Abstract
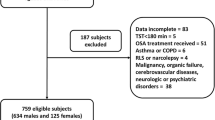
In our previous study, we observed younger OSAS patients had higher CPAP acceptance but similar compliance as older OSAS patients, suggesting gender factor might play an important role on CPAP acceptance. Hence, we aimed to evaluate the influences of both gender and age on CPAP acceptance and compliance in Taiwanese OSAS patients. This retrospective study included 371 subjects which were subdivided by gender and age (younger: age < 55 years, and older: age ≥ 55 years) (n = 24 for younger women, n = 67 for older women, n = 131 for younger men; and n = 149 for older men). Anthropometric parameters, blood pressures, Epworth sleepiness scale, polysomnography variables, CPAP acceptance, and CPAP compliance were collected and compared. Univariate analysis evaluated the influence of different variables on CPAP acceptance. Due to the presence of multicollinearity for N3 sleep and AHI, as well as N3 sleep and DI, multivariate logistic regression models were conducted using three different models with N3 sleep, AHI, and DI included separately. Univariate analysis found women had less CPAP acceptance than men. Multivariate logistic regression analysis indicated younger women had lower CPAP acceptance, but in contrast younger men had higher CPAP acceptance. No difference was observed among the four subgroups for long-term CPAP compliance. In conclusion, our findings suggest that both age and gender impact CPAP acceptance for treating OSAS in Taiwan, with women having lower CPAP acceptance than men regardless of age. No apparent influence of age and gender on CPAP compliance was observed.

Similar content being viewed by others
Abbreviations
- AHI:
-
Apnea/hypopnea index
- CAD:
-
Coronary artery disease
- CPAP:
-
Continuous positive airway pressure
- CVD:
-
Cardiovascular disease
- CVA:
-
Cerebrovascular accident
- DBP:
-
Diastolic blood pressure
- DI:
-
Desaturation index
- EDS:
-
Excessive daytime sleepiness
- EEG:
-
Electroencephalography
- ESS:
-
Epworth sleepiness scale
- HTN:
-
Hypertension
- MAP:
-
Mean arterial pressure
- OSAS:
-
Obstructive sleep apnea syndrome
- PSG:
-
Polysomnography
- REM:
-
Rapid eye movement
- SaO2:
-
Oxygen saturation
- SBP:
-
Systolic blood pressure
References
Henderson LA, Macefield VG. Obstructive sleep apnoea and hypertension: the role of the central nervous system. Curr Hypertens Rep. 2016;18:59.
Lin SW, Chou YT, Kao KC, Chuang LP, Yang CM, Hu HC, et al. Immediate and long-term neurocognitive outcome in patients with obstructive sleep apnea syndrome after continuous positive airway pressure treatment. Indian J Otolaryngol Head Neck Surg. 2015;67:79–85.
Ramos AR, Tarraf W, Rundek T, Redline S, Wohlgemuth WK, Loredo JS, et al. Obstructive sleep apnea and neurocognitive function in a Hispanic/Latino population. Neurology. 2015;84:391–8.
O’Connor C, Thornley KS, Hanly PJ. Gender differences in the polysomnographic features of obstructive sleep apnea. Am J Respir Crit Care Med. 2000;161:1465–72.
Resta O, Caratozzolo G, Pannacciulli N, Stefano A, Giliberti T, Carpagnano GE, et al. Gender, age and menopause effects on the prevalence and the characteristics of obstructive sleep apnea in obesity. Eur J Clin Invest. 2003;33:1084–9.
Li Z, Li Y, Yang L, Li T, Lei F, Vgontzas AN, et al. Characterization of obstructive sleep apnea in patients with insomnia across gender and age. Sleep Breath. 2015;19:723–7.
Gupta MA, Simpson FC, Lyons DC. The effect of treating obstructive sleep apnea with positive airway pressure on depression and other subjective symptoms: a systematic review and meta-analysis. Sleep Med Rev. 2016;28:55–68.
Neikrug AB, Liu L, Avanzino JA, Maglione JE, Natarajan L, Bradley L, et al. Continuous positive airway pressure improves sleep and daytime sleepiness in patients with Parkinson disease and sleep apnea. Sleep. 2014; 37:177–85.
Barbe F, Duran-Cantolla J, Sanchez-de-la-Torre M, Martinez-Alonso M, Carmona C, Barcelo A, et al. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: a randomized controlled trial. JAMA. 2012;307:2161–8.
Diamanti C, Manali E, Ginieri-Coccossis M, Vougas K, Cholidou K, Markozannes E, et al. Depression, physical activity, energy consumption, and quality of life in OSA patients before and after CPAP treatment. Sleep Breath. 2013;17:1159–68.
Salepci B, Caglayan B, Kiral N, Parmaksiz ET, Comert SS, Sarac G, et al. CPAP adherence of patients with obstructive sleep apnea. Respir Care. 2013;58:1467–73.
Schwab RJ, Badr SM, Epstein LJ, Gay PC, Gozal D, Kohler M, et al. An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med. 2013; 188: 613 – 20.
Simon-Tuval T, Reuveni H, Greenberg-Dotan S, Oksenberg A, Tal A, Tarasiuk A. Low socioeconomic status is a risk factor for CPAP acceptance among adult OSAS patients requiring treatment. Sleep. 2009; 32: 545 – 52.
