Abstract
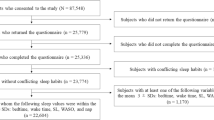
This study aimed to explore the prevalence of sleep disturbances among preschool children in rural areas of China and identify the underlying associated factors. A cross-sectional study was conducted in rural areas of Anhui Province, China, from September 2019 to January 2020. The caregivers of children from 26 kindergartens completed the demographic questionnaire, the Children’s Sleep Habits Questionnaire (CSHQ), the Strengths and Difficulties Questionnaire (SDQ), the Self-rating Anxiety Scale (SAS), and the adapted Identification and Management of Feeding Difficulties (IMFeD) tool. One-way analysis of variance, independent-samples t-test, and hierarchical multiple linear regression were conducted to explore the potential influencing factors of sleep disturbances in preschool children. For the specific sleep disturbances based on each subscale of the CSHQ, bedtime resistance (54.9%) and sleep anxiety (47.9%) were the most common types of sleep disturbances, followed by daytime sleepiness (21.3%), sleep duration (20.8%), parasomnias (16.5%), sleep-onset delay (12.6%), night wakings (12.2%) and sleep-disordered breathing (10.3%). The ages of children, children’s emotional/behavioral problems, children’s feeding difficulties, inconsistent parenting attitudes of parents, poor parenting styles, non-parent caregivers, and caregiver anxiety contributed significantly to the CSHQ total score, accounting for approximately 27.1% (R2 = 0.271) of the variance. Our study indicates that the prevalence of sleep disturbances among preschool children in rural areas of China is quite high. Furthermore, the potential risk factors are complicated, including factors related to both children and their caregivers.
Similar content being viewed by others
Availability of data and material
The raw data required to reproduce these findings cannot be shared at this time as the data also forms part of an ongoing study.
Code availability
N/A.
References
Dubois-Comtois K, Pennestri MH, Bernier A, Cyr C, Godbout R. Family environment and preschoolers’ sleep: the complementary role of both parents. Sleep Med. 2019;58:114–22. https://doi.org/10.1016/j.sleep.2019.03.002.
Gregory AM, O’Connor TG. Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. J Am Acad Child Adolesc Psychiatry. 2002;41(8):964–71. https://doi.org/10.1097/00004583-200208000-00015.
Gregory AM, Sadeh A. Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Med Rev. 2012;16(2):129–36. https://doi.org/10.1016/j.smrv.2011.03.007.
Wang G, Takahashi M, Wu R, Liu Z, Adachi M, Saito M, Nakamura K, Jiang F. Association between sleep disturbances and emotional/behavioral problems in Chinese and Japanese preschoolers. Behav Sleep Med. 2020;18(3):420–31. https://doi.org/10.1080/15402002.2019.1605995.
Mindell JA, Sadeh A, Kwon R, Goh DY. Cross-cultural differences in the sleep of preschool children. Sleep Med. 2013;14(12):1283–9. https://doi.org/10.1016/j.sleep.2013.09.002.
Phillips NL, Moore T, Teng A, Brookes N, Palermo TM, Lah S. Behavioral interventions for sleep disturbances in children with neurological and neurodevelopmental disorders: a systematic review and meta-analysis of randomized controlled trials. Sleep. 2020;43(9):zsaa040. https://doi.org/10.1093/sleep/zsaa040.
Liu X, Liu L, Owens JA, Kaplan DL. Sleep patterns and sleep problems among schoolchildren in the United States and China. Pediatrics. 2005;115:241–9. https://doi.org/10.1542/peds.2004-0815F.
Takahashi M, Wang G, Adachi M, Jiang F, Jiang Y, Saito M, Nakamura K. Differences in sleep problems between Japanese and Chinese preschoolers: a cross-cultural comparison within the Asian region. Sleep Med. 2018;48:42–8. https://doi.org/10.1016/j.sleep.2017.11.1145.
Liu Z, Wang G, Geng L, Luo J, Li N, Owens J. Sleep patterns, sleep disturbances, and associated factors among chinese urban kindergarten children. Behav Sleep Med. 2016;14(1):100–17. https://doi.org/10.1080/15402002.2014.963581.
Wang D. Reduction but not elimination: health inequalities among urban, migrant, and rural children in China-the moderating effect of the fathers’ education level. BMC Public Health. 2019;19(1):1219. https://doi.org/10.1186/s12889-019-7522-6.
Shibata M, Ninomiya T, Anno K, Kawata H, Iwaki R, Sawamoto R, Kubo C, Kiyohara Y, Sudo N, Hosoi M. Perceived inadequate care and excessive overprotection during childhood are associated with greater risk of sleep disturbance in adulthood: the Hisayama Study. BMC Psychiatry. 2016;16:215. https://doi.org/10.1186/s12888-016-0926-2.
