Abstract
Background
Myocarditis and pericarditis have been associated most notably with mRNA vaccines, but the association with a recently authorized adjuvated vaccine (NVX-CoV2373) is controversial.
Objective
The aim was to analyze the cases of myocarditis and pericarditis in association with NVX-CoV2373 reported to the World Health Organization (WHO) global database of individual case safety reports (ICSRs) for drug monitoring (VigiBase), applying disproportionality analyses.
Patients and methods
The main characteristics of the ICSRs reporting myopericarditis with NVX-CoV2373 have been summarized. Reporting odds ratios (RORs) as a measure of disproportionality for reported myopericarditis (November 1967–August 2022) have been calculated for NVX-CoV2373; mRNA and adenoviral vector-based vaccines were also included as a reference.
Results
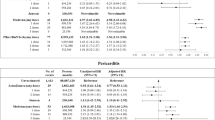
In total, 61 ICSRs included NVX-CoV2373. Most of the reports originated in Australia (50; 82.0%); 24 (39.3%) were considered serious. None of them were fatal. The median age of individuals was 35.5 years old, and most were males (38; 62.3%). Chest pain was the most common co-reported event 43 (70.5%). The median induction period was 3 days after immunization. Increased disproportionality for myopericarditis was found for NVX-CoV2373 (ROR 14.47, 95% confidence interval [CI] 11.22–18.67) and mRNA vaccines: BNT162b2 (ROR 17.15, 95% CI 16.88–17.42) and mRNA-1273 (ROR 6.92, 95% CI 6.77–7.08). Higher values were found in males. The adenoviral vector-based vaccine Ad26.COV2.S showed slightly increased disproportionality (ROR 1.83, 95% CI 1.70–1.98), whereas no increased disproportionality was found for ChAdOx1.
Conclusions
NVX-CoV2373 vaccine showed a similar increased disproportionality as mRNA vaccines. More evidence from controlled studies is necessary; however, a precautionary approach is warranted. Healthcare professionals should be aware of the potential occurrence of myopericarditis with this new vaccine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Data from the World Health Organization (WHO) Program for International Drug Monitoring database (VigiBase) were examined to calculate reporting odds ratios (RORs) for reporting of myopericarditis with NVX-CoV2373 vaccine, relative to other vaccines and drugs. |
NVX-CoV2373 and mRNA vaccines were associated with significantly elevated RORs for myopericarditis and higher values for males. |
Healthcare professionals should be aware of the potential occurrence of myopericarditis associated with this vaccine. |
1 Introduction
The NVX-CoV2373 coronavirus disease 2019 (COVID-19) vaccine (Novavax) is a new adjuvated protein-based vaccine combining the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike protein with Matrix-M adjuvant, recently authorized for emergency use by the Food and Drug Administration (FDA), to prevent COVID-19 in individuals 12 years of age and older [1]. The vaccine was previously authorized in Australia, Canada, UK and the European Union [2].
Due to clinical trial evidence, the FDA issued a warning for increased risks of myocarditis and pericarditis, which was included in the Fact Sheet for Healthcare Providers [3]. Conversely, no warning nor any mention of the risk of myocarditis or pericarditis is available in the Summary of Product Characteristics (SmPC) issued by the European Medicines Agency (EMA) [4]. Myocarditis and pericarditis were early signals associated with mRNA vaccines that emerged in Israel on 2021 [5, 6]. Since then, the causality evidence has accumulated, and both mRNA vaccines, BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna), have listed these events in their product label.
Misalignment of regulatory decisions between regulatory agencies may suggest the presence of conflicting evidence. The aim of the present study was to describe and analyze the cases of myocarditis and pericarditis with COVID-19 vaccines reported to the World Health Organization (WHO) global database of individual case safety reports (ICSRs) applying disproportionality analysis.
