Abstract
Health effects of weekend catch-up sleep (CUS) could differ depending on both the ability to obtain sufficient sleep during weekdays and amount of weekend CUS required to compensate for sleep lost during the week. Using data from 3128 middle-aged (40–64 years) participants of the Sleep Heart Health Study, we examined the longitudinal association of these two aspects of sleep with all-cause mortality. CUS was calculated as the difference in self-reported habitual sleep duration between weekends and weekdays, and classified into no, short (1 h), and long (2 h or more) CUS. Polysomnography-measured total sleep time, representing the ability to obtain sufficient sleep, was classified into short (< 360 min) or normal (≥ 360 min) sleep durations. We estimated multivariable-adjusted mortality hazard ratios (HRs) and 95% confidence intervals (CIs) for six groups divided by the extent of CUS and sleep duration. Participants were followed up for a median (interquartile range) of 12.3 (11.3–13.5) years. Short weekend CUS with normal sleep duration was associated with lower mortality compared to no CUS with normal sleep duration (HR, 0.48; 95% CI 0.27–0.83). When stricter cutoffs were applied for sleep durations, while the protective effect of short CUS with normal sleep duration (≥ 390 min) was strengthened (HR, 0.36; 95% CI 0.17–0.78), the harmful effect of short CUS with short sleep duration (< 330 min) emerged (HR, 1.84; 95% CI 1.08–3.14). Results highlight the importance of balancing sleep ability and CUS. Sufficient sleep may reduce weekday sleep debt and only a short CUS would be required on weekends, improving mortality in middle-aged adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Insufficient sleep has been recognized as a risk factor for human health outcomes, including obesity, diabetes, hypertension, cardiovascular disease, cognitive decline, and all-cause mortality [1, 2]. However, consistently sleeping as long as needed is still a challenge for many of us, because we often voluntarily curtail sleep to maximize time for daily social activities. Nightly sleep loss accumulates over days, resulting in a buildup of chronic sleep loss (sleep debt). Although extending sleep, or catch-up sleep (CUS), on weekends is a common way of making up for sleep lost during the week, it is currently debated whether weekend CUS could cancel out some of the health risks associated with sleep loss and circadian misalignment [3,4,5].
Experimental studies have shown that weekend CUS could not make up for even one hour of nightly sleep lost during weekdays [6, 7]. On the contrary, an epidemiological study has suggested that weekend compensatory sleep mitigates the harmful effect of short sleep during weekdays on all-cause mortality [4]. These mixed findings suggest that the health effects of weekend compensatory sleep could differ depending on both the amount of CUS and one’s ability to obtain sufficient sleep. The ability to obtain sufficient sleep could be generated under the control of homeostatic and circadian drives, both of which are interfered with by aging, social constraints, and/or certain pathologies [8]. Following the homeostatic regulation of sleep, it is plausible that the greater the weekday sleep reduction, the greater the amount of weekend CUS, reflecting sleep debt. Therefore, there may be a threshold value for lost sleep during weekdays, below which weekend CUS could successfully pay off the sleep debt. Additionally, the ability to obtain a certain amount of sleep and the sufficient opportunity to sleep during weekdays may be vital to minimize sleep debt. Obtaining sufficient sleep during weekdays decreases the degree to which CUS is required on weekends. Moreover, consistent with the idea that almost everyone is constantly sleep deprived and carries some amount of sleep debt [7, 9, 10], weekend sleep extension may have a favorable effect [7]. Nonetheless, this possible favorable effect is more likely to emerge among individuals who maintain their ability to obtain sufficient sleep and need only a small amount of weekend CUS within their controllable range, than among those who are impaired in their ability to obtain sufficient sleep or need a greater amount of weekend CUS beyond their controllable range. As with other physiological disciplines, an objective measurement of sleep duration (e.g., polysomnography [PSG]), compared to self-reports of sleep duration, could allow for a more reliable assessment of the ability to obtain sufficient sleep. Although sleep experts recommend sufficient sleep duration for seven to nine hours per day for young to middle-aged adults [11], a considerable mismatch between self-reported and objectively measured sleep duration has been found across studies, with the former being longer on average than the latter [1, 12]. This subjective–objective sleep discrepancy is likely, at least partly, to result from a general tendency to overestimate one’s sleep duration subjectively11. We investigated the combined effects of the degree of weekend CUS and PSG-measured sleep duration on long-term mortality outcomes in middle-aged (40–64 years) adults using data from the Sleep Heart Health Study (SHHS), a multicenter population-based prospective cohort study [13, 14].
