–20.
Isaia G, Corsinovi L, Bo M, Santos-Pereira P, Michelis G, Aimonino N, Zanocchi M. Insomnia among hospitalized elderly patients: prevalence, clinical characteristics and risk factors. Arch Gerontol Geriatr. 2011;52(2):133–7. https://doi.org/10.1016/j.archger.2010.03.001.
Halperin D. Environmental noise and sleep disturbances: A threat to health? Sleep Sci. 2014;7(4):209–12. https://doi.org/10.1016/j.slsci.2014.11.003.
Desaulniers J, Desjardins S, Lapierre S, Desgagné A. Sleep environment and insomnia in elderly persons living at home. J Aging Res. 2018;2018:8053696. https://doi.org/10.1155/2018/8053696.
Acknowledgements
We express our gratitude to NGSMIPS for their support during the conduct of this research study.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Conceptualization: SMG; Methodology; UPN and CS; Data Collection: EST, GM, P; Data Analysis: SMG and UPN; Manuscript writing: EST, GM, P; Supervision: SMG and CS. SMG holds the final responsibility for the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no competing interests.
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki. The study was initiated only after approval was obtained from the Institutional Ethics Committee in the month of November 2021 (Ref. No: NGSMIPS/IEC/20/2020). Consent from participants was obtained prior to their participation in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thomas, E.S., Mathew, G., Prajnashree et al. Assessment of Factors Affecting Sleep Quality in Geriatric Patients: A Cross-sectional Single Centre Study. Sleep Vigilance (2024). https://doi.org/10.1007/s41782-023-00260-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s41782-023-00260-5