Abstract
Purpose
Fear and anxiety for pain makes people avoid dental treatments. The main aim of the study was to evaluate the acceptance and efficiency of pulpal anesthesia induced by photobiomodulation (PBM) therapy, during conventional cavity preparation of decayed permanent teeth.
Methods
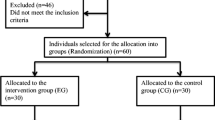
Patients of 11–25 years old (n = 24) were included in a split-mouth and randomized crossover clinical study. Conventional cavity treatment was made in two contralateral decayed teeth of the same arch, in similar extent of caries ICDAS 4 or 5, of each patient, one under conventional local anesthesia by pharmacological agents (control group) and another under pulpal anesthesia induced by PBM therapy (PBM group). The diode laser irradiation parameters were 810 nm wavelength, CW, non-contact mode, 600 μm hand piece, 6 mm, 250 mW, 120 s (60 s buccal, 60 s lingual), 0.88 W/cm2, 106.2 J/cm2, 30 J. The Wong Baker’s faces pain scale was used for assessing the discomfort levels, whereas the acceptance was obtained by asking the preference of the patient. Data were statistically compared using the Mann-Whitney Wilcoxon’s test (p < 0.05).
Results
For laser anesthesia (PBM group), the mean discomfort valued was 1.37 ± 1.55, similar to that for injection anesthesia (control group) which was 1.25 ± 1.53 (p = 0.59), independently of the ICDAS classification. Twenty-two out of 24 patients replied that they prefer the method with the laser (91.7%).
Conclusions
This pilot study demonstrated the clinical effectiveness and acceptance of PBM induces pulpal anesthesia for cavity preparation of decayed permanent teeth and deserves further research and development.


Similar content being viewed by others
References
Gordon D, Heimberg RG, Tellez M, Ismail AI (2013) A critical review of approaches to the treatment of dental anxiety in adults. J Anxiety Disord 27:365–378. doi:10.1016/j.janxdis.2013.04.002
Pawlicki RE (1991) Psychological/behavioral techniques in managing pain and anxiety in the dental patient. Anesth Prog 38:120–127
Corah NL, O’Shea RM, Ayer WA (1985) Dentists’ management of patients’ fear and anxiety. J Am Dent Assoc 110:734–736
Milgrom P, Coldwell SE, Getz T, Weinstein P, Ramsay DS (1997) Four dimensions of fear of dental injections. J Am Dent Assoc 128:756–766
Milgrom P, Fiset L, Melnick S, Weinstein P (1988) The prevalence and practice management consequences of dental fear in a major US city. J Am Dent Assoc 116:641–647
Gatchel RJ, Ingersoll BD, Bowman L, Robertson MC, Walker C (1983) The prevalence of dental fear and avoidance: a recent survey study. J Am Dent Assoc 107:609–610
Byers MR (1984) Dental sensory receptors. Int Rev Neurobiol 25:39–94
Malamed SF, Gagnon S, Leblanc D (2000) Efficacy of articaine: a new amide local anaesthetic. J Am Dent Assoc 131:635–642
Rahn R, Hauzeneder W, Flanze L (1991) Efficiency of a 2% epinephrine-free Articain solution (Ultracain 2%) for dental local anaesthesia. Dtsch Stomatol 41:379–382
Khoury F, Hinterthan A, Schürmann J, Arns H (1991) Clinical comparative study of local anesthetics. Random double blind study with four commercial preparations. Dtsch Zahnarztl Z 46:822–824
Haas DA (2002) An update on local anesthetics in dentistry. J Can Dent Assoc 68:546–551
Daubländer M, Müller R, Lipp MD (1997) The incidence of complications associated with local anesthesia in dentistry. Anesth Prog 44:132–141
Cummings DR, Yamashita DD, McAndrews JP (2011) Complications of local anesthesia used in oral and maxillofacial surgery. Oral Maxillofac Surg Clin North Am 23:369–377. doi:10.1016/j.coms.2011.04.009
Malamed SF (2000) The possible secondary effects in cases of local anesthesia. Rev Belg Med Dent 55:19–28
Keller U, Hibst R, Geurtsen W, Schilke R, Heidemann D, Klaiber B, Raab WH (1998) Erbium:YAG laser application in caries therapy. Evaluation of patient perception and acceptance. J Dent 26:649–656
