Abstract
Purpose
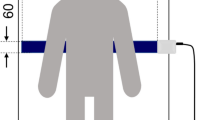
Respiration during sleep is one of the indicators of an individual’s health. However, many respiratory measurement devices need to be worn by the patient and can affect sleep. We introduce here a novel, easy-to-use, respiratory rate-monitoring sensor made of stretchable piezoelectric material that can be used conveniently at home as well as in a clinical setting.
Methods
We enrolled 6 members of a family as volunteers ranging in age from 9 months to 69 years. The sensor was used to continuously record respiratory rate data for all individuals during sleep.
Results
The sensor could detect known breathing patterns such as stable, unstable, or deep breathing as well as apnea during sleep. We observed significant differences in the respiratory rates and respiratory stability between subjects during sleep.
Conclusion
The piezoelectric sensor was effective in people in all age groups, paving a way for future use as a convenient and reliable mode of respiratory assessment for adults as well as neonates at home and in a clinical setting.




Similar content being viewed by others
References
World Health Organization. (1984). A programme for controlling acute respiratory infections in children: Memorandum from a WHO meeting. Bulletin of the World Health Organization, 62, 47–58.
Moon, R. Y., Darnall, R. A., Feldman-Winter, L., Goodstein, M. H., & Hauck, F. R. (2016). SIDS and other sleep-related infant deaths: Evidence base for 2016 updated recommendations for a safe infant sleeping environment. Pediatrics, 138(5), e20162940. https://doi.org/10.1542/peds.2016-2940.
Kinney, H. C., & Thach, B. T. (2009). The sudden infant death syndrome. New England Journal of Medicine, 361, 795–805. https://doi.org/10.1056/NEJMra0803836.
Guilleminault, C., & Quo, S. D. (2001). Sleep-disordered breathing. A view at the beginning of the new Millennium. Dental Clinics of North America, 45, 643–656.
Vaessen, T. J. A., Overeem, S., & Sitskoorn, M. M. (2015). Cognitive complaints in obstructive sleep apnea. Sleep Medicine Reviews. https://doi.org/10.1016/j.smrv.2014.03.008.
Berry, R. B., Budhiraja, R., Gottlieb, D. J., Gozal, D., Iber, C., Kapur, V. K., et al. (2012). Rules for scoring respiratory events in sleep: Update of the 2007 AASM manual for the scoring of sleep and associated events. Journal of Clinical Sleep Medicine, 8(5), 597–619. https://doi.org/10.5664/jcsm.2172.
Seymour, C. W., Liu, V. X., Iwashyna, T. J., Brunkhorst, F. M., Rea, T. D., Scherag, A., et al. (2016). Assessment of clinical criteria for sepsis for the third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA - Journal of the American Medical Association, 315(8), 762–774. https://doi.org/10.1001/jama.2016.0288.
Al-Sayed, L. E., Schrank, W. I., & Thach, B. T. (1994). Ventilatory sparing strategies and swallowing pattern during bottle feeding in human infants. Journal of Applied Physiology, 77(1), 78–83. https://doi.org/10.1152/jappl.1994.77.1.78.
Gewolb, I. H., Vice, F. L., Schweitzer-Kenney, E. L., Taciak, V. L., & Bosma, J. F. (2001). Developmental patterns of rhythmic suck and swallow in preterm infants. Developmental Medicine and Child Neurology, 43(1), 22–27. https://doi.org/10.1017/S0012162201000044.
Gewolb, I. H., & Vice, F. L. (2006). Maturational changes in the rhythms, patterning, and coordination of respiration and swallow during feeding in preterm and term infants. Developmental Medicine and Child Neurology, 48(7), 589–594. https://doi.org/10.1017/S001216220600123X.
Butterworth, S. (1930). On the theory of filter amplifiers. Experimental Wireless and the Wireless Engineer, 7, 536–541.
