Abstract
Purpose
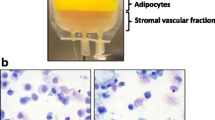
Aspirates from the liposuction procedures have been identified as a potential source of cells, termed the stromal vascular fraction (SVF) that could be utilized for regenerative engineering purposes owing to their multipotent capability. They stimulate regenerative effect through the secretion of biologically active molecules that act in a paracrine fashion to enhance angiogenic, anti-fibrotic, anti-apoptotic, and immuno-modulation responses at targeted tissue. As the prospects in SVF continue to drive interest among scientists, there have been corresponding innovations added, many of which have been patented or are currently in the process. This review aims at exploring the relevant additions to our previous knowledge of SVF.
Method
Patent on stromal vascular fraction, patent on adipose tissue, or adipose tissue products were searched on PubMed, PMC, Google Scholar, https://patents.justia.com/patent/, and http://www.patentsencyclopedia.com/app/ from 2005 to 2020. Withdrawn, abandoned, or inactive applications were excluded.
Result
There were many innovations in isolation methods, isolation kits, characterization molecules, purification, pharmacological mechanisms, and implant/graft/therapeutic applications of SVF. These were highlighted under subcategories and the scope of inventions including methods of cell isolation and processing; methods and devices for the application of SVF; and therapeutic application of SVF for diseased conditions. Each subcategory was further summarized by detailing its inventors, patent number, the field of invention, description, and major claims.
Conclusion
The recent patented innovations from basic and clinical studies indicate that SVF has the prospect of providing a better quality of life to patients. Though the FDA is yet to approve the clinical use of SVF, more studies are ongoing to standardize the processes involved and also provide more evidence to support the safety.
Lay Summary
The aspirates from liposuction contain a fraction that holds in native cells, termed the stromal vascular SVF. Due to the regenerative potentials of SVF, there has been an increased research interest, with corresponding discoveries. These include the methods of isolation, isolation kits, characterization and purification makers, mechanism of action, applications, and therapies. In this report, a summary of some of the active and recently applied patents on SVF was detailed. These native cells are made up of a mixture of populations, which has the potential for application in regenerative engineering. They can be obtained through mechanical or enzymatic means and produce their regeneration effect mainly by the secretion of bioactive molecules that can modulate immune responses and inflammations. In conclusion, these recent patented innovations indicated that SVF has the prospect of providing a better quality of life to patients; however, more studies are needed before approval from the FDA for clinical applications.
Similar content being viewed by others
References
Dykstra JA, et al. Concise review: fat and furious: harnessing the full potential of adipose-derived stromal vascular fraction. Stem Cells Transl Med. 2017;6(4):1096–108.
Prockop DJ. Repair of tissues by adult stem/progenitor cells (MSCs): controversies, myths, and changing paradigms. Molecular Therapy: J Am Soc Gene Ther. 2009;17(6):939–46.
Senesi L, et al. Mechanical and enzymatic procedures to isolate the stromal vascular fraction from adipose tissue: preliminary rResults. Front Cell Dev Biol. 2019;7:88.
Boris V, Afanasyev EEE, Axel R, Zander AJ. Friedenstein, founder of the mesenchymal stem cell concept. Cell Ther Transplant. 2009;1(3):35–8.
Russo A, et al. Autologous micro-fragmented adipose tissue for the treatment of diffuse degenerative knee osteoarthritis: an update at 3 year follow-up. J Exp Orthop. 2018;5(1):52.
Pak, J., et al., Cartilage regeneration in humans with adipose tissue-derived stem cells and adipose stromal vascular fraction cells: updated status. International journal of molecular sciences, 2018. 19(7).
Kemilew J, et al. The use of allogenic stromal vascular fraction (SVF) cells in degenerative joint disease of the spine in dogs. In Vivo. 2019;33(4):1109–17.
Desando, G., et al., Regenerative features of adipose tissue for osteoarthritis treatment in a rabbit model: enzymatic digestion versus mechanical disruption. International journal of molecular sciences, 2019. 20(11).
Lv X, et al. Comparative efficacy of autologous stromal vascular fraction and autologous adipose-derived mesenchymal stem cells combined with hyaluronic acid for the treatment of sheep osteoarthritis. Cell Transplant. 2018;27(7):1111–25.
Yokota N, et al. Comparative clinical outcomes after intra-articular injection with adipose-derived cultured stem cells or noncultured stromal vascular fraction for the treatment of knee osteoarthritis. Am J Sports Med. 2019;47(11):2577–83.