Methods
Participants
All data were derived from the SHHS and other details of the study are available in previously published literature [13]. The study was performed in accordance with the Helsinki Declaration, and each participant provided written informed consent. A total of 6441 participants aged 40 years and older were enrolled from existing cohorts and underwent the baseline examination between 1995 and 1998. Of these, 3128 middle-aged (40–64 years) participants who underwent overnight PSG were included in the current investigation. Across community-based cohorts, including the SHHS, older adults less frequently sleep longer on weekends than on weekdays [1, 4, 15, 16]. Therefore, we only included middle-aged adults in our analysis. The distinction between middle-aged and older adults relied on the National Sleep Foundation’s expert consensus age categories [17]. The current project was approved in April 2020 by the Ethics Committee of the National Center of Neurology and Psychiatry (project number: A2020-012). All analyzed data are publicly available (sleepdata.org). This study is reported following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cohort studies.
Measures
Objective sleep measure
We employed participants’ PSG-measured total sleep time (TST) as an objective index of the ability to maintain sleep. An unattended, portable in-home PSG was conducted during the baseline examination, using the Compumedics P Series System (Abbotsford, Victoria, Australia). The vast majority of participants underwent in-home PSG on a weekday (n = 2866, 91.6%). Standard PSG characteristics, including TST (total time in non-rapid eye-movement stages 1–3 and rapid eye movement sleep), were evaluated based on the SHHS Reading Center manual of operations, as described previously [18].
Subjective sleep measure
During the baseline examination, the participants were asked to report their habitual sleep duration at night on weekdays (or workdays) and on weekends (or non-workdays) in hours.
Primary exposure
The primary exposures were a specific amount of habitual weekend extra sleep (short CUS, or long CUS vs. no CUS) and short sleep duration determined on a PSG night (vs. normal sleep duration), both of which were obtained at the baseline examination. The primary definition of short sleep duration was TST of less than 360 min (6 h) on PSG, a cutoff commonly used to define objectively short sleep among adults in epidemiological studies, including the SHHS [19,20,21]. Additionally, we applied two stricter cutoffs for short and normal sleep durations (< 330 min, and ≥ 390 min, respectively) to explain how impaired or maintained sleep affects the associations between weekend CUS and mortality. The amount of weekend CUS was calculated as the difference in habitual sleep duration between weekends and weekdays, and classified into no CUS, short (1-h) CUS, and long (2-h or more) CUS, based on previous studies [22, 23]. The two TST and three CUS classifications were combined to generate six TST-CUS classifications, i.e., no CUS with short TST, short CUS with short TST, long CUS with short TST, no CUS with normal TST, short CUS with normal TST, and long CUS with normal TST.
Mortality outcome
Deaths from any cause were identified using multiple concurrent approaches, including follow-up interviews, written annual questionnaires or telephonic conversations with participants or their next-of-kin, surveillance of local hospital records and community obituaries, and linkage with the Social Security Administration Death Master File, as described elsewhere [24].
Other covariates
Baseline sociodemographic and health covariates included age, sex, race/ethnicity (Caucasian and other), smoking status (current, former, and never), body mass index, hypertension (defined as an average systolic blood pressure > 140 mm Hg or average diastolic blood pressure > 90 mm Hg, or the use of antihypertensive medications), diabetes (self-reported or determined by the use of insulin or hypoglycemic medications), stroke, myocardial infarction (identified by a self-reported history of diagnosis by a physician), and an apnea hypopnea index with 4% oxygen desaturation. Additionally, baseline sleep-related covariates included the habitual sleep duration on weekdays in hours, social jetlag, defined as the actual difference between the midpoint of sleep on weekends and that on weekdays, calculated by habitual bedtime and waketime on weekdays and weekdays [25], daytime sleepiness level defined by the Epworth Sleepiness Scale [26], number of naps for five minutes or longer per week, length of sleep during naps taken on the day of assessment in hours and minutes, insomnia or poor sleep as indicated by a self-reported consumption of sleeping pills or difficulty in initiating or maintaining sleep [19], use of antidepressants or benzodiazepines, and rapid eye movement sleep percentage, which has been shown not only to negatively associate with mortality risk in community-based cohorts, including the SHHS [27], but also to be more variable than non-rapid eye-movement sleep stages across in-home PSG nights [28].
