Abstract
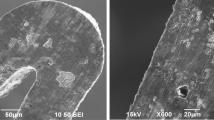
Nitinol is a nickel–titanium alloy widely used in medical devices for its unique pseudoelastic and shape-memory properties. However, nitinol can release potentially hazardous amounts of nickel, depending on surface manufacturing yielding different oxide thicknesses and compositions. Furthermore, nitinol medical devices can be implanted throughout the body and exposed to extremes in pH and reactive oxygen species (ROS), but few tools exist for evaluating nickel release under such physiological conditions. Even in cardiovascular applications, where nitinol medical devices are relatively common and the blood environment is well understood, there is a lack of information on how local inflammatory conditions after implantation might affect nickel ion release. For this study, nickel release from nitinol wires of different finishes was measured in pH conditions and at ROS concentrations selected to encompass and exceed literature reports of extracellular pH and ROS. Results showed increased nickel release at levels of pH and ROS reported to be physiological, with decreasing pH and increasing concentrations of hydrogen peroxide and NaOCl/HOCl having the greatest effects. The results support the importance of considering the implantation site when designing studies to predict nickel release from nitinol and underscore the value of understanding the chemical milieu at the device–tissue interface.




Similar content being viewed by others
References
Wadood A (2016) Brief overview on nitinol as biomaterial [Internet]. Adv Mater Sci Eng. Accessed 4 Nov, 2019. https://www.hindawi.com/journals/amse/2016/4173138/
Eliaz N (2019) Corrosion of metallic biomaterials: a review. Materials 12:407
Rosenbloom SN, Kumar P, Lasley C (2021) The role of surface oxide thickness and structure on the corrosion and nickel elution behavior of nitinol biomedical implants. J Biomed Mater Res B Appl Biomater 109:1334–1343
Saito M, Arakaki R, Yamada A, Tsunematsu T, Kudo Y, Ishimaru N (2016) Molecular mechanisms of nickel allergy. Int J Mol Sci 17:202
Mu Y, Godar DE, Merrill SJ (2017) A perspective on the challenges and issues in developing biomarkers for human allergic risk assessments. Biomark Med 11:523–526
Das KK, Reddy RC, Bagoji IB, Das S, Bagali S, Mullur L et al (2019) Primary concept of nickel toxicity—an overview. J Basic Clin Physiol Pharmacol 30:141–152
Kasprzak KS, Sunderman FW, Salnikow K (2003) Nickel carcinogenesis. Mutat Res Mol Mech Mutagen 533:67–97
Shabalovskaya S, Anderegg J, Van Humbeeck J (2008) Critical overview of Nitinol surfaces and their modifications for medical applications. Acta Biomater 4:447–467
Kim JH, Shin JH, Shin DH, Moon M-W, Park K, Kim T-H et al (2011) Comparison of diamond-like carbon-coated nitinol stents with or without polyethylene glycol grafting and uncoated nitinol stents in a canine iliac artery model. Br J Radiol 84:210–215
Nagaraja S, Sullivan SJL, Stafford PR, Lucas AD, Malkin E (2018) Impact of nitinol stent surface processing on in-vivo nickel release and biological response. Acta Biomater 72:424–433
Hoffman WE, Charbel FT, Edelman G (1996) Brain tissue oxygen, carbon dioxide, and pH in neurosurgical patients at risk for ischemia. Anesth Analg 82:582
Andrews RJ, Bringas JR, Alonzo G (1994) Cerebrospinal fluid pH and PCO2 rapidly follow arterial blood pH and PCO2 with changes in ventilation. Neurosurgery 34:466–470
Ohman H, Vahlquist A (1994) In vivo studies concerning a pH gradient in human stratum corneum and upper epidermis. Acta Derm Venereol 74:375–379
Ng KYB, Mingels R, Morgan H, Macklon N, Cheong Y (2018) In vivo oxygen, temperature and pH dynamics in the female reproductive tract and their importance in human conception: a systematic review. Hum Reprod Update 24:15–34
Obradović D, Husar M, Andelković V, Krstić M (1981) Tufegdzić N [Study of the pH values of uterine secretions in women with and without intrauterine devices]. Jugosl Ginekol Opstet 21:7–10
Halliwell B, Clement MV, Long LH (2000) Hydrogen peroxide in the human body. FEBS Lett 486:10–13
Forman HJ, Bernardo A, Davies KJA (2016) What is the concentration of hydrogen peroxide in blood and plasma? Arch Biochem Biophys 603:48–53