Nurnberger S, et al. Adipose-tissue-derived therapeutic cells in their natural environment as an autologous cell therapy strategy: the microtissue-stromal vascular fraction. Eur Cell Mater. 2019;37:113–33.
Shimozono Y, et al. Adipose-based therapies for knee pain-fat or fiction. J Knee Surg. 2019;32(1):55–64.
Ramakrishnan VM, Boyd NL. The adipose stromal vascular fraction as a complex cellular source for tissue engineering applications. Tissue Eng Part B Rev. 2018;24(4):289–99.
Polancec, D., et al., Immunophenotyping of a stromal vascular fraction from microfragmented lipoaspirate used in osteoarthritis cartilage treatment and its lipoaspirate counterpart. Genes, 2019. 10(6).
Chang JZL, Lu M, Meng TW, Han C. Ding Systemic and local adipose tissue in knee osteoarthritis. Osteoarthr Cartil. 2018;26(7):864–71.
Salikhov RZ, et al. The stromal vascular fraction from fat tissue in the treatment of osteochondral knee defect: case report. Front Med. 2018;5:154.
Michalek, J., et al., Stromal vascular fraction cells of adipose and connective tissue in people with osteoarthritis: a case control prospective multi-centric non-randomized study. Global Surgery, 2017. 3(3).
Fotouhi A, et al. Platelet rich plasma, stromal vascular fraction and autologous conditioned serum in treatment of knee osteoarthritis. Biomed Pharmacother Biomed Pharmacother. 2018;104:652–60.
Lee MJ, Wu Y, Fried SK. Adipose tissue heterogeneity: implication of depot differences in adipose tissue for obesity complications. Mol Aspects Med. 2013;34(1):1–11.
Bisicchia, S., et al., Micro-fragmented stromal-vascular fraction plus microfractures provides better clinical results than microfractures alone in symptomatic focal chondral lesions of the knee. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA, 2019.
Ashammakhi N, et al. Minimally invasive and regenerative therapeutics. Adv Mater. 2019;31(1):e1804041.
Garza JR, et al. Clinical efficacy of intra-articular mesenchymal stromal cells for the treatment of knee osteoarthritis: a double-blinded prospective randomized controlled clinical trial. Am J Sports Med. 2020;48(3):588–98.
Russo A, et al. Autologous and micro-fragmented adipose tissue for the treatment of diffuse degenerative knee osteoarthritis. J Exp Orthop. 2017;4(1):33.
Kilinc, M.O., et al., The ratio of ADSCs to HSC-progenitors in adipose tissue derived SVF may provide the key to predict the outcome of stem-cell therapy. Clin Transl Med, 2018. 7.
Mark, B., et al., Prospective study of autologous adipose derived stromal vascular fraction containing stem cells for the treatment of knee osteoarthritis. Int J Stem Cell Res Ther, 2019. 6(1).
Parsons AM, et al. Regenerative potential and inflammation-induced secretion profile of human adipose-derived stromal vascular cells are influenced by donor variability and prior breast cancer diagnosis. Stem Cell Rev Rep. 2018;14(4):546–57.
Dominici M, C.L., Veronesi E, Piccinno S.E, Paolucci P, De Santis G, Conte P. , Method of obtaining a population of cells. U.S. Patent and Trademark Office, 2014. U.S. Patent No. 10273457 https://patents.justia.com › patent › 20140302605.
March K.L, J.B.H., Methods for preventing aggregation of adipose stromal cells. . U.S. Patent and Trademark Office, 2011. U.S Application No: 20110208162. https://patentscope.wipo.int/search/en/detail.jsf?docId = WO2010048628.
March K.L, J.B.H., Adipose stromal vascular fraction-conditioned medium. U.S. Patent and Trademark Office 2015. Application No: 20150147409. https://patents.justia.com/patent/20150147409
March K.L, R.J., Adipose tissue-derived stromal cells and methods of isolating and using the same. . U.S. Patent and Trademark Office 2012. U.S Application No. 20120129253. https://patents.google.com/patent/US20120129253A1/en.
Rosson G, E.J.H., Nahas Z, Ye Z, Hillel A . , Compositions and methods for implantation of adipose tissue and adipose tissue products. U.S. Patent and Trademark Office., 2011. U.S. Patent No. 9441200. https://uspto.report/patent/app/20110183001.
Y., W.A., Differential gradient separation of cells. U.S. Patent and Trademark Office, 2012. U.S. Patent No. 8283169. https://patents.google.com/patent/US8283169B1/en.
Herbert., B., Biomarkers for cell therapy. International Patent Publication, 2016. International Application No. 20160245825. https://patents.google.com/patent/US20160245825A1/en.
