Abstract
Background
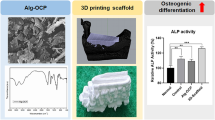
In tissue engineering, cellularization of scaffolds has typically been performed by seeding the cells after scaffold fabrication. 3D-printing technology now allows bioprinting of cells encapsulated in a hydrogel simultaneously with the scaffold material. Here, we aimed to investigate whether bioprinting or cell seeding post-printing is more effective in enhancing responses of pre-osteoblastic MC3T3-E1 cell line derived from mouse calvaria.
Methods
Two methods were used for incorporation of pre-osteoblasts in poly(lactic-co-glycolic acid)/β-tricalcium phosphate (PLGA/β-TCP) scaffolds: first, seeding the cells after scaffold printing, and second, bioprinting of alginate-encapsulated cells between PLGA/β-TCP struts. AlamarBlue® assay was used to determine cell retention and proliferation. Live/dead staining and picrosirius red staining were used to assess cell viability and collagen deposition, respectively. Alkaline phosphatase activity was measured to assess the osteoblastic phenotype of pre-osteoblasts.
Results
Cell retention was 51 ± 5% in cell-seeded and 87 ± 3% in bioprinted scaffolds, whereas cell viabilities were 87 ± 2% and 78 ± 4%, respectively. Cell proliferation was higher on cell-seeded scaffolds (day 7: 2.5-fold, day 14: 4.0-fold, day 21: 4.7-fold) compared with bioprinted scaffolds (1.2-fold, 2.1-fold, and 3.9-fold, respectively). At day 21, the voids between PLGA/β-TCP struts were covered with cell-deposited collagenous matrix in both scaffold types. Alkaline phosphatase activity was higher (3.4-fold) on cell-seeded scaffolds compared with bioprinted scaffolds.
Conclusion
Our data demonstrate that encapsulation of pre-osteoblasts in alginate and printing inside PLGA/β-TCP scaffolds enhances cell retention but decreases cell proliferation and osteogenic differentiation compared to seeding cells on scaffolds post-printing. This might have important implications for bone tissue engineering.
Lay Summary
Bioprinting, i.e., printing of hydrogel-encapsulated cells alone or in combination with scaffold material, presents an attractive tool for fabrication of customized tissue equivalents as opposed to conventional cell seeding on tissue engineering scaffolds. However, the function of the printed cells might be adversely affected by the hydrogel encapsulation and printing process. Our aim was to investigate whether bioprinting of alginate-encapsulated pre-osteoblasts in poly(lactic-co-glycolic) acid/β-tricalcium phosphate scaffold is more effective in enhancing cell retention, proliferation, and osteogenic differentiation as opposed to cell seeding post-printing. Our studies showed that the bioprinted scaffold had enhanced cell retention capacity, but impaired cell proliferation and osteogenic differentiation compared to the cell-seeded scaffold. These findings might have important implications for the improvement of alginate-based bioinks with, e.g., (natural) bioactive peptides for bioprinting of bone tissue engineering scaffolds.

Grapical abstract




Similar content being viewed by others
References
Buza JA III, Einhorn T. Bone healing in 2016. Clin Cases Miner Bone Metab. 2016;13:101–5. https://doi.org/10.11138/ccmbm/2016.13.2.101.
Marino JT, Ziran BH. Use of solid and cancellous autologous bone graft for fractures and nonunions. Orthop Clin North Am. 2010;41:15–26. https://doi.org/10.1016/j.ocl.2009.08.003.
Nerem RM. Regenerative medicine: the emergence of an industry. J R Soc Interface. 2010;7:S771–5. https://doi.org/10.1098/rsif.2010.0348.focus.
Arul KT, Manikandan E, Ladchumananandasivam R. Polymer-based calcium phosphate scaffolds for tissue engineering applications. In: Grumezescu AM, editor. Nanoarchitectonics in Biomedicine: William Andrew Publishing; 2019. p. 585–618. https://doi.org/10.1016/B978-0-12-816200-2.00011-6.