Statistical analysis
Of the 3128 individuals analyzed, 590 (18.9%) individuals had at least one missing value in the baseline covariates. A chained equation with 20 imputed datasets was used to replace the missing data, assuming that data were missing randomly [29]. We used Cox proportional hazard models to assess associations between the individuals’ ability to obtain sufficient sleep, amount of weekend CUS, and all-cause mortality using our exposure of interest. We first assessed the individual effect of TST on mortality. Then, we assessed the joint effects of TST and CUS on mortality using the primary and secondary normal cutoffs. The secondary cutoffs were applied while excluding individuals with a PSG-measured TST between 330 and 390 min (n = 1100), leaving 2028 individuals for analysis. Results are shown as hazard ratios with 95% confidence intervals. To test for effect of modification in joint analysis, an interaction term between TST and CUS was entered into each model. All analyses were performed using SPSS Statistics, version 23 (IBM Japan, Tokyo). In addition to unadjusted and age/sex-adjusted models, we ran two multivariable-adjusted models. Model 1 included demographic and health covariates selected based on the known risk factors of mortality, including age, sex, race (Caucasian vs. other), body mass index, smoking status, hypertension, diabetes, apnea hypopnea index with 4% oxygen desaturation, stroke, and myocardial infarction. Model 2 further included sleep-related covariates, including the self-reported habitual sleep duration on weekdays, midsleep point on weekdays, number of daytime naps per week, length of naps, score on the Epworth Sleepiness Scale, use of antidepressants or benzodiazepines, insomnia or poor sleep, and rapid eye movement sleep percentage. Finally, we conducted sensitivity analysis by excluding those dying and censored in the first two years following baseline to exclude other possible explanations for the association of TST and CUS with mortality [30].
Results
Characteristics of participants
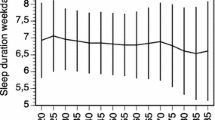
The SHHS cohort included 3,128 middle-aged adults with a mean (standard deviation [SD]) age of 54.5 (6.6) years (40–64 years) at baseline. Participants reported sleeping habitually for 6.98 (1.13) h on weekdays and 7.59 (1.24) h on weekends. The reported habitual bedtime on weekdays and weekends were 22:55 (1:26) and 23:12 (1:32), respectively. The reported habitual waketime on weekdays and weekends were 6:11 (1:31) and 7:06 (1:26), respectively. Over half of the participants (n = 1713, 54.8%) did not habitually extend their sleep on weekends. Of the remaining participants who habitually caught up on their sleep on weekends (n = 1415, 45.2%), two-thirds (n = 946) reported having short (1-h) CUS, while one-third (n = 469) reported having long (2-h +) CUS on weekends. Participants slept for a median (interquartile range [IQR]) of 376.0 (331.0–413.5) minutes on the PSG night. The majority of participants (n = 1881, 60.1%) had an objectively normal sleep duration (TST ≥ 360 min), while the remaining participants (n = 1247, 39.9%) had an objectively short sleep duration (TST < 360 min) (Fig. 1A, B). Table 1 reports demographic, health, and sleep characteristics varying across the TST-CUS classifications. Individuals with short weekend CUS and normal sleep duration tended to have a lower body mass index, apnea hypopnea index, daytime sleepiness, fewer daytime naps, and a higher rate of rapid eye movements during sleep compared to individuals in the other CUS-TST classifications. Figure 1C illustrates the relationships between self-reported habitual sleep durations on weekdays and weekends and PSG-measured TST stratified by the TST-CUS classifications. Self-reported habitual sleep timing (i.e., bedtime, waketime) with calculated midsleep on weekdays and weekends, and self-reported frequency and length of daytime naps, stratified by the TST-CUS classifications, are shown in Supplementary Figs. S1 and S2, respectively.
