Abstract
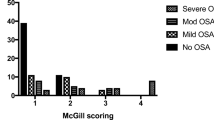
The purposes of this study were: (1) to confirm the prevalence of sleep-disordered breathing (SDB) in Japanese children using nocturnal pulse oximetry (NPOx) as a screening tool and (2) to examine what kind of parameters are suitable for the evaluation of SDB in children. We conducted a study of 99 children between 4 and 15-year-old and obtained their demographic characteristics and the presence of SDB-related symptoms by questionnaire from their parents. In our study, 36% had been Down syndrome (DS), 25% had cardiovascular disease and 34% had dental/oral abnormality. As SDB-related symptoms, snoring (35%), awake disturbance (48%), arousal (41%) and nocturia (19%) were reported. We analyzed each parameter based on the previous reported data of children and temporary defined normal range as follows; 3%ODI < 2.04, 4%ODI < 0.78, SpO2 nadir > 89% and McGill oximetry score = 1. In non-DS group, each parameter showed abnormal value especially in younger group (abnormality; 61–94%), but the abnormality was decreased during the growth (abnormality; 11–63%). Interestingly, in DS group the value of each parameter was kept on abnormal during the growth (abnormality; 55–100%). We investigated the correlation between McGill oximetry score and ODI or SpO2 nadir. There was a significant positive correlation between McGill oximetry score and 3% or 4% ODI. Moreover, there was a significant negative correlation between McGill oximetry score and SpO2 nadir. Based on NPOx screening, prevalence of SDB was high; however, it was decreased during the growth in non-DS group. Each parameter might be useful for SDB screening in children.



Similar content being viewed by others
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5.
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177:1006–14.
McNicholas WT, Bonsigore MR, Management Committee of EU COST ACTION B26. Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. Eur Respir J. 2007;29:156–78.
Strohl KP, Brown DB, Collop N, George C, Grunstein R, Han F, Kline L, Malhotra A, Pack A, Phillips B, Rodenstein D, Schwab R, Weaver T, Wilson K, ATS Ad Hoc Committee on Sleep Apnea, Sleepiness, and Driving Risk in Noncommerical Drivers. An official American Thoracic Society clinical practice guideline: sleep apnea, sleepiness, and driving risk in noncommercial drivers. An update of a 1994 statement. Am J Respir Crit Care Med. 1994;2013(187):1259–66.
Guilleminault C, Lee JH, Chan A. Pediatric obstructive sleep apnea syndrome. Arch Pediatr Adolesc Med. 2005;159:775–85.
Mitchell RB, Kelly J. Behavior, neurocognition and quality-of-life in children with sleep-disordered breathing. Int J Pediatr Otorhinolaryngol. 2006;70:395–406.
Papaioannou G, Kambas I, Tsaoussoglou M, Panaghiotopoulou-Gartagani P, Chrousos G, Kaditis AG. Age-dependent changes in the size of adenotonsiller tissue in childhood: implications for sleep-disordered breathing. J Pediatr. 2013;162:269–74.
Li HY, Huang YS, Chen NH, Fang TJ, Lee LA. Impact of adenotonsillectomy on behavior in children with sleep-disordered breathing. Laryngoscope. 2006;116:1142–7.
Kitamura T, Miyazaki S, Kadotani H, Suzuki H, Kanemura T, Kodama I, Nishikawa M, Kobayashi R, Okawa M. Prevalence of obstructive sleep apnea syndrome in Japanese elementary school children aged 6–8 years. Sleep Breath. 2014;18:359–66.
Kobayashi R, Miyazaki S, Karaki M, Hoshikawa H, Nakata S, Hara H, Kikuchi A, Kitamura T, Mori N. Obstructive sleep apnea in Asian primary school children. Sleep Breath. 2014;18:483–9.
Tahara S, Hara H, Yamashita H. Evaluation of body growth in prepubertal Japanese children with obstructive sleep apnea after adenotonsillectomy over a long postoperative period. Int J Pediatr Otorhinolaryngol. 2015;79:1806–9.
Ono J, Chishaki A, Ohkusa T, Sawatari H, Nishizaka M, Ando S. Obstructive sleep apnea-related symptoms in Japanese people with Down syndrome. Nurs Health Sci. 2015;17:420–5.
Kuroda H, Sawatari H, Ando S, Ohkusa T, Rahmawati A, Ono J, Nishizaka M, Hashiguchi N, Matsuoka F, Chishaki A. A nationwide, cross-sectional survey on unusual sleep postures and sleep-disordered breathing-related symptoms in people with Down syndrome. J Intellect Disabil Res. 2017;61:656–67.