Reuveni H, Tarasiuk A, Wainstock T, Ziv A, Elhayany A, Tal A. Awareness level of obstructive sleep apnea syndrome during routine unstructured interviews of a standardized patient by primary care physicians. Sleep. 2004;27:1518–25.
Hoy CJ, Vennelle M, Kingshott RN, Engleman HM, Douglas NJ. Can intensive support improve continuous positive airway pressure use in patients with the sleep apnea/hypopnea syndrome?. Am J Respir Crit Care Med. 1999; 159: 1096–100.
Shahrabani S, Tzischinsky O, Givati G, Dagan Y. Factors affecting the intention and decision to be treated for obstructive sleep apnea disorder. Sleep Breath. 2014; 18: 857–68.
Tzischinsky O, Shahrabani S, Peled R. Factors affecting the decision to be treated with continuous positive airway pressure for obstructive sleep apnea syndrome. Isr Med Assoc J. 2011;13:413–9.
Tarasiuk A, Reznor G, Greenberg-Dotan S, Reuveni H. Financial incentive increases CPAP acceptance in patients from low socioeconomic background. PLoS One. 2012;7:e33178.
Greenberg-Dotan S, Reuveni H, Simon-Tuval T, Oksenberg A, Tarasiuk A. Gender differences in morbidity and health care utilization among adult obstructive sleep apnea patients. Sleep. 2007;30:1173–80.
Morrish E, Shneerson JM, Smith IE. Why does gender influence survival in obstructive sleep apnoea? Respir Med. 2008;102:1231–6.
Ye L, Pien GW, Ratcliffe SJ, Weaver TE. Gender differences in obstructive sleep apnea and treatment response to continuous positive airway pressure. J Clin Sleep Med. 2009;5:512–8.
Woehrle H, Graml A, Weinreich G. Age- and gender-dependent adherence with continuous positive airway pressure therapy. Sleep Med. 2011;12:1034–6.
Yang MC, Lin CY, Lan CC, Huang CY, Huang YC, Lim CS, et al. Factors affecting CPAP acceptance in elderly patients with obstructive sleep apnea in Taiwan. Respir Care. 2013;58:1504–13.
Pelletier-Fleury N, Rakotonanahary D, Fleury B. The age and other factors in the evaluation of compliance with nasal continuous positive airway pressure for obstructive sleep apnea syndrome. A Cox’s proportional hazard analysis. Sleep Med. 2001; 2:225–32.
Alotair HA, Bahammam AS. Continuous positive airway pressure compliance in Saudi men and women with sleep apnea. Saudi Med J. 2008;29:1064–5.
Jordan AS, McEvoy RD. Gender differences in sleep apnea: epidemiology, clinical presentation and pathogenic mechanisms. Sleep Med Rev. 2003; 7: 377–89.
Chen NH, Johns MW, Li HY, Chu CC, Liang SC, Shu YH, et al. Validation of a Chinese version of the Epworth sleepiness scale. Qual Life Res. 2002; 11: 817–21.
Rechtschaffen A KA. A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Bethesda, MD: National Institutes of Health; 1968.
Anstead M, Phillips B, Buch K. Tolerance and intolerance to continuous positive airway pressure. Curr Opin Pulm Med. 1998;4:351–4.
Grunstein RR. Sleep-related breathing disorders. 5. Nasal continuous positive airway pressure treatment for obstructive sleep apnoea. Thorax. 1995;50:1106–13.
Gay P, Weaver T, Loube D, Iber C, Positive Airway Pressure Task F. Standards of Practice C. et al. Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep. 2006;29:381–401.
Shapiro GK, Shapiro CM. Factors that influence CPAP adherence: an overview. Sleep Breath. 2010; 14: 323–35.
Engleman HM, Wild MR. Improving CPAP use by patients with the sleep apnoea/hypopnoea syndrome (SAHS). Sleep Med Rev. 2003;7:81–99.
Faulx MD, Larkin EK, Hoit BD, Aylor JE, Wright AT, Redline S. Sex influences endothelial function in sleep-disordered breathing. Sleep. 2004;27:1113–20.
Young T, Finn L. Epidemiological insights into the public health burden of sleep disordered breathing: sex differences in survival among sleep clinic patients. Thorax. 1998;53(Suppl 3):S16–9.
Quintana-Gallego E, Carmona-Bernal C, Capote F, Sanchez-Armengol A, Botebol-Benhamou G, Polo-Padillo J, et al. Gender differences in obstructive sleep apnea syndrome: a clinical study of 1166 patients. Respir Med. 2004;98:984–9.
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author contributions
Literature search: CCL and WLS; data collection: YCH and MCY; study design: MCY and YKW; analysis of data: MCY; manuscript preparation: YCH and MCY; review of manuscript: YKW and MCY. All authors read and approved the study.
Funding
The study was supported by a grant from the Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation (TCRD-TPE-106-RT-1).
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
The study was performed in accordance with the Declaration of Helsinki. The Institutional Review Board of the Taipei Tzuchi Hospital approved the protocol.
Informed consent
Since the study was retrospective in design, informed consent was not necessary.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Huang, YC., Lan, CC., Wu, YK. et al. Age- and gender-related differences of CPAP acceptance for obstructive sleep apnea syndrome in Taiwan. Sleep Biol. Rhythms 16, 107–115 (2018). https://doi.org/10.1007/s41105-017-0132-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-017-0132-8