Abstract
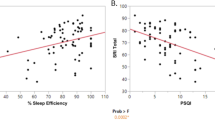
Substance use disorder (SUD) can have circadian characteristics and individuals with evening chronotype are more prone to addiction. In this study, the effect of chronotypes on the treatment outcomes of SUD was investigated. The study included 66 patients who were diagnosed with SUD according to DSM-5. Two clinical interviews were conducted at 6-month intervals, and remission/relapse status was evaluated at the second interview. The Structured Clinical Interview Form for DSM-IV Axis I Disorders (SCID-I), Addiction Profile Index Practitioner Form, Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), Pittsburg Sleep Quality Index and Morningness-Eveningness Questionnaire (MEQ) were applied to the patients. MEQ scores of relapsed patients were found to be different in terms of eveningness than those in remission (45.62 ± 8.70 versus 49.75 ± 7.60, p = 0.045). As the craving and addiction profile index total scores (addiction severity) increased, eveningness chronotype scores also increased (r = − 0.387 and r = − 0.286, respectively). The mean scores of craving and BDI were higher in relapsed patients compared to those in remission (p = 0.003 and p = 0.015, respectively). Our results suggest that patients with SUD had a lower morningness chronotype than the general population; additionally, more relapsed patients had an eveningness chronotype. Thus, chronotypes may play a role in the onset, prevention, and treatment outcome of SUD.
Similar content being viewed by others
References
Reinberg A, Ashkenazi I. Concepts in human biological rhythms. Dialogues Clin Neurosci. 2003;5:327–42.
Falcón E, McClung CA. A role for the circadian genes in drug addiction. Neuropharmacology. 2009;56:91–6.
Baik JH. Dopamine signaling in reward-related behaviors. Front Neural Circuits. 2013;7:152.
Lüscher C. Drug-evoked synaptic plasticity causing addictive behavior. J Neurosci. 2013;33:17641–6.
Webb IC. Circadian rhythms and substance abuse: chronobiological considerations for the treatment of addiction. Curr Psychiatry Rep. 2017;19:12.
McClung CA. Circadian genes, rhythms and the biology of mood disorders. Pharmacol Ther. 2007;114:222–32.
Adan A. Chronotype and personality factors in the daily consumption of alcohol and psychostimulants. Addiction (Abingdon, England). 1994;89:455–62.
Giannotti F, Cortesi F, Sebastiani T, Ottaviano S. Circadian preference, sleep and daytime behaviour in adolescence. J Sleep Res. 2002;11:191–9.
Prat G, Adan A. Influence of circadian typology on drug consumption, hazardous alcohol use, and hangover symptoms. Chronobiol Int. 2011;28:248–57.
Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol Int. 2006;23:497–509.
Wittmann M, Paulus M, Roenneberg T. Decreased psychological well-being in late “chronotypes” is mediated by smoking and alcohol consumption. Subst Use Misuse. 2010;45:15–30.
Kervran C, Fatseas M, Serre F, Taillard J, Beltran V, Leboucher J, et al. Association between morningness/eveningness, addiction severity and psychiatric disorders among individuals with addictions. Psychiatry Res. 2015;229:1024–30.
Teneggi V, Tiffany ST, Squassante L, Milleri S, Ziviani L, Bye A. Effect of sustained-release (SR) bupropion on craving and withdrawal in smokers deprived of cigarettes for 72 h. Psychopharmacology. 2005;183:1–12.
Ren ZY, Zhang XL, Liu Y, Zhao LY, Shi J, Bao Y, et al. Diurnal variation in cue-induced responses among protracted abstinent heroin users. Pharmacol Biochem Behav. 2009;91:468–72.
Peles E, Hetzroni T, Bar-Hamburger R, Adelson M, Schreiber S. Melatonin for perceived sleep disturbances associated with benzodiazepine withdrawal among patients in methadone maintenance treatment: a double-blind randomized clinical trial. Addiction (Abingdon, England). 2007;102:1947–53.
Han J, Xu Y, Yu C-X, Shen J, Wei Y-M. Melatonin reverses the expression of morphine-induced conditioned place preference through its receptors within central nervous system in mice. Eur J Pharmacol. 2008;594:125–31.
Raghavendra V, Kulkarni SK. Reversal of morphine tolerance and dependence by melatonin: possible role of central and peripheral benzodiazepine receptors. Brain Res. 1999;834:178–81.
Lewis TF. Substance abuse and addiction treatment: practical application of counseling theory. London: Pearson Higher Ed; 2013.
Çorapçıoğlu A, Aydemir Ö, Yıldız M, Esen A, Köroğlu IV E. DSM-IV Eksen I Bozuklukları (SCID-I) için yapılandırılmış klinik görüşme, klinik versiyon. Ankara: Hekimler yayın birliği. 1999.
Ögel K, Evren C, Karadağ F, Gürol T. Bağımlılık Profil İndeksi’nin (BAPİ) geliştirilmesi, geçerlik ve güvenilirliği. Turk Psikiyatri Derg. 2012;23:264–73.