Habitual weekday and weekend sleep duration, objective sleep duration, and their relationship. A The distribution of weekend catch-up sleep (CUS), as represented by the difference in participants’ habitual sleep duration on weekends and that on weekdays, each self-reported in hours at baseline. B The distribution of participants’ total sleep time (TST) determined by in-home polysomnography at baseline. C The relationships between habitual weekday and weekend sleep duration, and PSG-measured TST stratified by the extent of CUS (no, short, long) and TST (short, normal)
Associations of TST and CUS with survival
A total of 232 deaths (7.4%) were reported over a median (IQR) follow-up time of 12.3 (11.3–13.5) years. The regression analysis of TST showed that compared to normal sleep duration, short sleep duration was consistently associated with higher mortality (fully adjusted HR, 1.45; 95% CI 1.10–1.91; Supplementary Table S1), which was also the case when the secondary cutoffs were applied (fully adjusted HR, 2.01; 95% CI 1.45–2.87; Supplementary Table S1).
We observed a protective effect of short weekend CUS on mortality. The regression analysis of TST-CUS classifications showed that compared to no CUS with normal sleep duration (≥ 360 min), 1-h CUS with normal sleep duration was consistently associated with lower mortality, independently from health and sleep covariates (fully adjusted HR, 0.48; 95% CI 0.27–0.83; Table 2; Fig. 2A, B). When the secondary cutoffs were applied to define short (< 330 min) and normal (≥ 390 min) sleep durations, we observed both an enhanced protective effect of short weekend CUS on mortality and a newly emerged adverse effect of short weekend CUS. The regression analysis of TST-CUS classifications showed that compared to no CUS with normal sleep duration (≥ 390 min), 1-h CUS with normal sleep duration (≥ 390 min) was consistently associated with lower mortality (fully adjusted HR, 0.36; 95% CI 0.17–0.78), whereas 1-h CUS with short sleep duration (< 330 min) was consistently associated with higher mortality (fully adjusted HR, 1.84; 95% CI 1.08–3.14; Table 2)
Multivariable-adjusted Cox regression plots by total sleep time (TST) and weenend catch-up sleep (CUS). Differential cumulative incidences (A) and hazard ratios (HRs) (B) from the fully adjusted Cox proportional hazard model (Model 2) are shown. CI confidence interval, CUS catch-up sleep, Ref reference, TST total sleep time
.
The sensitivity analysis, including those who survived the first two years from baseline, did not show any different results, except for an increased mortality risk of no CUS with short sleep duration (< 330 min) defined by a secondary cutoff (Supplementary Table S2).
Discussion
In this secondary analysis of a community-based, prospective cohort study, we found both beneficial and adverse health effects of weekend CUS that differed depending on the amount of CUS and the ability to obtain sufficient sleep among middle-aged adults. If one slept for a normal duration (≥ 360 min) on the PSG night, a habitual short (1-h) weekend CUS was associated with a lower mortality risk, compared to no weekend CUS. When stricter cutoffs were applied to define short (< 330 min) and normal (≥ 390 min) sleep durations, the harmful effect of short (1-h) weekend CUS newly emerged, whereas the protective effect of short (1-h) weekend CUS was strengthened.
Our findings may help clarify which individuals would benefit more from weekend CUS. The link between weekend CUS and lower mortality was observed only among individuals with objectively normal sleep duration (as either ≥ 360 min or ≥ 390 min). The protective effect of 1-h CUS, as compared to no CUS, if sleep duration is normal, implies that middle-aged adults potentially carry some amount of sleep debt despite their normal ability to obtain sufficient sleep, but a slight amount of weekend CUS could successfully compensate for their sleep debt as far as they maintain that sleep ability. This finding partly aligns with the reported beneficial effects of weekend CUS [22, 23, 31] and newly suggest that only a very small fraction of additional wakefulness is allowed to maintain against biological sleep needs during weekdays so that weekend CUS could efficiently liquidate its cumulative cost.