Panasenko OM, Gorudko IV, Sokolov AV (2013) Hypochlorous acid as a precursor of free radicals in living systems. Biochem Mosc 78:1466–1489
Ganong WF (1985) Review of medical physiology, 12th edn. Lange Medical Publications, California
Russell TL, Berardi RR, Barnett JL, Dermentzoglou LC, Jarvenpaa KM, Schmaltz SP et al (1993) Upper gastrointestinal pH in seventy-nine healthy, elderly, north american men and women. Pharm Res 10:187–196
Mattioli S, Pilotti V, Felice V, Lazzari A, Zannoli R, Bacchi ML et al (1990) Ambulatory 24-hr pH monitoring of esophagus, fundus, and antrum. Dig Dis Sci 35:929–938
Wilson CG (2010) The transit of dosage forms through the colon. Int J Pharm 395:17–25
Challa T, Vynala V, Allam KV (2011) Colon specific drug delivery systems: a review on primary and novel approaches. Int J Pharm Sci Rev Res 7:171–181
Nugent SG, Kumar D, Rampton DS, Evans DF (2001) Intestinal luminal pH in inflammatory bowel disease: possible determinants and implications for therapy with aminosalicylates and other drugs. Gut 48:571–577
ASTM Standard F2063-18, “Standard specification for wrought nickel-titanium shape memory alloys for medical devices and surgical implants,” ASTM International, West Conshohocken, PA, 2018. https://doi.org/10.1520/F2063-18
ASTM Standard F2129-19a, “Standard test method for conducting cyclic potentiodynamic polarization measurements to determine the corrosion susceptibility of small implant devices,” ASTM International, West Conshohocken, PA, 2019. https://doi.org/10.1520/F2129-19A
Calculator for pH buffers [Internet] (2019) Cent. Proteome Res. Liverp. Accessed 7 Nov, 2019. http://www.liverpool.ac.uk/cpr/Research/Tools/BuffferCalc/Buffer.html
ASTM Standard F3306-19, “Standard Test Method for Ion Release Evaluation of Medical Implants,” ASTM International, West Conshohocken, PA, 2019. https://doi.org/10.1520/F3306-19
Eiselstein LE, Steffey D, Nissan A, Corlett N, Dugnani R, Kus E et al (2009) Acceptance criteria for corrosion resistance of medical devices: statistical analysis of nitinol pitting in in vivo environments. J Mater Eng Perform 18:768–780
Nagaraja S, Di Prima M, Saylor D, Takai E (2016) Current practices in corrosion, surface characterization, and nickel leach testing of cardiovascular metallic implants: cardiovascular metallic implants FDA workshop. J Biomed Mater Res B Appl Biomater. https://doi.org/10.1002/jbm.b.33630
Saylor DM, Craven BA, Chandrasekar V, Simon DD, Brown RP, Sussman EM (2018) Predicting patient exposure to nickel released from cardiovascular devices using multi-scale modeling. Acta Biomater 70:304–314
Wataha JC, O’Dell NL, Singh BB, Ghazi M, Whitford GM, Lockwood PE (2001) Relating nickel-induced tissue inflammation to nickel release in vivo. J Biomed Mater Res 58:537–544
Nickel [Internet] (2020) Greenwood Village, Colorado, USA: IBM Watson Health. https://www.micromedexsolutions.com/micromedex2/librarian/CS/CC19BB/ND_PR/evidencexpert/ND_P/evidencexpert/DUPLICATIONSHIELDSYNC/6C9CCC/ND_PG/evidencexpert/ND_B/evidencexpert/ND_AppProduct/evidencexpert/ND_T/evidencexpert/PFActionId/evidencexpert.IntermediateToDocumentLink?docId=341&contentSetId=134&title=NICKEL&servicesTitle=NICKEL#close
Shabalovskaya S, Ryhänen J, Yahia L (2002) Bioperformance of nitinol: surface tendencies [Internet]. Mater Sci Forum. https://www.scientific.net/MSF.394-395.131. Accessed 16 Nov 2019
Nasakina EO, Sevost’yanov MA, Gol’dberg MA, Demin KY, Baikin AS, Goncharenko BA et al (2015) Long-term corrosion tests of nanostructural nitinol of (55.91 wt % Ni, 44.03 wt % Ti) composition under static conditions: Ion release. Inorg Mater Appl Res 6:59–66
Capoşi M, Prodana M, Ioniţă D (2011) Effect of temperature and pH on the metal release from TiNi. Sci Bull 73:27–36
Pound BG (2010) Corrosion behavior of nitinol in blood serum and PBS containing amino acids. J Biomed Mater Res B Appl Biomater 94B:287–295
Shabalovskaya SA, Anderegg JW, Undisz A, Rettenmayr M, Rondelli GC (2012) Corrosion resistance, chemistry, and mechanical aspects of Nitinol surfaces formed in hydrogen peroxide solutions. J Biomed Mater Res B Appl Biomater 100B:1490–1499
Weaver JD, Gutierrez EJ, Nagaraja S, Stafford PR, Sivan S, Di Prima M (2017) Sodium hypochlorite treatment and nitinol performance for medical devices. J Mater Eng Perform 26:4245–4254