2 Methods
We searched in the WHO global database of ICSRs (VigiBase) for ICSRs from inception on November 14, 1967, to August 23, 2022. VigiBase is maintained and developed on behalf of the WHO by the Uppsala Monitoring Centre (UMC), situated in Uppsala, Sweden (https://www.who-umc.org/). We utilized a de-duplicated dataset version of VigiBase including 31,703,998 ICSRs (database version 28/8/2022). The ICSRs were accessed using the VigiLyze tool.
The following COVID-19 vaccines of interest were considered in the searches: NVX-CoV2373 (COVID-19 vaccine prot. subunit [NVX CoV 2373]), Pfizer-BioNTech (Tozinameran; active ingredient variant), Moderna (COVID-19 vaccine mRNA; mRNA 1273), Ad26.COV2.S (COVID-19 vaccine NRVV Ad26 [JNJ 78436735]) and AstraZeneca (COVID-19 vaccine NRVV Ad [ChAdOx1 nCoV-19]). The main adverse reaction of interest was myopericarditis and included the following preferred terms of the Medical Dictionary for Regulatory Activities (MedDRA) Terminology (version 25.0; http://www.meddra.org/): “myocarditis” and/or “pericarditis” and/or “myopericarditis.” Myopericarditis or the combined outcome “myocarditis or pericarditis” have been used in previous studies [7] and in reports by regulatory agencies and health authorities [8, 9]. Secondarily, we also explore disproportionality for the preferred terms “myocarditis” and “pericarditis” separately.
ICSRs were described in terms of source of report, patient age, gender, seriousness according to the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) Harmonized Tripartite Guideline on clinical safety regarding definitions and standards for expedited reporting (E2A) [10], and outcome (recovery, fatality). The induction period was calculated (when available) as the time between the start of the drug treatment and the clinical diagnosis of pericarditis and myocarditis in the ICSRs. Co-reported drugs and vaccines were described.
Disproportionality analysis was performed using a case–non-case approach through the calculation of the reporting odds ratio (ROR) and the 95% confidence interval (CI) using Woolf’s method [11]. ROR values > 1.0 indicate a higher than expected reporting rate, but do not necessarily mean differences in the risk probability for the adverse reaction [12, 13].
mRNA vaccines served as a positive control for the increased disproportionality of the event since they have been described as causal regarding myopericarditis risk, whereas adenoviral vector-based vaccines ChAdOx1 and Ad26.COV2.S were also included as a reference since they have been also associated with myopericarditis reports, but a definite association has not been established at the moment [14].
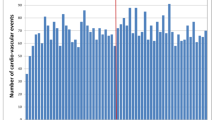
To test the consistency of the disproportionality, we performed sensitivity analysis according to the origin of the reports (country/region), according to the period from first to last report received of myopericarditis with NVX-CoV2373, considering ICSRs reported with vaccines only (Anatomical Therapeutic Chemical [ATC] classification group: J07) and according to the dataset type (de-duplicated dataset and non–de-duplicated dataset). All analyses were conducted using Stata version 17.0 MP (Stata- Corp LP, College Station, Texas, USA).
3 Results
Following our search, 61,812 ICSRs of myopericarditis were found. From these, 61 ICSRs included the NVX-CoV2373 vaccine; 45 (73.8%) reported pericarditis, 11 (18.0%) myocarditis, four (6.6%) myopericarditis and one (1.6%) both terms (myocarditis and pericarditis) (Table 1). For nine ICSRs (14.8%), there was more than one suspected COVID-19 vaccine (i.e., heterologous vaccination regimens including NVX-CoV2373 and other suspected COVID-19 vaccines): five (55.6%) indicated mRNA-1273 vaccine (Moderna) and four (44.4%) BNT162b2 vaccine (Pfizer-BioNTech). In four cases, NVX-CoV2373 was utilized as a booster: two were administered after mRNA-1273 and two after BNT162b2. Only three ICSRs (4.9%) mentioned concomitant medication (other than vaccines): tranexamic acid, cannabidiol and flecainide. Twenty-four reports (39.3%) were considered serious: 19 caused/prolonged hospitalization, three were life-threatening, one was disabling/incapacitating and 11 were considered to pose other medically important conditions (note that the same report can be reported with more than one seriousness criterion). None of them were fatal. Of the 32 ICSRs with available information on outcome, at the time of the study, 20 persons had failed to recover from the adverse reaction, eight were recovering and only four had recovered (one of them with sequelae). The median induction period for myopericarditis from vaccination (after the most recent immunization) estimated from 40 ICSRs was 3 days (interquartile range [IQR] 1–11). Most of the reports originated in Australia (50; 82.0%), followed by European countries: Germany (6; 9.8%), France (2; 3.3%) and Italy (1; 1.6%). Two ICSRs originated in the United States (US) (2; 3.3%) (Table 1).