Notwithstanding, no protective effect was seen for a high amount (2-h or more) of weekend CUS with normal sleep duration. Health and sleep covariates, including social jetlag and daytime napping, did not influence this null finding. The presence of such a high amount of CUS itself may represent the accumulated sleep debt that is not substantially compensated for during weekends, even when their ability to obtain sufficient sleep is not objectively impaired. A high amount of weekend CUS, compared to a low amount, is more likely to put individuals at risk of circadian misalignment, typically due to delayed sleep offset on weekends (work-free days). Given that social jetlag mainly represents actual sleep timing as a measure for circadian misalignment, it could be substantially influenced by sleep loss [25]; this finding suggests that the individual effect of accumulated sleep debt counteracts the protective effects of weekend CUS on mortality, independently from sleep timing effects. Therefore, it is plausible that 2-h + CUS failed to exert a protective effect against mortality, as compared to no CUS. In contrast, the protective effect of short (1-h) weekend CUS with normal sleep duration remained robust after accounting for social jetlag, suggesting the individual effect of the amount of weekend CUS itself on mortality, independent of the circadian drift of sleep phase across the weekday–weekend cycle.
The lack of the protective effect of weekend CUS on mortality among individuals with objectively short sleep duration (as either < 360 min or < 330 min) suggests that when a weekday sleep amount is substantially reduced, the accumulated sleep debt greatly exceeds the homeostatic, restorative potential of CUS for only two weekend nights. Interestingly, when short sleep duration was defined by a second, stricter definition (< 330 min), the harmful effect of weekend CUS remained significant after adjustments among individuals with short (1-h) and not long (2-h +) weekend CUS. Additionally, a sensitivity analysis showed a harmful effect of no weekend CUS, as well as short weekend CUS, with short sleep duration (< 330 min). These findings appear to align with experimental evidence of the harmful effects of sleep debt due to short weekday sleep (e.g., sleep restriction to 4 or 5 h per night for weekdays) on metabolic and endocrine function, which require more than two days to recover [6, 7, 32]. On the other hand, long (2-h +) weekend CUS with an objectively short sleep duration was not associated with an increased mortality risk, as compared to no CUS with objectively normal sleep duration. This finding suggests that a high amount of CUS could help stave off the harmful effects of accumulated sleep debt related to the impaired ability to obtain sufficient sleep. A large-scale longitudinal epidemiological study also suggested that weekend medium or long sleep mitigates the harmful effects related to weekday short sleep on mortality [4]. However, this previous sudy did not differentiate the effects of varying degrees of weekend CUS on mortality among individuals with weekday short sleep. Overcoming this limitation, our present study implies that long, but not short, weekend CUS could mitigate the harmful effects of potential sleep debt among those with weekday short sleep. Moreover, the harmful effect of no weekend CUS with short sleep duration, compared to no CUS with normal sleep duration, was only observed in the sensitivity analysis with a stricter cutoff to dfine short sleep duration (< 330 min). A possible explanation for this is that a certain proportion of individuals with no CUS with objectively short sleep duration were genetically resistant to sleep loss, as represented by short sleepers [33, 34]. In addition, the circadian stability of habitual sleep timing related to no weekend CUS could also alleviate the adverse health effects of short sleep duration [3].