Ramesh N, Moratti SC, Dias GJ. Hydroxyapatite-polymer biocomposites for bone regeneration: a review of current trends. J Biomed Mater Res B App Biomater. 2018;106:2046–57. https://doi.org/10.1002/jbm.b.33950.
Yu NY, Schindeler A, Little DG, Ruys AJ. Biodegradable poly (α-hydroxy acid) polymer scaffolds for bone tissue engineering. J Biomed Mater Res B App Biomater. 2010;93:285–95. https://doi.org/10.1002/jbm.b.31588.
Felfel R, Poocza L, Gimeno-Fabra M, Milde T, Hildebrand G, Ahmed I, et al. In vitro degradation and mechanical properties of PLA-PCL copolymer unit cell scaffolds generated by two-photon polymerization. Biomed Mater. 2016;11:015011. https://doi.org/10.1088/1748-6041/11/1/015011.
Pan Z, Ding J. Poly(lactide-co-glycolide) porous scaffolds for tissue engineering and regenerative medicine. Interface Focus. 2012;2:366–77. https://doi.org/10.1098/rsfs.2011.0123.
Sun X, Xu C, Wu G, Ye Q, Wang C. Poly(lactic-co-glycolic acid): applications and future prospects for periodontal tissue regeneration. Polymers (Basel). 2017;9:189. https://doi.org/10.3390/polym9060189.
Yoshida T, Miyaji H, Otani K, Inoue K, Nakane K, Nishimura H, et al. Bone augmentation using a highly porous PLGA/β-TCP scaffold containing fibroblast growth factor-2. J Periodontal Res. 2015;50:265–73. https://doi.org/10.1111/jre.12206.
Bizenjima T, Takeuchi T, Seshima F, Saito A. Effect of poly (lactide-co-glycolide) (PLGA)-coated beta-tricalcium phosphate on the healing of rat calvarial bone defects: a comparative study with pure-phase beta-tricalcium phosphate. Clin Oral Implants Res. 2016;27:1360–7. https://doi.org/10.1111/clr.12744.
Lee SK, Han CM, Park W, Kim IH, Joung YK, Han DK. Synergistically enhanced osteoconductivity and anti-inflammation of PLGA/β-TCP/mg(OH)2 composite for orthopedic applications. Mater Sci Eng C Mater Biol Appl. 2019;94:65–75. https://doi.org/10.1016/j.msec.2018.09.011.
Roseti L, Parisi V, Petretta M, Cavallo C, Desando G, Bartolotti I, et al. Scaffolds for bone tissue engineering: state of the art and new perspectives. Mater Sci Eng C. 2017;78:1246–62. https://doi.org/10.1016/j.msec.2017.05.017.
Miar S, Shafiee A, Guda T, Narayan R. Additive manufacturing for tissue engineering. In: Ovsianikov A, Yoo J, Mironov V, editors. 3D printing and biofabrication. Cham: Reference Series in Biomedical Engineering. Springer; 2018. p. 3–54. https://doi.org/10.1007/978-3-319-45444-3_2.
Chan BP, Leong KW. Scaffolding in tissue engineering: general approaches and tissue-specific considerations. Eur Spine J. 2008;17:467–79. https://doi.org/10.1007/s00586-008-0745-3.
Piard CM, Chen Y, Fisher JP. Cell-laden 3D printed scaffolds for bone tissue engineering. Clin Rev Bone Miner Metab. 2015;13:245–55. https://doi.org/10.1007/s12018-015-9198-5.
England S, Rajaram A, Schreyer DJ, Chen X. Bioprinted fibrin-factor XIII-hyaluronate hydrogel scaffolds with encapsulated Schwann cells and their in vitro characterization for use in nerve regeneration. Bioprinting. 2017;5:1–9. https://doi.org/10.1016/j.bprint.2016.12.001.
Duarte CD, Blaeser A, Weber M, Jäkel J, Neuss S, Jahnen-Dechent W, et al. Three-dimensional printing of stem cell-laden hydrogels submerged in a hydrophobic high-density fluid. Biofabrication. 2013;5:015003. https://doi.org/10.1088/1758-5082/5/1/015003.
