Abstract
Decision aids, sometimes known as decision-support tools, are increasingly used to help patients to understand treatment options and to reach an informed decision consistent with their own values, yet methods for their economic evaluation have received limited attention. This is at odds with the increasingly rigorous methods being applied to assess the cost effectiveness of other health technologies. This paper reviews current approaches to evaluating decision aids and proposes a new method for assessing their benefits relative to other interventions in a resource-constrained health system that seeks to improve health, equity and patient satisfaction. Current evaluation frameworks are found to be unsuitable for the economic evaluation of decision aids since their objectives are broader than health maximisation. Decision aids may generate significant non-health benefits such as improved patient knowledge and satisfaction, which cannot be assessed using cost-utility analysis. A stated-preference consultation time trade-off (CTTO) is proposed in which a proportion of hypothetical physician consultation is traded for use of the decision aid. A decision aid provides information for a patient to make an informed choice and therefore may be considered to be a substitute for physician time. The CTTO can be reported in consultation minutes or converted to monetary units using the cost of physician time. These values may be used, alongside the implementation cost, for economic evaluation.
Similar content being viewed by others
There are limitations with current methods to economically evaluate the benefits of decision aids. |
A new approach is proposed that considers decision aids as a substitute for physician consultation to obtain health care information for informed decision making. |
The consultation time-trade off (CTTO) allows the patient to express a preference for using the decision aid within the framework of opportunity cost. |
1 Background
Decision aids, sometimes known as decision-support tools, are increasingly used within the healthcare system. They are employed to support patients to understand treatment options and to reach an informed decision consistent with their own values [1]. They may enhance the shared doctor–patient decision-making process or allow patients to access information at their own leisure rather than within the constraint of a time-limited consultation. Alternatively, patients may not need a trained physician to understand some simpler health decisions, and their use may allow limited physician resources to be reemployed to more complex or more valuable tasks. Thus, decision aids have the potential to empower patients to make informed decisions on their own health and to reduce costs to the healthcare system: two important targets for health policy makers who generally count among their objectives improving health, equity and patient satisfaction. Furthermore, the use of decision aids may be desirable from an ethical and legal perspective by facilitating a higher legal standard of obtaining informed consent [2].
This paper defines a decision aid as a system that helps patients understand their disease management options to make an informed healthcare decision consistent with their values. The decision aid may be designed for use by the patient on their own or for use by the patient and physician together. Decision aids may also refer to systems for physicians to better interact with patients and raise relevant issues. While these may have similar benefits for the patient in terms of improved decision making, they aim to improve the effectiveness of physicians themselves and can be viewed as a separate concept falling within the context of physician training. From a measurement point of view, a patient will find it harder to distinguish between the performance of a physician using the tool and their performance without it.
Evidence that decision aids increase the quality of the decision-making process and decision quality is growing. However, there is limited standardisation of the measurement of their outcomes [3]. Assessments of the benefits of decision aids have focused on reporting improved patient knowledge, experience and satisfaction. A systematic review of the effects of decision aids identified 105 studies and found that decision aids increase people’s involvement and improve knowledge and realistic perception of outcomes [1].
A trial of shared decision-making and risk communication aids found that neither had an impact on patient health outcomes yet concluded that arguments for the techniques can be made from values and ethical principles set against cost [4]. Meanwhile, in a review of the impact of information provision on the health-related quality of life (HRQoL) of cancer survivors, only one of eight studies of interventions to increase health information showed a positive impact on HRQoL [5].
Decision aids have also been evaluated in terms of cost. An observational study of the use of a decision aid in choices on joint-replacement surgery found that the decision aid resulted in reduce rates of elective surgery and lower costs [6]. However, a systematic review of the impact of decision aids on costs to the healthcare system concluded that although patients chose more conservative disease management options, there was limited evidence that implementing decision-support interventions generated savings for the system [7].
Despite the range of outcomes that have been assessed, the full economic evaluation of decision aids provides a challenge for cost-utility analysis (CUA) using quality-adjusted life-years (QALYs), the dominant framework used to economically evaluate health technologies. Consequently, decision aids are rarely economically evaluated with a view to their opportunity cost despite having recognised cost-effectiveness implications for both the healthcare system and patients. This is at odds with increasingly rigorous methods being applied to assess the cost effectiveness of other health technologies [8].