The strengths of our study include its relatively large size, its prospective design, the availability of objective sleep measures, including those that are known to affect mortality (e.g., sleep duration, as well as REM sleep and apnea hypopnea index), and the sensitivity analysis conducted to control for some of the reverse causality. However, this study also has several limitations. A single-night PSG study could underestimate sleep duration due to the first-night effect. However, a study using data from the SHHS, in which some of the SHHS participants underwent two PSG recordings, found no significant differences in sleep duration between the two nights [28]. Therefore, our findings could not be fully explained by the first-night effect. Nonetheless, we cannot be sure that the obtained PSG-measured and self-reported sleep durations are truly representative of their habitual weekday and weekend sleep durations, because these sleep durations were assessed only at baseline, and because exact information was unavailable about whether participants underwent PSG on a workday even though most of them started the PSG on a weekday. In relation to this issue, another limitation is that the interpretation of our results could be speculative as we relied on self-reported data to assess the extent of their habitual weekend CUS. Therefore, our findings need to be confirmed through future studies that associate the objective difference in habitual sleep durations between weekdays and weekends and its changes over time with health outcomes, for instance, using wearable sleep technology. Moreover, while we adjusted for the confounding effects of sleep apnea and insomnia symptoms, other sleep disorders might have influenced our results. However, our findings suggest that individuals who maintain their sleep ability and perceive that their sleep habits need weekend CUS, but its small amount may benefit more from weekend CUS. Furthermore, from a longitudinal perspective, once their ability to obtain sufficient sleep becomes impaired by, for instance, aging or certain pathologies, this small amount of weekend CUS will not function properly and could, in turn, deteriorate health outcomes. An objective assessment of sleep habits may help identify the habit of weekend CUS that requires caution. With the development of wearable sleep technology, more reliable and valid sleep assessment methods will become available nationally. Meanwhile, people’s sleep debt is difficult to solve in modern society. Under such circumstances, our findings will be important in minimizing the negative effects of sleep debt and considering appropriate sleep habits promoting public health.
Conclusions
In a prospective community-based cohort that followed up 3,128 middle-aged adults (40–64 years) for 12 years for mortality outcomes, we addressed the longitudinal association of the habit of weekend CUS and the ability to obtain sufficient sleep with all-cause mortality. We revealed that individuals who reported extending their sleep on weekends by only a short period of time (1 h) had a lower mortality risk, compared to those who reported not extending their sleep on weekends, if they slept for a normal duration (≥ 360 min) on baseline PSG, whereas no protective effect was found among those who slept for a short duration (< 360 min). When objectively short and normal sleep durations were more strictly defined, whereas the protective effect of short weekend CUS on mortality became more obvious among those with objectively normal sleep duration, this short weekend CUS was associated with a higher mortality risk among those with an objectively short sleep duration. There was no increase in the mortality risk among those who reported extending their sleep on weekends by a long period of time (2 h or more), even when they only slept for a short duration on PSG. Our results emphasize the importance of balancing between the extent of CUS required to compensate for sleep debt that accumulates during weekdays and one’s ability to obtain sufficient sleep that could minimize the accumulation of nightly sleep loss among middle-aged adults. Weekend CUS may substantially benefit individuals who maintain their sleep ability and thus require a small amount of CUS. Further studies are needed to confirm these findings and examine underlying mechanisms.
References
Yoshiike T, Utsumi T, Matsui K, Nagao K, Saitoh K, Otsuki R, et al. Mortality associated with nonrestorative short sleep or nonrestorative long time-in-bed in middle-aged and older adults. Sci Rep. 2022;12:189. https://doi.org/10.1038/s41598-021-03997-z.
Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37:9–17. https://academic.oup.com/sleep/article/37/1/9/2454038. Accessed 9 Feb 2023
Chaput J-P, McHill AW, Cox RC, Broussard JL, Dutil C, da Costa BGG, et al. The role of insufficient sleep and circadian misalignment in obesity. Nat Rev Endocrinol. 2022;19:82–97. https://www.nature.com/articles/s41574-022-00747-7. Accessed 9 Feb 2023
Åkerstedt T, Ghilotti F, Grotta A, Zhao H, Adami H, Trolle-Lagerros Y, et al. Sleep duration and mortality—does weekend sleep matter? J Sleep Res. 2019;28:1–11. https://doi.org/10.1111/jsr.12712.
Roenneberg T, Merrow M. The circadian clock and human health. Curr Biol. 2016;26:R432–43. https://doi.org/10.1016/j.cub.2016.04.011.
Depner CM, Melanson EL, Eckel RH, Snell-Bergeon JK, Perreault L, Bergman BC, et al. Ad libitum weekend recovery sleep fails to prevent metabolic dysregulation during a repeating pattern of insufficient sleep and weekend recovery sleep. Curr Biol. 2019;29:957-967.e4. https://doi.org/10.1016/j.cub.2019.01.069.