Lindner B, W.C., Babinsky F, Niklas F, Winkler KW, Runow A, Schlee G, Device for transplanting body fat. U.S. Patent and Trademark Office, 2017. U.S Patent Application No. 15/298,889. https://patents.justia.com/patent/20170113005.
Kensy A, W.K., Procedure and device for separating adult stem cells from fatty tissue. U.S. Patent and Trademark Office, 2014. U. S Patent No. 8628950. https://portal.unifiedpatents.com/patents/patent/US-20120100611-A1.
R.M., F., Methods and apparatus for collecting and separating regenerative cells from adipose tissue. International Patent Publication, 2011. International Application No. 20110086426. https://patents.justia.com/patent/2011008642.
Hedrick M.H, F.J.K., Systems and methods for manipulation of regenerative cells from adipose tissue. Patent and Trademark Office. , 2013. U.S Application No. 20130288290. https://patents.google.com/patent/WO2007139551A1/en.
Cimino w. w, L.R., Katz A. J, Tissue processing apparatus and method for processing adipose tissue. U.S. Patent and Trademark Office, 2015. U.S. Patent No. 9296984. https://portal.unifiedpatents.com/patents/patent/US-9296984-B2.
Khan S. M, D.F.E., Breite A. G., Activating adipose-derived stem cells for transplantation. U.S. Patent and Trademark Office, 2015. U. S Patent No. 9650608. https://patents.google.com/patent/US20150037289.
Stubbers R, C.M., Apparatus and methods for cell isolation. U.S. Patent and Trademark Office. , 2014. U. S Patent No. 8822202. https://patents.google.com/patent/US20130337551.
Zaeem A. K. A, D.-T.A.R., Rakuff S, Shoemaker P. L, Kvam E. L, Chen X, Roy J., Automated systems and methods for isolating regenerative cells from adipose tissue U.S. Patent and Trademark Office., 2015. U. S Patent No. 9109198. https://patents.google.com/patent/US20120276628.
Wu A.Y, M.D.M., Method and apparatus for increasing adipose vascular fraction. U.S. Patent and Trademark Office., 2010. U. S Patent No. 8446586. https://patents.google.com/patent/US20100112084.
Fraser J. K, H.M.H., Methods of making enhanced, autologous fat grafts. U.S. Patent and Trademark Office., 2011. U.S Patent No. 7901672. https://patents.google.com/patent/US20110003388.
Hedrick M. H, F.J.K., Schulzki M. J, Byrnes B, Carlson G, Schreiber R. E, Wulur Systems for isolating and using clinically safe adipose derived regenerative cells. Patent and Trademark Office. , 2018. U. S Patent No. 10119113. https://patents.google.com/patent/US20160137970
Casteilla L, P.-B.V., Penicaud L, Chanut C. , Method for culturing cells derived from the adipose tissue and uses. U.S. Patent and Trademark Office., 2009. U. S Patent No. 8945920. https://patents.google.com/patent/US20090246182A1/en.
March K. L, R.J., Cells derived from adipose tissue and methods of isolation and uses U.S. Patent and Trademark Office, 2019. U. S Application No. US 2019 / 0169573 A1. https://patentscope.wipo.int/search/en/detail.jsf?docId = US243294872&tab = PCTCLAIMS&_cid = P12-KV9UEC-80835–241.
Silva F. J, W.M., Patel A. N, Bull D. A. , Brown fat cell compositions and methods. . U.S. Patent and Trademark Office., 2014. U. S Patent No. 10597638. https://patents.justia.com/patent/20140023622.
Rosson G, E.J.H., Nahas Z, Ye Z, Hillel A. , Compositions and methods for implantation of adipose tissue and adipose tissue products. U.S. Patent and Trademark Office, 2011. U. S Patent No. 9441200. https://uspto.report/patent/app/20110183001.
C, Y.-d.H., Differentiation of adipose stromal cells into osteoblasts and uses thereof. U.S. Patent and Trademark Office, 2007. U. S Patent No. 9200255B2. https://patents.google.com/patent/US20070134211A1/en
Fraser J. K, H.M.H., Zhu M, Strem B M, Daniels M, Wulur I, Methods of using adipose tissue-derived cells in the treatment of cardiovascular conditions. U.S. Patent and Trademark Office, 2017. . U. S Patent No. 9597395. https://patents.google.com/patent/US20060083720A1/en.
Fraser J. K, H.M.H., Daniels E, Methods of using regenerative cells in the treatment of erectile dysfunction. U.S. Patent and Trademark Office., 2017. U. S Patent No. 9849149. https://patents.justia.com/patent/9849149.