The median age of the patients was 35.5 years old (IQR 28–47). Most of the reports involved males (38; 62.3%). The ICSRs included a median of five adverse reactions (IQR 2–9); ten ICSRs reported exclusively myopericarditis. "Chest pain" and "chest discomfort" were common co-reported adverse events (43 [70.5%] and nine [14.8%], respectively), followed by heart rate and rhythm anomalies (palpitations [14; 23.0%] and tachycardia [7; 11.5%]), dyspnea (15; 24.6%), arthralgia (11; 18.0%), dizziness (10; 16.4%) and lethargy (10; 16.4%). A complete list of co-reported events is available in the “Supplementary Appendix” (see the electronic supplementary material).
Overall, an increased disproportionality for myopericarditis was found for the NVX-CoV2373 vaccine (ROR 14.47, 95% CI 11.22–18.67) and the mRNA vaccines: BNT162b2 (ROR 17.15, 95% CI 16.88–17.42) and mRNA-1273 (ROR 6.92, 95% CI 6.77–7.08). No increased disproportionality was found for the adenoviral vector-based vaccine ChAdOx1 (ROR 0.80, 95% CI 0.76–0.85) (Table 2). Ad26.COV2.S registered increased disproportionality with a lesser magnitude than mRNA vaccines and NVX-CoV2373. Consistent results were found in males and females, with the highest disproportionality values for Pfizer-BioNTech and NVX-CoV2373 vaccines (Table 3). Disproportionality for the NVX-CoV2373 vaccine was found in the age groups 18–44 and 45–65 in both sexes, but with higher values in males (Table 4). Disproportionality was found also for the preferred terms “myocarditis” and “pericarditis” considered individually (Table 1). Similar results were found in sensitivity analysis when restricting the database to vaccine-only reports, restricting the study period to the reporting period of myopericarditis with NVX-CoV2373 vaccine, or when excluding data from Australia (the country that provided more reports of interest), USA or European countries. However, when restricting the analyses to ICSRs reporting vaccines only, the NVX-CoV2373 and mRNA vaccines remained with a statistically significant increased disproportionality (Supplementary Appendix).
4 Discussion
In this global database of ICSRs including more than 33 million reports, an increased disproportionality signal was found for NVX-CoV2373 vaccine in line with the mRNA vaccines, and the Pfizer-BioNTech vaccine in particular. The signal was consistent when taking into account sex and age. The increased disproportionality remained statistically significant in the sensitivity analysis after excluding Australian data, which made up most of the reports. The disproportionality was slightly more elevated in males and consistent across different analyses.