Kitamura S, Katayose Y, Nakazaki K, Motomura Y, Oba K, Katsunuma R, et al. Estimating individual optimal sleep duration and potential sleep debt. Sci Rep. 2016;6:35812. https://www.nature.com/articles/srep35812. Accessed 9 Feb 2023
Scullin MK. Do older adults need sleep? A review of neuroimaging, sleep, and aging studies. Curr Sleep Med Rep. 2017;3:204–14. https://doi.org/10.1007/s40675-017-0086-z.
Dement WC. Sleep extension: getting as much extra sleep as possible. Clin Sports Med. 2005;24:251–68. https://linkinghub.elsevier.com/retrieve/pii/S0278591904001516. Accessed 9 Feb 2023
Van Dongen HPA, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–26. http://www.ncbi.nlm.nih.gov/pubmed/12683469. Accessed 9 Feb 2023
Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation’s updated sleep duration recommendations: Final report. Sleep Health. 2015;1:233–43. https://doi.org/10.1016/j.sleh.2015.10.004.
Utsumi T, Yoshiike T, Kaneita Y, Aritake-Okada S, Matsui K, Nagao K, et al. The association between subjective–objective discrepancies in sleep duration and mortality in older men. Sci Rep. 2022;12:18650. https://doi.org/10.1038/s41598-022-22065-8.
Quan SF, Howard V, Iber C, Kiley JP, Nieto J, Connor GTO, et al. The sleep heart health study: design, rationale, and methods. Sleep. 1997;20:1077–85. https://academic.oup.com/sleep/article/20/12/1077/2749934/The-Sleep-Heart-Health-Study-Design-Rationale-and. Accessed 9 Feb 2023
Zhang G-Q, Cui L, Mueller R, Tao S, Kim M, Rueschman M, et al. The National Sleep Research Resource: towards a sleep data commons. J Am Med Informatics Assoc. 2018;25:1351–8. https://academic.oup.com/jamia/article/25/10/1351/5026200. Accessed 9 Feb 2023
Sivertsen B, Pallesen S, Friborg O, Nilsen KB, Bakke ØK, Goll JB, et al. Sleep patterns and insomnia in a large population‐based study of middle‐aged and older adults: The Tromsø study 2015–2016. J Sleep Res. 2021;30:1–8. https://onlinelibrary.wiley.com/doi/https://doi.org/10.1111/jsr.13095
Jonasdottir SS, Minor K, Lehmann S. Gender differences in nighttime sleep patterns and variability across the adult lifespan: a global-scale wearables study. Sleep. 2021;44:1–16. https://doi.org/10.1093/sleep/zsaa169/5901589.
Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National sleep foundation’s sleep time duration recommendations: methodology and results summary. Sleep Heal. 2015;1:40–3. https://doi.org/10.1016/j.sleh.2014.12.010.
Redline S, Sanders MH, Lind BK, Quan SF, Iber C, Gottlieb DJ, et al. Methods for obtaining and analyzing unattended polysomnography data for a multicenter study. Sleep. 1998;21:759–67. https://academic.oup.com/sleep/article/21/7/759/2731681. Accessed 9 Feb 2023
Bertisch SM, Pollock BD, Mittleman MA, Buysse DJ, Bazzano LA, Gottlieb DJ, et al. Insomnia with objective short sleep duration and risk of incident cardiovascular disease and all-cause mortality: Sleep Heart Health Study. Sleep. 2018;41:1–9. https://doi.org/10.1093/sleep/zsy047/4924334.
Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–92. https://doi.org/10.1093/sleep/33.5.585.
Fernandez-Mendoza J, He F, Vgontzas AN, Liao D, Bixler EO. Interplay of objective sleep duration and cardiovascular and cerebrovascular diseases on cause-specific mortality. J Am Heart Assoc. 2019. https://doi.org/10.1161/JAHA.119.013043.
Jung SW, Lee K-J, Lee J-H. Does weekend catch-up sleep affect high-sensitivity C-reactive protein levels among korean workers? J Occup Environ Med. 2019;61:e367–73. https://doi.org/10.1097/JOM.0000000000001657.
Im H-J, Baek S-H, Chu MK, Yang KI, Kim W-J, Park S-H, et al. Association between weekend catch-up sleep and lower body mass: population-based study. Sleep. 2017. https://doi.org/10.1093/sleep/zsx089.