Fraser J. k, H.M.H., Strem B. M, Methods of using regenerative cells in the treatment of stroke and related diseases and disorders. U.S. Patent and Trademark Office, 2016. U. S Patent No. 9511094. https://patents.justia.com/patent/9511094.
Fraser J. K, H.M.H., Daniels E Methods of using regenerative cells to promote epithelialization or neodermis formation. U.S. Patent and Trademark Office, 2018. U. S Patent No. 9872877. https://patents.justia.com/patent/9872877.
Vesey G, W.R.A., Pharmaceutical compositions and topical use thereof. U.S. Patent and Trademark Office, 2017. U. S Patent No. 9730964. https://patents.google.com/patent/US20140087001A1/en.
G., V., Therapeutic methods using adipose tissue-derived cell suspensions comprising adipocytes. U.S. Patent and Trademark Office, 2011. U. S Patent No. 9062288. https://patents.google.com/patent/US20110293577/ko.
Gimble J. M, L.M., Use of adipose tissue-derived stromal cells in spinal fusion. . U.S. Patent and Trademark Office, 2012. U. S Patent No. 8313743. https://patents.google.com/patent/US8313743B2/en.
Tamarat R, B.M., Use of adipose-tissue cell fractions for post-irradiation tissue regeneration. U.S. Patent and Trademark Office, 2012. U. S Patent No. 8173119. https://patents.google.com/patent/US20100233134.
March K. L, R.J., Adipose stromal stem cells for tissue and vascular modification. U.S. Patent and Trademark Office, 2019. U.S Patent Application No. 20120269775. https://patents.justia.com/patent/20120269775.
Rigotti G, B.G., Breast reconstruction or augmentation using computer modeled deposition of processed adipose tissue. U.S. Patent and Trademark Office, 2009. U.S Patent Application No. 20090181104. https://patentscope.wipo.int/search/ru/detail.jsf?docId = US42790951&tab = PCTCLAIMS.
Vesey G, W.R.A., Lilischkis R Therapeutics using adipose cells and cell secretions. Patent and Trademark Office, 2018. U. S Patent No. 10111909. https://patents.google.com/patent/US20140234272A1/en.
Bravo E, P.M., Adipose tissue-derived stromal stem cells for use in treating refractory complex perianal fistulas in Crohn's disease U.S. Patent and Trademark Office, 2019. U. S Patent No. 10357518. U.S. https://patentscope.wipo.int/search/zh/detail.jsf?docId = US203767469&tab = PCTCLAIMS.
Miguel M. G. F, D.L.P.M.A.G., Castro R. A. G, Arranz M. G, Garcia-Olmo D., Use of adipose tissue-derived stromal stem cells in treating fistula. U.S. Patent and Trademark Office, 2020. U. S Patent No. 10548924. https://patents.google.com/patent/US20140072539
Ude CC, et al. Stromal vascular fraction for osteoarthritis of the knee regenerative engineering. Regen Eng Trans Med. 2022;8(2):210–24.
Cato T, Laurencin AM. Regenerative cell-based therapies: cutting edge, bleeding edge, and off the edge. Regen Eng Trans Med. 2020;6:78–89.
Laurencin CT, Nair LS. Regenerative engineering: approaches to limb regeneration and other grand challenges. Regen Eng Trans Med. 2015;1(1):1–3.
Laurencin, C.T. and Y. Khan, Regenerative engineering. Google Books. (Laurencin, Cato T., Khan Y, ed.) CRC Press/Taylor & Francis Group, 2013.
Escobar Ivirico JL, et al. Regenerative engineering for knee osteoarthritis treatment: biomaterials and cell-based technologies. Eng. 2017;3(1):16–27.
Kasir R, Vernekar VN, Laurencin CT. Regenerative engineering of cartilage using adipose-derived stem cells. Regen Eng Trans Med. 2015;1(1):42–9.
Laurencin CT, Khan Y. Regenerative engineering. Sci Trans Med. 2012;4(160):160ed9.
Paulos Y. Mengsteab, J.F., Mohammed A. Barajaa, Lakshmi S. Nair & Cato T. Laurencin., Ligament regenerative engineering: braiding scalable and tunable bioengineered ligaments using a BenchTop braiding machine. Regenerative Engineering and Translational Medicine, 2020.
CT Laurencin, L.N., Nanotechnology and tissue engineering - the caffold. CRC Press; 1st edition, 2008: 384.
Onoi Y, et al. Second-look arthroscopic findings of cartilage and meniscus repair after injection of adipose-derived regenerative cells in knee osteoarthrits: Report of two cases. Regen Ther. 2019;11:212–6.