Myocarditis after immunization has been described with live vaccinia virus vaccines [15] and more recently also with the COVID-19 vaccines [16, 17]. Among COVID-19 vaccinations, the highest incidence of myopericarditis has been observed with mRNA vaccines [7]. Evidence of risk from controlled studies for non–mRNA vaccines is scarce, although a self-controlled case series found excess risk of myopericarditis (and not pericarditis) after the first dose of ChAdOx1 vaccine [18, 19]. However, major evidence of a risk association comes predominantly from studies with mRNA vaccines. In a hospital-based case–control study performed in France, an increased risk of myocarditis associated with BNT162b2 and mRNA-1273 vaccines was identified in the week after immunization (first or second dose); moreover, an increased risk of pericarditis was identified in the week after the second dose [20]. Another large cohort study, including 23 million participants from four Nordic countries, found a higher risk of myopericarditis associated with BNT162b2 and mRNA-1273 vaccines, showing an incident risk ratio (IRR) of 6.57 and 1.75, respectively [21]. Recently, a retrospective cohort study using claims databases in the US found an increased risk of myopericarditis after COVID-19 mRNA vaccination, with IRRs of 1.71 and 2.17 after the second dose for BNT162b2 and mRNA-1273, respectively. No statistically significant risk differences regarding myopericarditis among the two mRNA vaccines were found [22]. Consistent with the previous studies, we found both mRNA vaccines associated with a high disproportionality for myopericarditis. On the other hand, the induction period after immunization with NVX-CoV2373 was 3 days, similar to the mRNA-induced myocarditis, which occurred in the first days after the most recent immunization [23].
The pivotal randomized clinicals trials with the NVX-CoV2373 vaccine included North American and British populations [24, 25]. Two cases of myocarditis were identified in 30,058 vaccinated individuals and one case among 19,982 who received placebo [26], which would account for a non-statistically significant increase of myocarditis risk (relative risk 1.33, 95% CI 0.12–14.66). Moreover, during the extensions of the clinical trials, three additional cases of myocarditis were identified in immunized patients. This evidence was differently interpreted. The FDA considered a precautionary approach and assumed the risk to be certain since no cases of myocarditis were detected in any of the mRNA vaccine trials [27]. On the other hand, the EMA did not consider myocarditis as an “identified risk” since the incidence of myocarditis of three cases per 14,513 person-years would not be higher than the baseline risk of myocarditis in the general population (background rate) estimated at 1.6-4.6 per 14,513 person-years from European data (EU-Access study) [26]. However, caution should be taken when using background rates from different populations to rule out vaccine risks since there is considerable heterogeneity between geographies and databases that can lead to unreliable inferences [28].
The mechanism of action for vaccine-induced myopericarditis remains to be elucidated. It has been observed that vaccines triggering an intense immune response such as mRNA vaccines could be associated with a higher risk of myocarditis [21]. Several mechanisms affected by the immune–genetic background, age and sex have been hypothesized to explain the risk of myocarditis with mRNA vaccines. First, it could be due to mRNA immune reactivity; second, the Spike protein antigen could induce a cross-reaction of SARS-CoV-2 spike glycoproteins with myocardial contractile proteins; and, lastly, hyperimmunity could burst due to hormone-related factors contributing to the sex-specific differences observed in both COVID-19 mRNA vaccines (more risk in young males) [29, 30]. The mRNA vaccines use a lipid nanoparticle component that encapsulates the mRNA strand encoding the S-protein sequence and which may confer immune reactivity. Interestingly, the NVX-CoV2373 also uses a nanoparticle delivery vehicle to assemble in S-proteins. On the contrary, no nanoparticles are used in the adenoviral vector-based vaccines ChAdOx1 and Ad26.COV2.S [31]. More research would be needed to understand the role of nanoparticles in the potential risk of vaccine-induced myocarditis. The highest disproportionality values were observed in males. The reason for the male predominance in myopericarditis is unknown. Testosterone is thought to play a role, via a combined mechanism of inhibition of anti-inflammatory cells and enhancement of a T helper type 1 (Th1) immune response, whereas estrogen has inhibitory effects on proinflammatory T cells, with a decrease in cell-mediated immune responses [32]. A higher disproportionality was found in older women; in this regard, it has been described that postmenopausal women show a higher incidence of pericarditis [33]. No evidence towards an increased disproportionality trend was found for younger ages with NVX-CoV2373. Caution should be taken with this observation since the lack of reports in non-adults made impossible a complete analysis on younger ages.