Yue A, Bai Y, Shi Y, Luo R, Rozelle S, Medina A, Sylvia S. Parental migration and early childhood development in rural China. Demography. 2020;57(2):403–22. https://doi.org/10.1007/s13524-019-00849-4.
Owens JA. Introduction: culture and sleep in children. Pediatrics. 2005;115:201–3. https://doi.org/10.1542/peds.2004-0815a.
Tambalis KD, Panagiotakos DB, Psarra G, Sidossis LS. Insufficient sleep duration is associated with dietary habits, screen time, and obesity in children. J Clin Sleep Med. 2018;14(10):1689–96. https://doi.org/10.5664/jcsm.7374.
Garfield V. The association between body mass index (BMI) and sleep duration: where are we after nearly two decades of epidemiological research? Int J Environ Res Public Health. 2019;16(22):4327. https://doi.org/10.3390/ijerph16224327.
He L, Li X, Wang W, Wang Y, Qu H, Zhao Y, Lin D. Clustering of multiple lifestyle behaviors among migrant, left-behind and local adolescents in China: a cross-sectional study. BMC Public Health. 2021;21(1):542. https://doi.org/10.1186/s12889-021-10584-4.
Fellmeth G, Rose-Clarke K, Zhao C, Busert LK, Zheng Y, Massazza A, Sonmez H, Eder B, Blewitt A, Lertgrai W, Orcutt M, Ricci K, Mohamed-Ahmed O, Burns R, Knipe D, Hargreaves S, Hesketh T, Opondo C, Devakumar D. Health impacts of parental migration on left-behind children and adolescents: a systematic review and meta-analysis. Lancet (London, England). 2018;392(10164):2567–82. https://doi.org/10.1016/S0140-6736(18)32558-3.
Schultz LF, Kroll C, Constantino B, Trombelli M, El Rafihi-Ferreira R, Mastroeni MF. Association of maternal depression and anxiety symptoms with sleep duration in children at preschool age. Matern Child Health J. 2020;24(1):62–72. https://doi.org/10.1007/s10995-019-02843-z.
Ding P, Geng ML, Wu XY, Li SY, Tao SM, Wang L, Chen J, Peng L, Wang SM, Yin GZ, Zhang AH, Deng H, Tang YX, Ma YQ, Huang HP, Xiang M, Tao FB. Sleep quality in preschool children in three provinces along the middle and lower reaches of the Yangtze River. Chin J Sch Health. 2019;40(8):1173–6.
Wu R, Wang GH, Zhu H, Jiang F, Jiang CL. Sleep patterns in chinese preschool children: a population-based study. J Clin Sleep Med. 2018;14(4):533–40. https://doi.org/10.5664/jcsm.7038.
Wu X, Tao S, Rutayisire E, Chen Y, Huang K, Tao F. The relationship between screen time, nighttime sleep duration, and behavioural problems in preschool children in China. Eur Child Adolesc Psychiatry. 2017;26(5):541–8. https://doi.org/10.1007/s00787-016-0912-8.
Organization WH. WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. World Health Organization. 2006.
American Academy of Pediatrics. Children, adolescents, and television. Pediatrics. 2001;107(2):423–6. https://doi.org/10.1542/peds.107.2.423.
Council on Communications and Media. Media and Young Minds. Pediatrics. 2016;138(5):e20162591. https://doi.org/10.1542/peds.2016-2591
Owens JA, Spirito A, McGuinn M, Nobile C. Sleep habits and sleep disturbance in elementary school-aged children. J Dev Behav Pediatr. 2000;21(1):27–36. https://doi.org/10.1097/00004703-200002000-00005.
Perpétuo C, Fernandes M, Veríssimo M. Comparison between actigraphy records and parental reports of child’s sleep. Front Pediatr. 2020;8: 567390. https://doi.org/10.3389/fped.2020.567390.
Liu Z, Wang G, Tang H, Wen F, Li N. Reliability and validity of the Children’s Sleep Habits Questionnaire in preschool-aged Chinese children. Sleep Biol Rhythms. 2014;12(3):187–93. https://doi.org/10.1111/sbr.12061.
Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23(8):1043–51.
Wang G, Xu G, Liu Z, Lu N, Ma R, Zhang E. Sleep patterns and sleep disturbances among Chinese school-aged children: prevalence and associated factors. Sleep Med. 2013;14(1):45–52. https://doi.org/10.1016/j.sleep.2012.09.022.
Wang G, Liu Z, Xu G, Jiang F, Lu N, Baylor A, Owens J. Sleep disturbances and associated factors in chinese children with autism spectrum disorder: a retrospective and cross-sectional study. Child Psychiatry Hum Dev. 2016;47(2):248–58. https://doi.org/10.1007/s10578-015-0561-z.
Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry. 1997;38(5):581–6. https://doi.org/10.1111/j.1469-7610.1997.tb01545.x.
Guedeney A, Pingault JB, Thorr A, Larroque B, EDEN Mother-Child Cohort Study Group. Social withdrawal at 1 year is associated with emotional and behavioural problems at 3 and 5 years: the Eden mother-child cohort study. European child & adolescent psychiatry. 2014;23(12):1181–1188. doi: https://doi.org/10.1007/s00787-013-0513-8
Kou JH, Du YS, Xia LM. Reliability and validity of “children Strengths and Difficulties Questionnaire” in Shanghai norm. Shanghai Arch Psychiatry. 2005;17(1):25–8.
Dunstan DA, Scott N. Norms for Zung’s self-rating anxiety scale. BMC Psychiatry. 2020;20(1):90. https://doi.org/10.1186/s12888-019-2427-6.
Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–9. https://doi.org/10.1016/s0033-3182(71)71479-0.
Liu X, Chen M, Wang Y, Sun L, Zhang J, Shi Y, Wang J, Zhang H, Sun G, Baker PN, Luo X, Qi H. Prenatal anxiety and obstetric decisions among pregnant women in Wuhan and Chongqing during the COVID-19 outbreak: a cross-sectional study. BJOG. 2020. https://doi.org/10.1111/1471-0528.16381.
Ma X, Wang Y, Hu H, Tao XG, Zhang Y, Shi H. The impact of resilience on prenatal anxiety and depression among pregnant women in Shanghai. J Affect Disord. 2019;250:57–64. https://doi.org/10.1016/j.jad.2019.02.058.
Deng C, Zhang W, Jin Y, Feng HJ, He XL, Liu QJ, Liu YL, Liao Y. Analysis of relationship between eating problems of 1–5 years old children and the feeding behavior. Chin J Child Health Care. 2012;20(8):686–8.
Qu G, Wang L, Tang X, Wu W, Zhang J, Sun Y. Association between caregivers’ anxiety and depression symptoms and feeding difficulties of preschool children: A cross-sectional study in rural China. Arch Pediatr. 2020;27(1):12–7. https://doi.org/10.1016/j.arcped.2019.11.007.
Lin CC, Ni YH, Lin LH, Lau BH, Chao HC, Lee HC. Effectiveness of the IMFeD tool for the identification and management of feeding difficulties in Taiwanese children. Pediatr Neonatol. 2018;59(5):507–14. https://doi.org/10.1016/j.pedneo.2018.01.001.
Garg P, Williams JA, Satyavrat V. A pilot study to assess the utility and perceived effectiveness of a tool for diagnosing feeding difficulties in children. Asia Pac Fam Med. 2015;14(1):7. https://doi.org/10.1186/s12930-015-0024-5.
Li W, Wang G, Yu Z, Ip P, Leng Y, Zhang Y, Zhao J, Zhang J, Jiang Y, Deng Y, Wu Y, Meng M, Zhu Q, Jiang F. Grandparental care and sleep disturbances in preschool children: a population-based prospective cohort study. Sleep Med. 2021;82:165–71. https://doi.org/10.1016/j.sleep.2021.03.033.
Yang CK, Hahn HM. Cosleeping in young Korean children. J Dev Behav Pediatr. 2002;23(3):151–7. https://doi.org/10.1097/00004703-200206000-00004.
Guo MY, Xie CB, Zhao XL, Liao Y, Gu LP, Gao JH, Li XH, Wen XZ. Study on the association between sleep arrangements and sleep quality in preschool children. Chin J Child Health Care. 2019;27(1):37–41.
Wang PY, Li W, Hu YB, Wang GH, Jiang F, Chen J. Investigation on sleep problems and related factors in preschool children during home quarantine. Chin J Child Health Care. 2021;29(5):479–83.
Lemola S, Schwarz B, Siffert A. Interparental conflict and early adolescents’ aggression: is irregular sleep a vulnerability factor? J Adolesc. 2012;35(1):97–105. https://doi.org/10.1016/j.adolescence.2011.06.001.
Kljajic Z, Roje Z, Becic K, Capkun V. Obstructive sleep apnea in children: How it affects parental psychological status? Int J Pediatr Otorhinolaryngol. 2019;117:157–62. https://doi.org/10.1016/j.ijporl.2018.11.032.
Cadart M, De Sanctis L, Khirani S, Amaddeo A, Ouss L, Fauroux B. Parents of children referred to a sleep laboratory for disordered breathing reported anxiety, daytime sleepiness and poor sleep quality. Acta Paediatr. 2018;107(7):1253–61. https://doi.org/10.1111/apa.14353.