Nixon GM, Kermack AS, Davis GM, Manoukian JJ, Brown KA, Brouillette T. Planning adenotonsillectomy in children with obstructive sleep apnea: the role of overnight oximetry. Pediatrics. 2004;113:e19–25.
Brouillette RT, Morielli A, Lemianis A, Waters KA, Luciano R, Ducharme FM. Nocturnal pulse oximetry as an abbreviated testing modality for pediatric obstructive sleep aonea. Pediatrics. 2000;105:405–12.
Saito H, Araki K, Ozawa H, Mizutari K, Inagaki K, Habu N, Yamashita T, Fujii R, Miyazaki S, Ogawa K. Pulse-oximetery is useful in determining the indications for adeno-tonsillectomy in pediatric sleep-disordered breathing. Int J Pediatr Otorhinolaryngol. 2007;71:1–6.
Lumeng JC, Chervin RD. Epidemiology of pediatric obstructive sleep apnea. Proc Am Thorac Soc. 2008;5:242–52.
Bixler EO, Vgontzas AN, Lin HM, Liao D, Calhoun S, Vela-Bueno A, Fedok F, Vlasic V, Graff G. Sleep disordered breathing in children in a general population sample: prevalence and risk factors. Sleep. 2009;32:731–6.
Li AM, So HK, Au CT, Ho C, Lau J, Ng SK, Abdullah VJ, Fok TF, Wing YK. Epidemiology of obstructive sleep apnoea syndrome in Chinese children: a two-phase community study. Thorax. 2010;65:991–7.
American Academy of Sleep Medicine. International classification of sleep disorders. Diagnostic and coding manual. 2nd ed. Westchester: American Academy of Sleep Medicine; 2005.
Kaditis A, Kheirandis-Gozal L, Gozal D. Pediatric OSAS: oximetry can provide answers when polysomnography is not available. Sleep Med Rev. 2016;27:96–105.
Goodwin JL, Vasquez MM, Silva GE, Quan SF. Incidence and remission of sleep-disordered breathing and related symptoms in 6- to 17-year old children—The Tucson Children’s Assessment of Sleep Apnea Study. J Pediatr. 2010;157:57–61.
Scholle S, Wiater A, Scholle HC. Normative values of polysomnographic parameters in childhood and adolescence: cardiorespiratory parameters. Sleep Med. 2011;12:988–96.
Bonuck KA, Freeman K, Henderson J. Growth and growth biomaler changes after adenotonsillectomy: systematic review and meta-analysis. Arch Dis Child. 2009;94:83–91.
Kohler MJ, Lushington K, van den Heuvel CJ, Martin J, Pamula Y, Kennedy D. Adenotonsillectomy and neurocognitive deficits in children with sleep disordered breathing. PLoS One. 2009;4:e7343.
Maris M, Verhulst S, Wojciechowski M, Van de Heyning P, Boudewyns A. Prevalence of obstructive sleep apnea in children with Down syndrome. Sleep. 2016;39:699–704.
Bull MJ, the Committee on Genetics. Clinical report—Health supervision for children with Down syndrome. Pediatrics. 2011;128:393–406.
Nakano H, Furukawa T, Hayashi M, Ohshima E, Nishikata N, Nagai Y, Sato M. A new oximetry algorithm for screening of sleep-disordered breathing. Ther Res. 2005;26:931–7 (in Japanese with English Abstract).
Acknowledgements
The authors thank Ms. Yukiko Yamamoto, Oshima nursing school for technical support and the school staff, children, and their parents for their cooperation and participation. This research was supported by a Grant from Fukuda Foundation for Medical Technology.
Funding
This study was funded by Fukuda Foundation for Medical Technology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Tomoko Nao declares that I have no conflict of interest. Anita Rahmawati declares that she has no conflict of interest. Mari Nishizaka declares that she has no conflict of interest. Hiroyuki Sawatari declares that he has no conflict of interest. Nobuko Moriyama declares that she has no conflict of interest. Akiko Chishaki declares that she has no conflict of interest. Shin-Ichi Ando declares that he has no conflict of interest. Tomoko Ohkusa declares that she has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical committee permission
All procedures were in accordance with the Ethical Committee of Ube Frontier University (approved no. 15004).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nao, T., Rahmawati, A., Nishizaka, M. et al. Prevalence of sleep-disordered breathing in Japanese children: efficiency of screening with nocturnal pulse oximetry. Sleep Biol. Rhythms 18, 37–47 (2020). https://doi.org/10.1007/s41105-019-00242-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-019-00242-z