Hisli N. Beck depresyon envanterinin universite ogrencileri icin gecerliligi, guvenilirligi (A reliability and validity study of beck depression inventory in a university student sample). J Psychol. 1989;7:3–13.
Ulusoy M, Sahin NH, Erkmen H. The beck anxiety inventory: psychometric properties. J Cognit Psychother. 1998;12:163.
Agargun M. Pittsburgh uyku kalitesi indeksinin gecerligi ve guvenirligi. Turk Psikiyatri Dergisi. 1996;7:107–15.
Agargun MY, Cilli AS, Boysan M, Selvi Y, Gulec M, Kara H. Turkish version of morningness-eveningness questionnaire (MEQ). Sleep Hypn. 2007;9:16.
DSM-V. Diagnostic and statistical manual of mental disorders (DSM-5®). Arlington: American Psychiatric Pub; 2013.
Cornelius JR, Maisto SA, Pollock NK, Martin CS, Salloum IM, Lynch KG, et al. Rapid relapse generally follows treatment for substance use disorders among adolescents. Addict Behav. 2003;28:381–6.
Lopes-Rosa R, Kessler FP, Pianca TG, Guimaraes L, Ferronato P, Pagnussat E, et al. Predictors of early relapse among adolescent crack users. J Addict Dis. 2017;36:136–43.
Fleury MJ, Djouini A, Huỳnh C, Tremblay J, Ferland F, Ménard JM, et al. Remission from substance use disorders: a systematic review and meta-analysis. Drug Alcohol Depend. 2016;168:293–306.
Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2014. https://doi.org/10.1002/14651858.CD002207.pub4.
Breese GR, Sinha R, Heilig M. Chronic alcohol neuroadaptation and stress contribute to susceptibility for alcohol craving and relapse. Pharmacol Ther. 2011;129:149–71.
Drummond DC. Theories of drug craving, ancient and modern. Addiction (Abingdon, England). 2001;96:33–46.
Festinger DS, Rubenstein DF, Marlowe DB, Platt JJ. Relapse: Contributing factors, causative models, and empirical considerations. In: Tims FM, Leukefeld CG, Platt JJ, editors. Relapse and recovery in addictions. Yale University Press; 2001. p. 122–42.
Tate SR, Wu J, McQuaid JR, Cummins K, Shriver C, Krenek M, et al. Comorbidity of substance dependence and depression: role of life stress and self-efficacy in sustaining abstinence. Psychol Addict Behav. 2008;22:47.
Bachman JG, Freedman-Doan P, O’Malley PM, Schulenberg JE, Johnston LD. Revisiting marriage effects on substance use among young adults. Ann Arbor, MI: Institute for Social Research. 2008, (Monitoring the Future Occasional Paper No. 68).
Scott KM, Wells JE, Angermeyer M, Brugha TS, Bromet E, Demyttenaere K, et al. Gender and the relationship between marital status and first onset of mood, anxiety and substance use disorders. Psychol Med. 2010;40:1495–505.
Vignesh BT, Singh AK, Mohan SK, Murthy S, Joshi A. Association between socio-demographics and alcohol dependence among individuals living in an Indian setting. Glob J Health Sci. 2014;6:16–26.
Liu J, McDonough D, Wang Y, Zhou Y, Gao Z, Zhou C. Investigating the associations among drug dependents’ family function and exercise attitudes: marital status differences. Int J Environ Res Public Health. 2020;17:8111.
Habibi M, Darharaj M, Kelly A, Shahmiri H, Malekianjabali M, Kheirolomoom S. Drug use in soldiers: family and peer contextual associations. Subst Use Misuse. 2017;52:1357–63.
Carek PJ, Laibstain SE, Carek SM. Exercise for the treatment of depression and anxiety. Int J Psychiatry Med. 2011;41:15–28.
Tantimonaco M, Ceci R, Sabatini S, Catani MV, Rossi A, Gasperi V, et al. Physical activity and the endocannabinoid system: an overview. Cell Mol Life Sci. 2014;71:2681–98.
Smith MA, Lynch WJ. Exercise as a potential treatment for drug abuse: evidence from preclinical studies. Front Psychol. 2012;2:82.
Adan A, Natale V, Caci H. Cognitive strategies and circadian typology. In: Progress in circadian rhythm research. 2008. pp. 141–61.
Adan A, Lachica J, Caci H, Natale V. Circadian typology and temperament and character personality dimensions. Chronobiol Int. 2010;27:181–93.
Adan A, Natale V, Caci H, Prat G. Relationship between circadian typology and functional and dysfunctional impulsivity. Chronobiol Int. 2010;27:606–19.
Teneggi V, Tiffany ST, Squassante L, Milleri S, Ziviani L, Bye A. Smokers deprived of cigarettes for 72 h: effect of nicotine patches on craving and withdrawal. Psychopharmacology. 2002;164:177–87.