O’Connor TG, Caprariello P, Blackmore ER, Gregory AM, Glover V, Fleming P. Prenatal mood disturbance predicts sleep problems in infancy and toddlerhood. Early Hum Dev. 2007;83(7):451–8. https://doi.org/10.1016/j.earlhumdev.2006.08.006.
Goldberg WA, Lucas-Thompson RG, Germo GR, Keller MA, Davis EP, Sandman CA. Eye of the beholder? Maternal mental health and the quality of infant sleep. Soc Sci Med. 2013;79:101–8. https://doi.org/10.1016/j.socscimed.2012.07.006.
Xiao L, Zhang S, Li W, Wu R, Wang W, Wang T, Guo L, Lu C. The mediating effect of sleep quality on the relationship between emotional and behavioral problems and suicidal ideation. Int J Environ Res Public Health. 2019;16(24):4963. https://doi.org/10.3390/ijerph16244963.
Yoo SS, Gujar N, Hu P, Jolesz FA, Walker MP. The human emotional brain without sleep–a prefrontal amygdala disconnect. Curr Biol. 2007;17(20):R877–8. https://doi.org/10.1016/j.cub.2007.08.007.
Benca RM, Obermeyer WH, Thisted RA, Gillin JC. Sleep and psychiatric disorders. A meta-analysis Arch Gen Psychiatry. 1992;49(8):651–68. https://doi.org/10.1001/archpsyc.1992.01820080059010.
Richdale AL, Schreck KA. Sleep problems in autism spectrum disorders: prevalence, nature, & possible biopsychosocial aetiologies. Sleep Med Rev. 2009;13(6):403–11. https://doi.org/10.1016/j.smrv.2009.02.003.
Malow BA, Marzec ML, McGrew SG, Wang L, Henderson LM, Stone WL. Characterizing sleep in children with autism spectrum disorders: a multidimensional approach. Sleep. 2006;29(12):1563–71. https://doi.org/10.1093/sleep/29.12.1563.
Khan MKA, Faught EL, Chu YL, Ekwaru JP, Storey KE, Veugelers PJ. Is it nutrients, food items, diet quality or eating behaviours that are responsible for the association of children’s diet with sleep? J Sleep Res. 2017;26(4):468–76. https://doi.org/10.1111/jsr.12466.
Dahl RE, Lewin DS. Pathways to adolescent health: sleep regulation and behavior. J Adoles Health. 2002;31:175–84. https://doi.org/10.1016/s1054-139x(02)00506-2.
Eisenberg ME, Olson RE, Neumark-Sztainer D, Story M, Bearinger LH. Correlations between family meals and psychosocial well-being among adolescents. Arch Pediat Adoles Med. 2004;158(8):792–6. https://doi.org/10.1001/archpedi.158.8.792.
Tauman R, Levine A, Avni H, Nehama H, Greenfeld M, Sivan Y. Coexistence of sleep and feeding disturbances in young children. Pediatrics. 2011;127(3):e615–21. https://doi.org/10.1542/peds.2010-2309.
Metbulut AP, Özmert EN, Teksam O, Yurdakök K. A comparison between the feeding practices of parents and grandparents. Eur J Pediatr. 2018;177(12):1785–94. https://doi.org/10.1007/s00431-018-3244-5.
Li M, Xue H, Wang W, Wang Y. Parental Expectations and Child Screen and Academic Sedentary Behaviors in China. Am J Prev Med. 2017;52(5):680–9. https://doi.org/10.1016/j.amepre.2016.12.006.
Acknowledgements
We appreciate the authors listed in this paper for their contributions to this study, including study design, site investigation, data collation and analysis, and paper writing; in addition, we also appreciate Dr. Sun Liang, Dr. Qin Qirong and their colleagues in the local Center for Disease Control and Prevention and all kindergartens for their great cooperation.
Funding
This work was supported by the National Natural Science Foundation of China (Grant number: 81872704).
Author information
Authors and Affiliations
Contributions
Dr. YS: designed the study and made the final revision; TZ, KX, HL, XC, and GQ: collected the data; TZ and KX: wrote the manuscript; HL and XC: helped in manuscript writing; YW and JZ: critically reviewed the manuscript and helped in revising the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by Ethics Committee of Anhui Medical University (20180402) and followed the principles of informed consent and strict confidentiality.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Written informed consent for publication was obtained from all the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhao, T., Xuan, K., Liu, H. et al. Sleep disturbances and correlates among a sample of preschool children in rural China. Sleep Biol. Rhythms 20, 123–136 (2022). https://doi.org/10.1007/s41105-021-00348-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-021-00348-3