There are currently just three published CUAs of decision aids. Trenaman et al. investigated the cost effectiveness of a decision aid in patients with obstructive sleep apnoea, finding that use of the decision aid was dominated, incurring lower QALYs and higher costs, but noted that current methods to measure the outcomes of decision aids may under-estimate their benefits [9]. Trenaman et al. [10] found that a decision aid for patients considering total joint replacement was dominant, since it was cost saving and produced a small (not statistically significant) QALY gain. Penton et al. [11] developed a hypothetical model of the cost effectiveness of a patient decision aid detailing the benefits and risks of bisphosphonates for patients with osteoporosis, finding the decision aid may have an incremental cost-effectiveness ratio below US$50,000/QALY.
Other economic evaluations of decision aids include Kennedy et al. [12], which separately measured self-reported health status, treatments received and costs in a randomised controlled trial of decision aids for menorrhagia; Cantor et al. [13] which developed a model to calculate the cost per life-year saved of a decision aid for colorectal cancer screening; Tubeuf et al. [14] which assessed the incremental cost per first vaccine uptake; and Hollinghurst et al. [15] which conducted a cost-consequences analysis of a decision aid to support decisions on mode of delivery among women with a previous Caesarean section, where consequences were assessed in terms of decisional conflict and mode of delivery.
In a resource-constrained healthcare system, there is a need for the costs and benefits of interventions to be assessed in a manner that has cross-programme comparability in order to assess the opportunity cost of the forgone alternative to make the best use of limited resources [16]. This paper begins by considering the assessment of benefits of decision aids within the context of CUA, the dominant framework used by health technology assessment (HTA) agencies for economic evaluation. Limitations of this framework for the assessment of decision aids are identified. An alternative framework for the economic evaluation of decision aids is proposed that may be more consistent with the broader reasons that decisions aids are employed within the healthcare system, including health gain, enhanced patient-centred decision making, knowledge of treatment options and decision satisfaction.
2 Current Framework: QALYs
QALYs are the most commonly used outcome in the denominator of the CUA in HTAs in developed countries and are an extra-welfarist approach. QALYs are calculated by weighting each year of life lived using a utility score. Utility scores are anchored so that 1 is perfect health and 0 is equivalent to the state of death.
The term ‘utility’ and its theory is based on von Neumann-Morgenstern (vN-M) utility theory. The normative model for utility theory, the model for how a rational individual ought to behave, is that utility scores represent the strength of an individual’s preference when faced with uncertainty for a given outcome, in this case, a health state [17]. Expected utility is the weighted sum of the utilities of all possible outcomes of a course of action, weighted by the probability of that outcome occurring.
Brouwer et al. [18] summarised the differences between welfarism and extra-welfarism using four characteristics: (1) the outcomes considered relevant in an evaluation, (2) the sources of valuation of the relevant outcomes, (3) the basis of weighting of relevant outcomes and (4) interpersonal comparisons. The QALY can be considered an extra-welfarist approach since:
-
it uses health as a measure of outcome;
-
it permits the use of sources of valuation other than the affected individuals: general public are often preferred, although, in the subsequent example of QALYs for atrial fibrillation, patient preferences are used;
-
it permits the weighting of outcomes according to principles that need not be preference based;
-
it permits interpersonal comparisons of well-being in a variety of dimensions, thus enabling movement beyond Paretian economics.
The purpose of a decision aid is generally to improve the decision-making process to enable the physician and the patient to come to the best choice among management options with different outcomes. The current framework aims to maximise health (QALY). It assumes that patients are ‘health maximisers’: that increased understanding of relative risks and benefits associated with each management option would result in proportionally more patients choosing the decision that is associated with the largest health gain. Such a situation will be represented in CUA as a greater QALY gain (Eq. 1):
where EU is the expected utility, p1 is the probability of outcome 1, u1 is the utility of outcome 1, and n is the number of possible outcomes. The decision aid influences the probability that a particular outcome is chosen.
Robinson and Thomson [19] developed an expected utility approach for use within a decision-analysis framework to integrate patient preferences with probabilistic information, which builds on the above methodology. They lay out the standard gamble as a technique for eliciting preferences for atrial fibrillation and warfarin anticoagulation [19].