Although an important proportion of the cases were life-threatening, none of them were fatal. Other reported cases for mRNA vaccines have shown a low fatality rate [14]. It is worth to note that at least one-third of the cases were reversible and that a greater risk of hospitalization and death has been observed in association with COVID-19 infection than with COVID-19 vaccination [18, 19].
4.1 Limitations
Our study also has several limitations. The data source for this study is a spontaneous report database from which no definitive causation associations can be drawn. There are other inherent limitations of the passive pharmacovigilance systems, such as a lack of denominators and underreporting, which have been described elsewhere [34]. On the other hand, the capacity to identify potential disproportionality signals is also increased in a global pharmacovigilance database over smaller national databases [35]. Moreover, the possibility of duplicate reporting cannot be ruled out; nevertheless, we used a de-duplicated dataset version to minimize this potential bias. Some patients did not recover from the adverse reaction, and at the moment of the study realization, we did not have latter updates regarding follow-up of outcomes, and this might have led to outcomes not being identified (i.e., recoveries and fatalities). Although common symptoms of myopericarditis such as chest pain were often co-reported, other relevant information such as viral testing for myocarditis was lacking from the reports. On the other hand, myocarditis events may have been missed because of inaccuracies in the coding of the events or diagnostic misclassification. In addition, potential bias can also occur, such as notoriety bias due to the media attention that myocarditis has attained. However, the consistency of the disproportionality was evaluated through different sensitivity analyses.
5 Conclusions
In conclusion, myopericarditis associated with COVID-19 vaccines seem to be an adverse reaction of a different frequency according to the type of vaccine. The new NVX-CoV2373 vaccine shows an increased disproportionality for myopericarditis similar to mRNA vaccines. More evidence from controlled studies is necessary; however, a precautionary approach is warranted. Healthcare professionals should be aware of the potential occurrence of myopericarditis with this new vaccine.
References
Food and Drug Administration (FDA). Coronavirus (COVID-19) Update: FDA Authorizes Emergency Use of NVX-CoV2373 COVID-19 Vaccine, Adjuvanted; 2022. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-emergency-use-NVX-CoV2373-covid-19-vaccine-adjuvanted. Accessed 8 Jan 2023.
Pan American Health Organization (PAHO). Pharmacovigilance for COVID-19 Vaccines Dashboard. https://covid-19pharmacovigilance.paho.org/novavax-serum-institute-of-india-sii#APPROVAL Accessed 8 Jan 2023.
Food and Drug Administration (FDA). Fact sheet for healthcare providers administering vaccine (vaccination providers). Emergency use authorization (EUA) of the NVX-CoV2373 COVID-19 vaccine, adjuvanted to prevent coronavirus disease (COVID-19). https://www.fda.gov/media/159897/download. Accessed 25 Aug 2022.
European Medicines Agency (EMA). Summary of Product Characteristics, (SmPC); 2022 https://www.ema.europa.eu/en/documents/product-information/nuvaxovid-epar-product-information_en.pdf. Accessed 8 Jan 2023.
Mevorach D, Anis E, Cedar N, Bromberg M, Haas EJ, Nadir E, Olsha-Castell S, Arad D, Hasin T, Levi N, Asleh R, Amir O, Meir K, Cohen D, Dichtiar R, Novick D, Hershkovitz Y, Dagan R, Leitersdorf I, Ben-Ami R, Miskin I, Saliba W, Muhsen K, Levi Y, Green MS, Keinan-Boker L, Alroy-Preis S. Myocarditis after BNT162b2 mRNA vaccine against Covid-19 in Israel. N Engl J Med. 2021;385(23):2140–9.
Witberg G, Barda N, Hoss S, Richter I, Wiessman M, Aviv Y, Grinberg T, Auster O, Dagan N, Balicer RD, Kornowski R. Myocarditis after Covid-19 vaccination in a large health care organization. N Engl J Med. 2021;385(23):2132–9.