Barrett, K. E., Boitano, S., Barman, S. M., & Brooks, H. L. (2010). Respiratory physiology. In W. F. Ganong (Ed.), Ganong’s review of medical physiology (p. 588). Pennsylvania: The McGraw-Hill Companies Inc.
Bendixen, H. H., Smith, G. M., & Mead, J. (2017). Pattern of ventilation in young adults. Journal of Applied Physiology, 19(2), 195–198. https://doi.org/10.1152/jappl.1964.19.2.195.
Hathorn, M. K. S. (1974). The rate and depth of breathing in new-born infants in different sleep states. The Journal of Physiology, 243(1), 101–113. https://doi.org/10.1113/jphysiol.1974.sp010744.
Rodríguez-Molinero, A., Narvaiza, L., Ruiz, J., & Gálvez-Barrõn, C. (2013). Normal respiratory rate and peripheral blood oxygen saturation in the elderly population. Journal of the American Geriatrics Society. https://doi.org/10.1111/jgs.12580.
Rusconi, F., Castagneto, M., Gagliardi, L., Leo, G., Pellegatta, A., Porta, N., et al. (1994). Reference values for respiratory rate in the first 3 years of life. Pediatrics, 94(3), 350–355.
Douglas, N. J., White, D. P., Pickett, C. K., Weil, J. V., & Zwillich, C. W. (1982). Respiration during sleep in normal man. Thorax, 37(11), 840–844. https://doi.org/10.1136/thx.37.11.840.
Parmelee, A. H., Schulz, H. R., & Disbrow, M. A. (1961). Sleep patterns of the newborn. The Journal of Pediatrics, 58(2), 241–250. https://doi.org/10.1016/S0022-3476(61)80164-9.
Peng, M., Ding, Z., Wang, L., & Cheng, X. (2019). Detection of sleep biosignals using an intelligent mattress based on piezoelectric ceramic sensors†. Sensors (Switzerland), 19(18), 3843. https://doi.org/10.3390/s19183843.
Klap, T., & Shinar, Z. (2010). Using piezoelectric sensor for continuous-contact-free monitoring of heart and respiration rates in real-life hospital settings. Computing in Cardiology, 40(2013), 671–674.
Bu, N., Ueno, N., & Fukuda, O. (2009). Respiration and heartbeat measurement for sleep monitoring using a flexible AlN piezoelectric film sensor. Sensors and Transducers Journal, 109(10), 131–142.
Freundlich, J. J., & Erickson, J. C. (1974). Electrical impedance pneumography for simple nonrestrictive continuous monitoring of respiratory rate, rhythm and tidal volume for surgical patients. Chest, 65(2), 181–184. https://doi.org/10.1378/chest.65.2.181.
Al-Khalidi, F. Q., Saatchi, R., Burke, D., Elphick, H., & Tan, S. (2011). Respiration rate monitoring methods: A review. Pediatric Pulmonology. https://doi.org/10.1002/ppul.21416.
Daw, W. (2016). Medical devices for measuring respiratory rate in children: A review. Journal of Advances in Biomedical Engineering and Technology, 3(1), 21–27. https://doi.org/10.15379/2409-3394.2016.03.01.04.
Storck, K., Karlsson, M., Ask, P., & Loyd, D. (1996). Heat transfer evaluation of the nasal thermistor technique. IEEE Transactions on Biomedical Engineering, 43(12), 1187–1191. https://doi.org/10.1109/10.544342.
Helfenbein, E., Firoozabadi, R., Chien, S., Carlson, E., & Babaeizadeh, S. (2014). Development of three methods for extracting respiration from the surface ECG: A review. Journal of Electrocardiology, 47(6), 819–825. https://doi.org/10.1016/j.jelectrocard.2014.07.020.
Moody, G., Mark, R., Bump, M., Weinstein, J., Berman, A., Mietus, J., & Goldberger, A. (1986). Clinical validation of the ECG-derived respiration (EDR) technique. Computers in Cardiology, 13, 507–510.