Punjabi NM, Caffo BS, Goodwin JL, Gottlieb DJ, Newman AB, O’Connor GT, et al. Sleep-disordered breathing and mortality: a prospective cohort study. Patel A, editor. PLoS Med. 2009;6:e1000132. https://doi.org/10.1371/journal.pmed.1000132.
Roenneberg, Pilz, Zerbini, Winnebeck. Chronotype and social jetlag: a (Self-) critical review. Biology (Basel). 2019;8:54. https://www.mdpi.com/2079-7737/8/3/54. Accessed 9 Feb 2023
Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15:376–81. http://www.ncbi.nlm.nih.gov/pubmed/1519015. Accessed 9 Feb 2023
Zhang J, Jin X, Li R, Gao Y, Li J, Wang G. Influence of rapid eye movement sleep on all-cause mortality: a community-based cohort study. Aging (Albany NY). 2019;11:1580–8. http://www.aging-us.com/article/101858/text. Accessed 9 Feb 2023
Quan SF, Griswold ME, Iber C, Nieto FJ, Rapoport DM, Redline S, et al. Short-term variability of respiration and sleep during unattended nonlaboratory polysomnography–the Sleep Heart Health Study. Sleep. 2002;25:843–9. https://doi.org/10.1093/sleep/25.8.8.
Sterne JAC, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393–b2393. https://doi.org/10.1136/bmj.b2393.
Teno JM, Weitzen S, Fennell ML, Mor V. Dying trajectory in the last year of life: does cancer trajectory fit other diseases? J Palliat Med. 2001;4:457–64. https://doi.org/10.1089/109662101753381593.
Tasali E, Wroblewski K, Kahn E, Kilkus J, Schoeller DA. Effect of sleep extension on objectively assessed energy intake among adults with overweight in real-life settings a randomized clinical trial. JAMA Intern Med. 2022;182:365–70. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2788694. Accessed 9 Feb 2023
Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–9. https://linkinghub.elsevier.com/retrieve/pii/S0140673699013768. Accessed 9 Feb 2023
Ashbrook LH, Krystal AD, Fu Y-H, Ptáček LJ. Genetics of the human circadian clock and sleep homeostat. Neuropsychopharmacology. 2020;45:45–54. http://www.nature.com/articles/s41386-019-0476-7. Accessed 9 Feb 2023
Maire M, Reichert CF, Gabel V, Viola AU, Strobel W, Krebs J, et al. Sleep ability mediates individual differences in the vulnerability to sleep loss: Evidence from a PER3 polymorphism. Cortex. 2014;52:47–59. https://doi.org/10.1016/j.cortex.2013.11.008.
Acknowledgements
The Sleep Heart Health Study (SHHS) was supported by the National Heart, Lung, and Blood Institute cooperative agreements U01HL53916 (University of California, Davis), U01HL53931 (New York University), U01HL53934 (University of Minnesota), U01HL53937 and U01HL64360 (Johns Hopkins University), U01HL53938 (University of Arizona), U01HL53940 (University of Washington), U01HL53941 (Boston University), and U01HL63463 (Case Western Reserve University). The National Sleep Research Resource was supported by the National Heart, Lung, and Blood Institute (R24 HL114473, RFP 75N92019R002).
Funding
This work was supported by the Ministry of Health, Labor and Welfare, Government of Japan (Grant numbers #21FA1002 and #22FA2001).
Author information
Authors and Affiliations
Contributions
KK and TY conceptualized and designed research. TY, KK, AK, TU, and KM analyzed or interpreted data. TY and KK drafted the manuscript. TY, KK, AK, TU, and KM made a critical revision of the manuscript for important intellectual content. KK obtained funding. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no known conflicts of interest to disclose.
Ethical Approval
The current project was approved in April 2020 by the Ethics Committee of the National Center of Neurology and Psychiatry (project number: A2020-012). The study involving human participants was performed in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards, and each participant provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yoshiike, T., Kawamura, A., Utsumi, T. et al. A prospective study of the association of weekend catch-up sleep and sleep duration with mortality in middle-aged adults. Sleep Biol. Rhythms 21, 409–418 (2023). https://doi.org/10.1007/s41105-023-00460-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-023-00460-6