Yokoyama K, Kaneko K, Yabuta E, Asaoka K, Sakai J (2004) Fracture of nickel–titanium superelastic alloy in sodium hypochlorite solution. Mater Sci Eng A 369:43–48
Sullivan SJL, Madamba D, Sivan S, Miyashiro K, Dreher ML, Trépanier C et al (2017) The effects of surface processing on in-vivo corrosion of Nitinol stents in a porcine model. Acta Biomater 62:385–396
Nagaraja S, Chandrasekar V, Ormonde D, Hickey H, Lipschultz K, Chao C et al (2018) The impact of fatigue testing and surface processing on nickel release in nitinol stents. Shape Mem Superelasticity 4:462–471
Sullivan SJL, Dreher ML, Zheng J, Chen L, Madamba D, Miyashiro K et al (2015) Effects of oxide layer composition and radial compression on nickel release in nitinol stents. Shape Mem Superelasticity. 1:311–327
Clarke B, Carroll W, Rochev Y, Hynes M, Bradley D, Plumley D (2006) Influence of Nitinol wire surface treatment on oxide thickness and composition and its subsequent effect on corrosion resistance and nickel ion release. J Biomed Mater Res A 79A:61–70
Taira M, Toguchi MS, Hamada Y, Takahashi J, Itou R, Toyosawa S et al (2001) Studies on cytotoxic effect of nickel ions on three cultured fibroblasts. J Mater Sci Mater Med 12:373–376
Eliades T, Pratsinis H, Kletsas D, Eliades G, Makou M (2004) Characterization and cytotoxicity of ions released from stainless steel and nickel-titanium orthodontic alloys. Am J Orthod Dentofacial Orthop 125:24–29
Shih C-C, Lin S-J, Chen Y-L, Su Y-Y, Lai S-T, Wu GJ et al (2000) The cytotoxicity of corrosion products of nitinol stent wire on cultured smooth muscle cells. J Biomed Mater Res 52:395–403
Ryhänen J, Niemi E, Serlo W, Niemelä E, Sandvik P, Pernu H et al (1997) Biocompatibility of nickel-titanium shape memory metal and its corrosion behavior in human cell cultures. J Biomed Mater Res 35:451–457
Stohs SJ, Bagchi D (1995) Oxidative mechanisms in the toxicity of metal ions. Free Radic Biol Med 18:321–336
Gilbert JL, Sivan S, Liu Y, Kocagöz SB, Arnholt CM, Kurtz SM (2015) Direct in vivo inflammatory cell-induced corrosion of CoCrMo alloy orthopedic implant surfaces. J Biomed Mater Res A 103:211–223
Bochi GV, Torbitz VD, Santos RCV, Cubillos-Rojas M, López JLR, Siebel AM et al (2016) Fenton reaction-generated advanced oxidation protein products induces inflammation in human embryonic kidney cells. Inflammation 39:1285–1290
Das TK, Wati MR, Fatima-Shad K (2015) Oxidative stress gated by Fenton and Haber Weiss reactions and its association with Alzheimer’s disease. Arch Neurosci [Internet]. 2015. http://archneurosci.com/en/articles/60038.html. Accessed 18 Nov, 2019
Kanemura T, Yokoyama K, Sakai J (2008) Effects of acid type on corrosion and fracture behavior of Ni–Ti superelastic alloy under sustained tensile load in physiological saline solution containing hydrogen peroxide. Corros Sci 50:2785–2795
Freiberg KE, Bremer-Streck S, Kiehntopf M, Rettenmayr M, Undisz A (2014) Effect of thermomechanical pre-treatment on short- and long-term Ni release from biomedical NiTi. Acta Biomater 10:2290–2295
Acknowledgements
Funding for this work was provided by the U.S. Food and Drug Administration Center for Devices and Radiological Health. The project was supported by appointments of authors (H.S., P.A.T.) to the Research Participation Program administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and the U.S. Food and Drug Administration. The authors would like to thank Dr. Katherine Vorvolakos for review of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Eric M. Sussman and Huiyu Shi have contributed equally to this work.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This invited article is part of a special topical focus in the journal Shape Memory and Superelasticity on Cardiovascular Nitinol Medical Devices. The issue was organized by Dr. Srinidhi Nagaraja, G.RAU, Inc. and Dr. Harshad M. Paranjape, Confluent Medical Technologies, Inc.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sussman, E.M., Shi, H., Turner, P.A. et al. Nitinol Release of Nickel under Physiological Conditions: Effects of Surface Oxide, pH, Hydrogen Peroxide, and Sodium Hypochlorite. Shap. Mem. Superelasticity 8, 98–106 (2022). https://doi.org/10.1007/s40830-022-00364-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40830-022-00364-3