Tabriz AG, Hermida MA, Leslie NR, Shu W. Three-dimensional bioprinting of complex cell laden alginate hydrogel structures. Biofabrication. 2015;7:045012. https://doi.org/10.1088/1758-5090/7/4/045012.
Pepelanova I, Kruppa K, Scheper T, Lavrentieva A. Gelatin-methacryloyl (GelMA) hydrogels with defined degree of functionalization as a versatile toolkit for 3D cell culture and extrusion bioprinting. Bioengineering (Basel). 2018;5:55. https://doi.org/10.3390/bioengineering5030055.
Pawar SN, Edgar KJ. Alginate derivatization: a review of chemistry, properties and applications. Biomaterials. 2012;33:3279–305. https://doi.org/10.1016/j.biomaterials.2012.01.007.
Axpe E, Oyen M. Applications of alginate-based bioinks in 3D bioprinting. Int J Mol Sci. 2016;17:1976. https://doi.org/10.3390/ijms17121976.
Bendtsen ST, Quinnell SP, Wei M. Development of a novel alginate-polyvinyl alcohol-hydroxyapatite hydrogel for 3D bioprinting bone tissue engineered scaffolds. J Biomed Mater Res A. 2017;105:1457–68. https://doi.org/10.1002/jbm.a.36036.
Schuurman W, Khristov V, Pot MW, van Weeren PR, Dhert WJ, Malda J. Bioprinting of hybrid tissue constructs with tailorable mechanical properties. Biofabrication. 2011;3:021001. https://doi.org/10.1088/1758-5082/3/2/021001.
Detsch R, Sarker B, Grigore A, Boccaccini AR. Alginate and gelatine blending for bone cell printing and biofabrication. In: IASTED International Conference Biomedical Engineering Innsbruck. Innsbruck: ACTA Press; 2013. p. 451–5. https://doi.org/10.2316/P.2013.791-177.
Gelinsky M. Biopolymer hydrogel bioinks. In: Thomas DJ, Jessop ZM, Whitaker IS, editors. 3D Bioprinting for Reconstructive Surgery: Woodhead Publishing; 2018. p. 125–36. https://doi.org/10.1016/B978-0-08-101103-4.00008-9.
Blaeser A, Duarte Campos DF, Puster U, Richtering W, Stevens MM, Fischer H. Controlling shear stress in 3D bioprinting is a key factor to balance printing resolution and stem cell integrity. Adv Healthc Mater. 2016;5:326–33. https://doi.org/10.1002/adhm.201500677.
Wang W, Caetano G, Ambler WS, Blaker JJ, Frade MA, Mandal P, et al. Enhancing the hydrophilicity and cell attachment of 3D printed PCL/graphene scaffolds for bone tissue engineering. Materials. 2016;9:992–103. https://doi.org/10.3390/ma9120992.
Kroeze RJ, Knippenberg M, Helder MN. Osteogenic differentiation strategies for adipose-derived mesenchymal stem cells. Methods Mol Biol. 2011;702:233–48. https://doi.org/10.1007/978-1-61737-960-4_17.
Zamani Y, Mohammadi J, Amoabediny G, Visscher DO, Helder MN, Zandieh-Doulabi B, et al. Enhanced osteogenic activity by MC3T3-E1 pre-osteoblasts on chemically surface-modified poly (ε-caprolactone) 3D-printed scaffolds compared to RGD immobilized scaffolds. Biomed Mater. 2018;14:015008. https://doi.org/10.1088/1748-605X/aaeb82.
Tserepi A, Gogolides E, Bourkoula A, Kanioura A, Kokkoris G, Petrou P, et al. Plasma nano textured polymeric surfaces for controlling cell attachment and proliferation: a short review. Plasma Chem Plasma P. 2016;36:107–20. https://doi.org/10.1007/s11090-015-9674-1.
Chang R, Nam J, Sun W. Effects of dispensing pressure and nozzle diameter on cell survival from solid free form fabrication-based direct cell writing. Tissue Eng Part A. 2008;14:41–8. https://doi.org/10.1089/ten.a.2007.0004.