Tanboga I, Eren F, Altinok B, Peker S, Ertugral F (2011) The effect of low level laser therapy on pain during dental tooth-cavity preparation in children. Eur Arch Paediatr Dent 12:93–95
Zeredo JL, Sasaki KM, Takeuchi Y, Toda K (2005) Antinociceptive effect of Er:YAG laser irradiation in the orofacial formalin test. Brain Res 1032:149–153
Karu T (1999) Primary and secondary mechanisms of action of visible to near-IR radiation on cells. J Photochem Photobiol B 49:1–17
Tsuchiya K, Kawatani M, Takeshige C, Matsumoto I (1994) Laser irradiation abates neuronal responses to nociceptive stimulation of rat-paw skin. Brain Res Bull 34:369–374
Pozza DH, Fregapani PW, Weber JB, de Oliveira MG, de Oliveira MA, Ribeiro Neto N, de Macedo Sobrinho JB (2008) Analgesic action of laser therapy (LLLT) in an animal model. Med Oral Patol Oral Cir Bucal 13:E648–E652
Chow R, Armati P, Laakso EL, Bjordal JM, Baxter GD (2011) Inhibitory effects of laser irradiation on peripheral mammalian nerves and relevance to analgesic effects: a systematic review. Photomed Laser Surg 29:365–381. doi:10.1089/pho.2010.2928
Yachnev IL, Plakhova VB, Podzorova SA, Shelykh TN, Rogachevsky IV, Krylov BV (2012) Mechanism of pain relief by low-power infrared irradiation: ATP is an IR-target molecule in nociceptive neurons. Med Chem 8:14–21
Tsuchiya K, Kawatani M, Takeshige C, Sato T, Matsumoto I (1993) Diode laser irradiation selectively diminishes slow component of axonal volleys to dorsal roots from the saphenous nerve in the rat. Neurosci Lett 161:65–68
Chow RT, David MA, Armati PJ (2007) 830 nm laser irradiation induces varicosity formation, reduces mitochondrial membrane potential and blocks fast axonal flow in small and medium diameter rat dorsal root ganglion neurons: implications for the analgesic effects of 830 nm laser. J Peripher Nerv Syst 12:28–39
Wakabayashi H, Hamba M, Matsumoto K, Tachibana H (1993) Effect of irradiation by semiconductor laser on responses evoked in trigeminal caudal neurons by tooth pulp stimulation. Lasers Surg Med 13:605–610
Nagasawa A (1984) The anaesthetic effect of Nd:YAG laser in dental treatment. Jpn J Med Bio Eng 22:830–831
Chan A, Armati P, Moorthy AP (2012) Pulsed Nd: YAG laser induces pulpal analgesia: a randomized clinical trial. J Dent Res 91:79S–84S
Dederich DN (1993) Laser/tissue interaction: what happens to laser light when it strikes tissue? J Am Dent Assoc 124:57–61
Pitts NB (2004) ‘ICDAS’—an international system for caries detection and assessment being developed to facilitate caries epidemiology, research and appropriate clinical management. Community Dent Health 21:193–198
Jablonski-Momeni A, Stachniss V, Ricketts DN, Heinzel-Gutenbrunner M, Pieper K (2008) Reproducibility and accuracy of the ICDAS-II for detection of occlusal caries in vitro. Caries Res 42:79–87. doi:10.1159/000113160
Shoaib L, Deery C, Ricketts DN, Nugent ZJ (2009) Validity and reproducibility of ICDAS II in primary teeth. Caries Res 43:442–448. doi:10.1159/000258551
Zach L, Cohen G (1965) Pulp response to externally applied heat. Oral Surg Oral Med Oral Pathol 19:515–530
Antczak-Bouckoms AA, Tulloch JF, Berkey CS (1990) Split-mouth and cross-over designs in dental research. J Clin Periodontol 17:446–453
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This pilot study was conducted in accordance with the principles of the Helsinki Declaration of 1975, as revised in 2000.
Rights and permissions
About this article
Cite this article
Efthymiou, A., Marques, M.M., Franzen, R. et al. Acceptance and efficiency of anesthesia by photobiomodulation therapy during conventional cavity preparation in permanent teeth: a pilot randomized crossover clinical study. Laser Dent Sci 1, 65–71 (2017). https://doi.org/10.1007/s41547-017-0007-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41547-017-0007-y