3 Limitations with the Current Framework
It is increasingly acknowledged that the use of current evaluation frameworks that focus on health gain may not be appropriate to assess certain interventions in the healthcare system. Payne et al. [20] considered that complex interventions may create challenges in two ways: the intervention may not fit into one of the current appraisal systems, and/or maximising health is not the only objective. I argue that both apply to decision aids.
The QALY framework considers a ‘good’ decision one that produces the greatest health gain. However, decision aids are rarely implemented with the sole or even primary aim of generating a health benefit and the outcomes associated with use of a decision aid are likely to be broader than health.
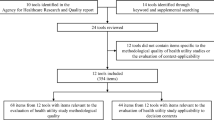
Of the 105 studies of decision aids identified in the previously mentioned systematic review, 71 assessed knowledge, 25 accurate risk perceptions, and 16 informed value-based choice; 63 assessed decisional conflict, ten assessed patient–physician communication, 24 assessed patient participation in decision making, 24 measured the proportion of participants undecided and 19 measured satisfaction with the choice or decision-making process. The impact of the decision aids on general or condition-specific health was only measured in 11 and 7 of the 105 studies, respectively. None of the studies included preference-based health outcomes [1].
A focus on health gain alone is not necessarily consistent with the broader aims of physicians employed in the agency relationship. Agents are there to reduce the information gap present when patients make healthcare decisions or to act on a patient’s behalf by assuming their values. These two concepts have been articulated in the decision-making literature by Bekker et al. [21], which considered an informed decision to be one “using relevant information about the advantages and disadvantages of all possible courses of action” (informed) and “in accordance with personal beliefs” (based on the patient’s values).
Vick and Scott [22] highlighted the complexity of the agency relationship. They identified that being able to talk to the doctor was the most important attribute. Patients tended to prefer more information to less, but females and highly qualified respondents wanted to choose their own treatment [22].
In the current framework, the decision aid’s role is to increase the probability that a certain outcome is chosen to realise a greater QALY gain. As discussed, it is unclear that the objective of health gain is the only or even the main aim of the tool. By excluding other benefits within the broad umbrella of process of care, the utility of decision aids is likely to be undervalued.
4 New Framework: Consultation Time
A new approach to measuring the benefits of decision aids should address the limitations of the current evaluation framework and the wider objectives of decision aids in helping doctors and patients to come to a ‘good’ decision.
A decision aid can be seen as a substitute for physician time and therefore a new approach should consider this framework. The aims of a physician are broader than maximising health and it is unlikely that a physician consultation would be assessed by considering the probability that a certain outcome is chosen in order to generate more QALYs. As well as improving the health of a patient in the long term, in the short term, doctors are a provider of information and a reducer of anxiety regardless of the potential for health gain. Indeed, the agency model of the doctor–patient relationship assumes that physicians are employed by a patient to reduce the information gap between the patient and the disease management options [23].
Adequate physician consultation time has been shown to be associated with quality of care and patient satisfaction as well as being an ethically important dimension of care. Patients seeking help from a doctor who spends more time with them are more likely to have a consultation that includes important elements of care [24]. Patients who believe their consultation lasted longer feel more satisfied [25]. Furthermore, sufficient consultation time is ethically important for the patient–physician relationship and can foster trust, maintain fidelity, demonstrate advocacy and demonstrate respect for the patient [26].
By considering the decision aid in terms of the opportunity cost of physician consultation and as a substitute for physician time, an approach of valuing the tool against the next best alternative is likely to capture a more direct measure of the benefit and include more attributes of the ‘good’ decision (Eq. 2):
where EU is the expected utility, c is the utility of the physician consultation, t is time and d is the utility of the decision aid. The decision aid and physician consultation time are assumed to be perfect substitutes.
The consultation time trade-off (CTTO) requires the patient to choose between use of the decision aid and varying lengths of consultation time with a physician before they reach the point of indifference. A ping-pong technique within a hypothetical 10-min consultation is proposed, with 10 min chosen as a length that patients will be familiar with for a consultation; however, the most appropriate length should be determined in pilot work with patients. The output of the CTTO will be a number of minutes the patient would be willing to trade for use of the tool, equivalent to the opportunity cost of the tool expressed by its displaced alternative: physician consultation time. The approach follows the widely used time trade-off (TTO) [27], which is commonly used to elicit health preferences and forms the basis of the EuroQol 5-Dimensions (EQ-5D) utility scale [28].