Ling RR, Ramanathan K, Tan FL, Tai BC, Somani J, Fisher D, MacLaren G. Myopericarditis following COVID-19 vaccination and non-COVID-19 vaccination: a systematic review and meta-analysis. Lancet Respir Med. 2022;10(7):679–88.
European Medicines Agency (EMA). Signal assessment report on myocarditis and pericarditis with Spikevax - COVID-19 mRNA vaccine (nucleoside-modified). Published online December 2nd ,2021. https://www.ema.europa.eu/en/documents/prac-recommendation/signal-assessment-report-myocarditis-pericarditis-spikevax-previously-covid-19-vaccine-moderna-covid_en.pdf Accessed 8 Jan 2023.
Centers for Disease Control and Prevention Advisory Committee on Immunization Practices meeting. Myopericarditis following COVID-19 vaccination: updates from the Vaccine Adverse Event Reporting System (VAERS). October 21, 2021.Accessed March 10, 2022. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-10-20-21/07-COVID-Su-508.pdf Accessed 8 Jan 2023.
ICH Harmonised Tripartite Guideline. Clinical safety data management: definitions and standards for expedited reporting. E2A. January 4th. 2022. https://database.ich.org/sites/default/files/E2A_Guideline.pdf. Accessed 8 Jan 2023.
Wang W, Lu S, Xie T. Optimal confidence intervals for the relative risk and odds ratio. Stat Med. 2023;42(3):281–96.
Rothman KJ, Lanes S, Sacks ST. The reporting odds ratio and its advantages over the proportional reporting ratio. Pharmacoepidemiol Drug Saf. 2004;13(8):519–23.
Uchikawa M, Hashiguchi M, Shiga T. Drug-induced QT prolongation and torsade de pointes in spontaneous adverse event reporting: a retrospective analysis using the japanese adverse drug event report database (2004–2021). Drugs Real World Outcomes. 2022;9(4):551–9.
Lane S, Yeomans A, Shakir S. Reports of myocarditis and pericarditis following mRNA COVID-19 vaccination: a systematic review of spontaneously reported data from the UK, Europe and the USA and of the scientific literature. BMJ Open. 2022;12(5): e059223.
Mei R, Raschi E, Forcesi E, Diemberger I, De Ponti F, Poluzzi E. Myocarditis and pericarditis after immunization: Gaining insights through the Vaccine Adverse Event Reporting System. Int J Cardiol. 2018;273:183–6.
Keshavarz P, Yazdanpanah F, Emad M, Hajati A, Nejati SF, Ebrahimian Sadabad F, Azrumelashvili T, Mizandari M, Raman SS. Myocarditis Following COVID-19 Vaccination: Cardiac Imaging Findings in 118 Studies. Tomography. 2022;8(4):1959–73. https://doi.org/10.3390/tomography8040164. (PMID: 36006062; PMCID: PMC9416085).
Singh R, Chakrabarti SS, Gambhir IS, Verma A, Kumar I, Ghosh S, Tiwari A, Chandan G, Chakrabarti S, Kaur U. Acute cardiac events after ChAdOx1 nCoV-19 corona virus vaccine: report of three cases. Am J Ther. 2022;29(5):e579–85.
Patone M, Mei XW, Handunnetthi L, Dixon S, Zaccardi F, Shankar-Hari M, Watkinson P, Khunti K, Harnden A, Coupland CAC, Channon KM, Mills NL, Sheikh A, Hippisley-Cox J. Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection. Nat Med. 2022;28(2):410–22.
Patone M, Mei XW, Handunnetthi L, Dixon S, Zaccardi F, Shankar-Hari M, Watkinson P, Khunti K, Harnden A, Coupland CAC, Channon KM, Mills NL, Sheikh A, Hippisley-Cox J. Risk of myocarditis after sequential doses of COVID-19 vaccine and SARS-CoV-2 infection by age and sex. Circulation. 2022;146(10):743–54.