Mahbub, I., Pullano, S. A., Wang, H., Islam, S. K., Fiorillo, A. S., To, G., et al. (2017). A low-power wireless piezoelectric sensor-based respiration monitoring system realized in CMOS process. IEEE Sensors Journal, 17, 1858–1864. https://doi.org/10.1109/JSEN.2017.2651073.
Villarroel, M., Guazzi, A., Jorge, J., Davis, S., Watkinson, P., Green, G., et al. (2014). Continuous non-contact vital sign monitoring in neonatal intensive care unit. Healthcare Technology Letters, 1(3), 87–91. https://doi.org/10.1049/htl.2014.0077.
Johansson, A., Oberg, P. A., & Sedin, G. (1999). Monitoring of heart and respiratory rates in newborn infants using a new photoplethysmographic technique. Journal of Clinical Monitoring and Computing, 15(7–8), 461–467.
Olsson, E., Ugnell, H., Oberg, P. A., & Sedin, G. (2000). Photoplethysmography for simultaneous recording of heart and respiratory rates in newborn infants. Acta Paediatrica, 89(7), 853–861. https://doi.org/10.1080/080352500750043774.
Wertheim, D., Olden, C., Savage, E., & Seddon, P. (2009). Extracting respiratory data from pulse oximeter plethysmogram traces in newborn infants. Archives of Disease in Childhood: Fetal and Neonatal Edition, 94(4), F301–F303. https://doi.org/10.1136/adc.2008.145342.
Castaneda, D., Esparza, A., Ghamari, M., Soltanpur, C., & Nazeran, H. (2018). A review on wearable photoplethysmography sensors and their potential future applications in health care. International Journal of Biosensors & Bioelectronics, 4(4), 195. https://doi.org/10.15406/ijbsbe.2018.04.00125.
Poets, C. F., Stebbens, V. A., Alexander, J. R., & Southall, D. P. (1991). Breathing patterns and heart rates at ages 6 weeks and 2 years. American Journal of Diseases of Children, 145(12), 1393–1396. https://doi.org/10.1001/archpedi.1991.02160120061020.
Weese-Mayer, D. E., Morrow, A. S., Conway, L. P., Brouillette, R. T., & Silvestri, J. M. (1990). Assessing clinical significance of apnea exceeding fifteen seconds with event recording. The Journal of Pediatrics, 117(4), 568–574. https://doi.org/10.1016/S0022-3476(05)80690-0.
Sridhar, R., Thach, B. T., Kelly, D. H., & Henslee, J. A. (2003). Characterization of successful and failed autoresuscitation in human infants, including those dying of SIDS. Pediatric Pulmonology, 36(2), 113–122. https://doi.org/10.1002/ppul.10287.
Acknowledgements
The authors would like to thank Sumitomo Riko Company Limited (Japan) for providing the TaidoSensor® for the study. The authors would also like to thank Mr. Ritwik Handa, MBA (Intel Corp., Phoenix, AZ, USA), for providing technical guidance and assistance in this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
SS contributed to the study design and analysis and interpretation of the data and co-wrote the manuscript. DJ contributed to the analysis and interpretation of the data and co-wrote the manuscript. NK is the lead investigator and contributed to the implementation of this study and edited the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare. S.S. belongs to the funded laboratory of the Tawara IVF clinic.
Ethical Approval
All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and its later amendments. The protocol for this study was approved by the Institutional Review Board at Tawara IVF clinic (No. 2019_0024).
Informed Consent
Written informed consent was obtained from all the participants of this study (or their parent or legal guardian in the case of children under 16 years of age) for participation and publication of their data.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
So, S., Jain, D. & Kanayama, N. Piezoelectric Sensor-Based Continuous Monitoring of Respiratory Rate During Sleep. J. Med. Biol. Eng. 41, 241–250 (2021). https://doi.org/10.1007/s40846-021-00602-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-021-00602-6