As discussed, a successful decision aid and physician consultation have complementary aims, including improved quality of care, patient satisfaction and ethical informed consent and therefore can be considered substitutes. The extent to which the two can be considered perfect substitutes will be determined in part by the attributes of the decision aid, which vary from decision aid to decision aid, and in part by the patient’s own attitude to shared decision making. Imperfect substitutes exhibit variable marginal rates of substitution along the consumer indifference curve. While this issue requires further investigation in real-world testing, it should be noted that the TTO has the same property affecting health state utility values used to estimate QALYs: that there is a curvature of the utility function for duration [29].
5 Application to Economic Evaluation
The benefit of the decision aid expressed in minutes can be directly compared against its cost (likely to include the cost of use and an appropriate proportion of implementation). Such a value would inform the amount of physician time that can be saved and redeployed to more complex tasks elsewhere in the healthcare system.
Alternatively, the number of physician minutes saved can be converted to a monetary value using the local wage rate of the physician that would have been employed on the task. This can then be applied to a cost–benefit analysis to allow comparability across healthcare programmes.
Placing the CTTO framework in a theoretical framework, Table 1 shows that the new approach may be considered within the extra-welfarist framework according to its key features [18], particularly due to its outcomes, which are bounded by consultation satisfaction, due to the possibility to weight outcomes (e.g. by different wage rates across medical specialties) and the possibility to make interpersonal comparisons.
6 Further Questions to Refine New Framework
Converting the CTTO to a monetary value has some implications in terms of the marginal value of a consultation to a patient, and therefore t in Eq. 2. The cost to the healthcare system of a physician consultation is constant if the physician is paid by time, so from the healthcare system perspective, the value of the consultation is constant. However, it may be that, from the patient perspective, the ideal consultation has a diminishing marginal utility because the patient has their most important questions answered first. Further work would be recommended on the marginal value of a consultation if the monetary measure is equated to a patient utility value. The value of the use of decision aids may also be influenced by endogenous factors such as a patient’s health literacy and their preference towards making their own decisions on treatment options compared with delegating the decision to their physician agent [30]. Patients with a higher propensity to make their own decisions on their health condition may find a greater benefit in decision aids. To address the latter, a stratification of decision-making preferences such as the Degner scale could be a useful measure to prospectively determine whether the patient is likely to benefit from use of a decision aid or retrospectively conduct cost–benefit analysis in subgroups of patients with different capacities to benefit [31].
The value of decision aids may also be influenced by exogenous factors such as the quality of the doctor providing the hypothetical substitute consultation. A patient who has experienced higher-quality doctor–patient encounters may be less inclined to trade this for time with the decision aid. This is addressed in the introduction to the tool by emphasising that the consultation is hypothetical and would be sufficient to answer a patient’s questions to their satisfaction.
Literature on the impact of decision aids on consultation time in the real world is unclear: eight studies found no difference, whereas two studies found a median increase of 2.6 min [1]. However, it should be noted that one of the studies reporting an increase included a cognitively challenging standard gamble that may have raised additional questions for respondents [32]. In some cases, this could be that the decision aid is not providing the necessary information and adding confusion that has to be clarified by the doctor. In most cases, the decision aid likely increases the knowledge of the patient, so they have more questions for the doctor. Indeed, evidence that decision aids increase knowledge is strong, and it may be hypothesised that a more knowledgeable patient is more empowered to ask further questions.
In any case, both of these scenarios should be measurable by the theoretical CTTO. A poor decision aid that adds confusion would lead to a first choice of ‘doctor’ (Fig. 1a) followed by agreeing to trade no consultation time for the tool (Fig. 1b). A good decision aid that increases patient knowledge will require a longer physician consultation to compensate the patient.
The preferences derived from the CTTO are those of the patient. Due to the unique combination of attributes of each decision aid, direct user experience is required to make an accurate trade-off. In contrast, economic evaluation of health technologies is often recommended from the public perspective using general public preferences for health states expressed from behind a ‘veil of ignorance’ [33]. This difference may limit the direct comparability of economic evaluation of decision aids using the CTTO with those using other measures that take the public perspective.