Webb IC, Lehman MN, Coolen LM. Diurnal and circadian regulation of reward-related neurophysiology and behavior. Physiol Behav. 2015;143:58–69.
Lai HMX, Cleary M, Sitharthan T, Hunt GE. Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: a systematic review and meta-analysis. Drug Alcohol Depend. 2015;154:1–13.
Decker KP, Peglow SL, Samples CR, Cunningham TD. Long-term outcomes after residential substance use treatment: relapse, morbidity, and mortality. Mil Med. 2017;182:e1589–95.
Antypa N, Vogelzangs N, Meesters Y, Schoevers R, Penninx BW. Chronotype associations with depression and anxiety disorders in a large cohort study. Depress Anxiety. 2016;33:75–83.
Hidalgo MP, Caumo W, Posser M, Coccaro SB, Camozzato AL, Chaves ML. Relationship between depressive mood and chronotype in healthy subjects. Psychiatry Clin Neurosci. 2009;63:283–90.
Kitamura S, Hida A, Watanabe M, Enomoto M, Aritake-Okada S, Moriguchi Y, et al. Evening preference is related to the incidence of depressive states independent of sleep-wake conditions. Chronobiol Int. 2010;27:1797–812.
Levandovski R, Dantas G, Fernandes LC, Caumo W, Torres I, Roenneberg T, et al. Depression scores associate with chronotype and social jetlag in a rural population. Chronobiol Int. 2011;28:771–8.
Merikanto I, Kronholm E, Peltonen M, Laatikainen T, Vartiainen E, Partonen T. Circadian preference links to depression in general adult population. J Affect Disord. 2015;188:143–8.
Park CI, An SK, Kim HW, Koh MJ, Namkoong K, Kang JI, et al. Relationships between chronotypes and affective temperaments in healthy young adults. J Affect Disord. 2015;175:256–9.
Fares S, Hermens DF, Naismith SL, White D, Hickie IB, Robillard R. Clinical correlates of chronotypes in young persons with mental disorders. Chronobiol Int. 2015;32:1183–91.
Gaspar-Barba E, Calati R, Cruz-Fuentes CS, Ontiveros-Uribe MP, Natale V, De Ronchi D, et al. Depressive symptomatology is influenced by chronotypes. J Affect Disord. 2009;119:100–6.
Lemoine P, Zawieja P, Ohayon MM. Associations between morningness/eveningness and psychopathology: an epidemiological survey in three in-patient psychiatric clinics. J Psychiatr Res. 2013;47:1095–8.
Broms U, Pitkäniemi J, Bäckmand H, Heikkilä K, Koskenvuo M, Peltonen M, et al. Long-term consistency of diurnal-type preferences among men. Chronobiol Int. 2014;31:182–8.
Taillard J, Philip P, Chastang JF, Bioulac B. Validation of Horne and Ostberg morningness-eveningness questionnaire in a middle-aged population of French workers. J Biol Rhythms. 2004;19:76–86.
Lee JH, Kim IS, Kim SJ, Wang W, Duffy JF. Change in individual chronotype over a lifetime: a retrospective study. Sleep Med Res. 2011;2:48–53.
Rogers HL, Reilly SM. A survey of the health experiences of international business travelers: part one—physiological aspects. AAOHN J. 2002;50:449–59.
Trinkoff AM, Storr CL. Work schedule characteristics and substance use in nurses. Am J Ind Med. 1998;34:266–71.
Perreau-Lenz S, Vengeliene V, Noori HR, Merlo-Pich EV, Corsi MA, Corti C, et al. Inhibition of the casein-kinase-1-epsilon/delta prevents relapse-like alcohol drinking. Neuropsychopharmacology. 2012;37:2121.
Kantermann T, Juda M, Merrow M, Roenneberg T. The human circadian clock’s seasonal adjustment is disrupted by daylight saving time. Curr Biol. 2007;17:1996–2000.
Lahti TA, Leppämäki S, Lönnqvist J, Partonen T. Transitions into and out of daylight saving time compromise sleep and the rest-activity cycles. BMC Physiol. 2008;8:1–6.
Author information
Authors and Affiliations
Contributions
Conceptualization: OAC, ASC; Methodology: OAC, ABY, HB, ŞG; Formal analysis and investigation: OAC, ASC, ABY; Writing—original draft preparation: OAC, ASC; Writing—review and editing: ABY, HB, ŞG; Resources: OAC, ASC; Supervision: ABY, HB, ŞG.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors report any conflict of interest for this article.
Ethical approval
Ethical approval for the study was obtained from the Ethics Committee of Faculty of Medicine of Sakarya University. Completed voluntary informed consent forms were obtained from the patients prior to the start of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ciner, O.A., Cilli, A.S., Yazici, A.B. et al. The effect of chronotypes on follow-up outcomes of patients with substance use disorder. Sleep Biol. Rhythms 22, 247–258 (2024). https://doi.org/10.1007/s41105-023-00496-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-023-00496-8