Kumbar SG, et al. Polymeric nanofibers as novel carriers for the delivery of therapeutic molecules. J Nanosci Nanotechnol. 2006;6(9–10):2591–607.
Shiv Shah TO, Bhattacharjee M, Laurencin CT. Minimally invasive cellular therapies for osteoarthritis treatment. Regen Eng Trans Med. 2021;7:76–90.
Daneshmandi L, et al. Emergence of the stem cell secretome in regenerative engineering. Trends Biotechnol. 2020;38(12):1373–84.
Rodriguez J, et al. Evaluation of three devices for the isolation of the stromal vascular fraction from adipose tissue and for ASC culture: a comparative study. Stem Cells Int. 2017;2017:9289213.
Otsuka T, et al. Identification of heparan-sulfate rich cells in the loose connective tissues of the axolotl (Ambystoma mexicanum) with the potential to mediate growth factor signaling during regeneration. Regen Eng Trans Med. 2020;6(1):7–17.
Ganesh Narayanan MB, Nair LS, Laurencin CT. Musculoskeletal tissue regeneration: the role of the stem cells. Regen Eng Trans Med. 2017;3:133–65.
Beachy SH, CatoLaurencin LN, Tsokas KA, Lundberg MS. Sources of variability in clinical translation of regenerative engineering products: insights from the national academies forum on regenerative medicine. Regen Eng Trans Med. 2020;6:1–6.
Barajaa MA, Nair LS, Laurencin CT. Bioinspired scaffold designs for regenerating musculoskeletal tissue interfaces. Regen Eng Trans Med. 2020;6(4):451–83.
Roato I, et al. Concentrated adipose tissue infusion for the treatment of knee osteoarthritis: clinical and histological observations. Int Orthop. 2019;43(1):15–23.
Tang X, et al. Biomimetic electroconductive nanofibrous matrices for skeletal muscle regenerative engineering. Regen Eng Trans Med. 2020;6(2):228–37.
Ifegwu OC, ManKan GAH, Rajpura K, O’Neill E, Kuo C-L, Lo KW-H. Bone regenerative engineering using a protein kinase A-specific cyclic AMP analogue administered for short term. Regen Eng Trans Med. 2018;4:206–15.
Jiang T, James MDR, Nair LS, Laurencin CT. Micro- and nanofabrication of chitosan structures for regenerative engineering. Acta Biomaterialia. 2014;10(4):1632–45.
Ogueri KS, et al. Polymeric biomaterials for scaffold-based bone regenerative engineering. Regen Eng Trans Med. 2019;5(2):128–54.
Kumar A, Kadamb AG, Kadamb K. Understanding the role of platelet rich plasma bone marrow concentrate micro fragmented adipose tissue stromal vascular fraction and stem cell in osteoarthritis of the knee - its time to wake up! EC Orthopaedics. 2019;10(9):804–12.
Wong SP, et al. Pericytes, mesenchymal stem cells and their contributions to tissue repair. Pharmacol Ther. 2015;151:107–20.
Meirelles Lda S, et al. Mechanisms involved in the therapeutic properties of mesenchymal stem cells. Cytokine Growth Factor Rev. 2009;20(5–6):419–27.
Tran, T.D.X., et al., Time- and Kellgren(-)Lawrence grade-dependent changes in intra-articularly transplanted stromal vascular fraction in osteoarthritic patients. Cells, 2019. 8(4).
FDA-Canada, Health Canada Policy Position Paper – autologous cell therapy products - Canada.ca. https://www.canada.ca/en/health-canada/services/drugs-health-products/biologics-radiopharmaceuticals-genetic-therapies/applications, 2020.
Gentile P, et al. Concise review: the use of adipose-derived stromal vascular fraction cells and platelet rich plasma in regenerative plastic surgery. Stem cells. 2017;35(1):117–34.
Shiv Shah, C.J.E., Maumita Bhattacharj, Ho-Man Kan, Cato T. Laurencin,, The synthetic artificial stem cell (SASC): shifting theparadigm of cell therapy in regenerative engineering. PNASG, 2022. 119 ( 2 ).
Hudetz D, et al. Early results of intra-articular micro-fragmented lipoaspirate treatment in patients with late stages knee osteoarthritis: a prospective study. Croat Med J. 2019;60(3):227–36.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ude, C.C., Dzidotor, G.K., Iloeje, K. et al. Recent Patents Involving Stromal Vascular Fraction. Regen. Eng. Transl. Med. 9, 295–314 (2023). https://doi.org/10.1007/s40883-022-00283-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40883-022-00283-w