Finally, the time at which the CTTO is asked requires consideration in relation to ex ante and ex post utility. Administering the CTTO soon after the decision aid has been used, means that patients are likely to have the clearest recollection of the decision itself. Having said this, the full evaluation of the tool may incorporate the downstream implications of the decision, for example after the patient has undergone an elective surgical procedure and the health consequences have been realised. The former, ex ante, application would be recommended for consistency with expected utility theory. Use of the CTTO after the health consequences have been realised would derive experience utilities [34], which may not be consistent with expected utility used in other healthcare decision-making contexts.
Other possible frameworks could be considered, such as contingent valuation (CV) or discrete-choice experiment (DCE), but I argue that neither of these are satisfactory. The use of CV in evaluations of healthcare is limited since the approach suffers from measurement biases related to the valuation of outcomes that are unfamiliar to respondents, small probabilities and lengthy time horizons of outcomes [35]. Bozic et al. [36] asked patients to rank and attribute a monetary value to decision aids in orthopaedic surgery. However, the study found binary results between patients who had no willingness to pay and those who expressed a willingness to pay in the range of $US50–500.
DCEs lack cross-program comparability, which is important for healthcare decision making. DCEs have addressed this issue by including a monetary attribute. However, this leads to the same challenges for measuring health in monetary terms as faced by CV. Cheraghi-Sohi et al. [37] elicited patient priorities for attributes of primary care consultations in the UK but acknowledged that the monetary attribute may lack validity where patients do not routinely pay for care.
The CTTO remains a conceptual framework and, to operationalise the approach, real-world testing alongside a decision aid would need to be conducted to determine the validity and responsiveness of the CTTO in a patient setting. This would involve the administration of the CTTO in a two-arm trial with and without a decision aid. The length of physician consultation and other outcomes such as knowledge and decision regret would need to be included in the study to establish the validity of the CTTO against established outcome measures.
7 Conclusion
Decision aids have the potential to facilitate healthcare decision making. However, due to the non-health attributes of decision making and the difficulty associating the decision with future health gain (or loss), current methods of economic evaluation are ill suited to evaluate them. While there may be practical reasons for conducting a CUA on decision aids, previous work has shown the approach to be incapable of capturing the full benefits of such interventions. The proposed new approach based on trading off physician consultation time allows decision aids to be economically evaluated within the framework of opportunity cost, which has the potential to support the healthcare system in achieving its aims of improving health, equity and patient satisfaction.
References
Stacey D, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:Cd001431.
Washington State, Blue Ribbon Commission on Health Care Costs and Access. 2007.
Sepucha KR, et al. Establishing the effectiveness of patient decision aids: key constructs and measurement instruments. BMC Med Inform Decis Mak. 2013;13(2):S12.
Edwards A, et al. Patient-based outcome results from a cluster randomized trial of shared decision making skill development and use of risk communication aids in general practice. Fam Pract. 2004;21(4):347–54.
Husson O, Mols F, van de Poll-Franse LV. The relation between information provision and health-related quality of life, anxiety and depression among cancer survivors: a systematic review. Ann Oncol. 2010.
Arterburn D, et al. Introducing decision aids at Group Health was linked to sharply lower hip and knee surgery rates and costs. Health Aff (Millwood). 2012;31(9):2094–104.
Walsh T, et al. Undetermined impact of patient decision support interventions on healthcare costs and savings: systematic review. BMJ. 2014;348:g188.
NICE, Guide to the methods of technology appraisal. 2013, National Institute for Health and Clinical Excellence.
Trenaman L, et al. Exploring the potential cost-effectiveness of patient decision aids for use in adults with obstructive sleep apnea: a case study. Med Decis Making. 2015;35(5):671–82.
Trenaman L, et al. Decision aids for patients considering total joint replacement: a cost-effectiveness analysis alongside a randomised controlled trial. Osteoarthr Cartil. 2017;25(10):1615–22.
Penton H, et al. Potential cost-effectiveness for using patient decision aids to guide osteoporosis treatment. Osteoporos Int. 2016;27(9):2697–707.
Kennedy AD, et al. Effects of decision aids for menorrhagia on treatment choices, health outcomes, and costs: a randomized controlled trial. JAMA. 2002;288(21):2701–8.