Nair K, Gandhi M, Khalil S, Yan KC, Marcolingo M, Barbee K, et al. Characterization of cell viability during bioprinting processes. Biotechnol J. 2009;4:1168–77. https://doi.org/10.1002/biot.200900004.
Sarker B, Rompf J, Silva R, Lang N, Detsch R, Kaschta J, et al. Alginate-based hydrogels with improved adhesive properties for cell encapsulation. Int J Biol Macromol. 2015;78:72–8. https://doi.org/10.1016/j.ijbiomac.2015.03.061.
Jia J, Richards DJ, Pollard S, Tan Y, Rodriguez J, Visconti RP, et al. Engineering alginate as bioink for bioprinting. Acta Biomater. 2014;10:4323–31. https://doi.org/10.1016/j.actbio.2014.06.034.
Gungor-Ozkerim PS, Inci I, Zhang YS, Khademhosseini A, Dokmeci MR. Bioinks for 3D bioprinting: an overview. Biomater Sci. 2018;6:915–46. https://doi.org/10.1039/C7BM00765E.
Das RK. Harnessing cell-material interaction to control cell fate: design principle of advanced functional hydrogel materials. J Chem Sci. 2017;129:1807–16. https://doi.org/10.1007/s12039-017-1387-y.
Tsukanaka M, Fujibayashi S, Otsuki B, Takemoto M, Matsuda S. Osteoinductive potential of highly purified porous β-TCP in mice. J Mater Sci Mater Med. 2015;26:132. https://doi.org/10.1007/s10856-015-5469-4.
Wilson JL, Najia MA, Saeed R, McDevitt TC. Alginate encapsulation parameters influence the differentiation of microencapsulated embryonic stem cell aggregates. Biotechnol Bioeng. 2014;111:618–31. https://doi.org/10.1002/bit.25121.
Khatab S, Leijs MJ, van Buul GM, Haeck JC, Kops N, Bos KP, et al. Encapsulation in alginate beads prolongs mesenchymal stem cell longevity in vivo but does not enhance their therapeutic efficacy in a murine model for osteoarthritis. Osteoarth Cart. 2019;27:S425–6. https://doi.org/10.1016/j.joca.2019.02.444.
Availability of Data and Material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conceptualization: Yasaman Zamani, Marco N. Helder, Behrouz Zandieh-Doulabi, Jenneke Klein-Nulend. Methodology: Yasaman Zamani, Marco N. Helder, Behrouz Zandieh-Doulabi, Jenneke Klein-Nulend. Formal analysis: Yasaman Zamani, Behrouz Zandieh-Doulabi. Investigation: Yasaman Zamani, Behrouz Zandieh-Doulabi. Data curation: Yasaman Zamani. Writing—original draft: Yasaman Zamani. Writing—review and editing: Yasaman Zamani, Javad Mohammadi, Ghassem Amoabediny, Marco N. Helder, Behrouz Zandieh-Doulabi, Jenneke Klein-Nulend. Resources: Javad Mohammadi, Ghassem Amoabediny, Marco N. Helder, Behrouz Zandieh-Doulabi, Jenneke Klein-Nulend. Supervision: Ghassem Amoabediny, Marco N. Helder, Behrouz Zandieh-Doulabi, Jenneke Klein-Nulend.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Description of Future Works
Future works include incorporation of varying concentrations of (natural) bioactive peptides in the bioink formulation to compensate for the bioinertness of alginate for enhanced osteogenic activity by the bioprinted cells.
Rights and permissions
About this article
Cite this article
Zamani, Y., Mohammadi, J., Amoabediny, G. et al. Bioprinting of Alginate-Encapsulated Pre-osteoblasts in PLGA/β-TCP Scaffolds Enhances Cell Retention but Impairs Osteogenic Differentiation Compared to Cell Seeding after 3D-Printing. Regen. Eng. Transl. Med. 7, 485–493 (2021). https://doi.org/10.1007/s40883-020-00163-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40883-020-00163-1