Cantor SB, et al. A framework for evaluating the cost-effectiveness of patient decision aids: a case study using colorectal cancer screening. Prev Med. 2015;77:168–73.
Tubeuf S, et al. Cost effectiveness of a web-based decision aid for parents deciding about MMR vaccination: a three-arm cluster randomised controlled trial in primary care. Br J Gen Pract. 2014;64(625):e493–9.
Hollinghurst S, et al. Economic evaluation of the DiAMOND randomized trial: cost and outcomes of 2 decision aids for mode of delivery among women with a previous cesarean section. Med Decis Making. 2010;30(4):453–63.
Drummond MF. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford medical publications. Oxford: Oxford University Press; 2005.
Hunter RM, et al. An educational review of the statistical issues in analysing utility data for cost-utility analysis. Pharmacoeconomics. 2015;33(4):355–66.
Brouwer WBF, et al. Welfarism vs. extra-welfarism. J Health Econ. 2008;27(2):325–38.
Robinson A, Thomson RG. The potential use of decision analysis to support shared decision making in the face of uncertainty: the example of atrial fibrillation and warfarin anticoagulation. Qual Health Care. 2000;9(4):238–44.
Payne K, McAllister M, Davies LM. Valuing the economic benefits of complex interventions: when maximising health is not sufficient. Health Econ. 2013;22(3):258–71.
Bekker H, et al. Informed decision making: an annotated bibliography and systematic review. Health Technol Assess. 1999;3(1):1–156.
Vick S, Scott A. Agency in health care. Examining patients’ preferences for attributes of the doctor-patient relationship. Journal of health economics. 1998;17(5):587–605.
Gafni A, Charles C, Whelan T. The physician-patient encounter: the physician as a perfect agent for the patient versus the informed treatment decision-making model. Soc Sci Med. 1998;47(3):347–54.
Wilson A, Childs S. The relationship between consultation length, process and outcomes in general practice: a systematic review. Br J Gen Pract. 2002;52(485):1012–20.
Cape J. Consultation length, patient-estimated consultation length, and satisfaction with the consultation. Br J Gen Pract. 2002;52(485):1004–6.
Braddock CH 3rd, Snyder L. The doctor will see you shortly. The ethical significance of time for the patient-physician relationship. J Gen Intern Med. 2005;20(11):1057–62.
Torrance GW. Measurement of health state utilities for economic appraisal. J Health Econ. 1986;5(1):1–30.
Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35(11):1095–108.
Attema AE, Brouwer WB. On the (not so) constant proportional trade-off in TTO. Qual Life Res. 2010;19(4):489–97.
McCaffery KJ, et al. Addressing health literacy in patient decision aids. BMC Med Inf Decis Mak. 2013;13(Suppl 2):S10–1.
Degner LF, Sloan JA. Decision making during serious illness: what role do patients really want to play? J Clin Epidemiol. 1992;45(9):941–50.
Thomson RG, et al. A patient decision aid to support shared decision-making on anti-thrombotic treatment of patients with atrial fibrillation: randomised controlled trial. Qual Saf Health Care. 2007;16(3):216–23.
Gold MR. Cost-effectiveness in health and medicine, xxiii. New York: Oxford University Press; 1996.
Kahneman D, Wakker PP, Sarin R. Back to Bentham? Explorations of Experienced Utility. Q J Econ. 1997;112(2):375–406.
Cookson R. Willingness to pay methods in health care: a sceptical view. Health Econ. 2003;12(11):891–4.
Bozic KJ, et al. Patient, surgeon, and healthcare purchaser views on the use of decision and communication aids in orthopaedic surgery: a mixed methods study. BMC Health Serv Res. 2014;14:366.
Cheraghi-Sohi S, et al. What patients want from primary care consultations: a discrete choice experiment to identify patients’ priorities. Ann Fam Med. 2008;6(2):107–15.
Acknowledgements
The author would like to thank Gary Rubin PhD and Shepley Orr DPhil for their helpful comments on an earlier version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The author received no specific funding for the preparation of this manuscript. TB is supported by a Boya Fellowship from Peking University.
Conflicts of Interest
TB has no conflicts of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Butt, T. Measuring the Benefits of Decision Aids for Economic Evaluation. PharmacoEconomics Open 3, 143–150 (2019). https://doi.org/10.1007/s41669-018-0087-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-018-0087-y