Stéphane Le Vu, Marion Bertrand, Marie-Joëlle Jabagi, Jérémie Botton, Jérôme Drouin, Bérangère Baricault, Kim Bouillon, Laura Semenzato, Alain Weill, Rosemary Dray-Spira, Mahmoud Zureik. Association entre les vaccins COVID-19 à ARN messager et la survenue de myocardite et péricardite chez les personnes de 12 à 50 ans en France. Etude à partir des données du Système National des Données de Santé (SNDS), 2021. https://ansm.sante.fr/uploads/2021/11/08/20211108-covid-19-vaccins-rapport-epiphare-myocardite-pericardite.pdf Accessed 8 Jan 2023.
Karlstad Ø, Hovi P, Husby A, Härkänen T, Selmer RM, Pihlström N, Hansen JV, Nohynek H, Gunnes N, Sundström A, Wohlfahrt J, Nieminen TA, Grünewald M, Gulseth HL, Hviid A, Ljung R. SARS-CoV-2 Vaccination and Myocarditis in a Nordic Cohort Study of 23 Million Residents. JAMA Cardiol. 2022;7(6):600–12.
Husby A, Hansen JV, Fosbøl E, et al. SARS-CoV-2 vaccination and myocarditis or myopericarditis: population based cohort study. BMJ. 2021;375: e068665.
Diaz GA, Parsons GT, Gering SK, Meier AR, Hutchinson IV, Robicsek A. Myocarditis and pericarditis after vaccination for COVID-19. JAMA. 2021;326(12):1210–2.
Heath PT, Galiza EP, Baxter DN, Boffito M, Browne D, Burns F, Chadwick DR, Clark R, Cosgrove C, Galloway J, Goodman AL, Heer A, Higham A, Iyengar S, Jamal A, Jeanes C, Kalra PA, Kyriakidou C, McAuley DF, Meyrick A, Minassian AM, Minton J, Moore P, Munsoor I, Nicholls H, Osanlou O, Packham J, Pretswell CH, San Francisco Ramos A, Saralaya D, Sheridan RP, Smith R, Soiza RL, Swift PA, Thomson EC, Turner J, Viljoen ME, Albert G, Cho I, Dubovsky F, Glenn G, Rivers J, Robertson A, Smith K, Toback S, 2019nCoV-302 Study Group. Safety and efficacy of NVX-CoV2373 Covid-19 vaccine. N Engl J Med. 2021;385(13):1172–83.
Dunkle LM, Kotloff KL, Gay CL, Áñez G, Adelglass JM, Barrat Hernández AQ, Harper WL, Duncanson DM, McArthur MA, Florescu DF, McClelland RS, Garcia-Fragoso V, Riesenberg RA, Musante DB, Fried DL, Safirstein BE, McKenzie M, Jeanfreau RJ, Kingsley JK, Henderson JA, Lane DC, Ruíz-Palacios GM, Corey L, Neuzil KM, Coombs RW, Greninger AL, Hutter J, Ake JA, Smith K, Woo W, Cho I, Glenn GM, Dubovsky F, 2019nCoV-301 Study Group. Efficacy and safety of NVX-CoV2373 in adults in the United States and Mexico. N Engl J Med. 2022;386(6):531–43. https://doi.org/10.1056/NEJMoa2116185. (Epub 2021 Dec 15. PMID: 34910859; PMCID: PMC8693692).
European Medicines Agency (EMA). EU RISK MANAGEMENT PLAN NUVAXOVID (COVID-19 VACCINE (RECOMBINANT, ADJUVANTED)) https://www.ema.europa.eu/en/documents/rmp-summary/nuvaxovid-epar-risk-management-plan_en.pdf Accessed 25 Aug 2022.
Food and Drug Administration (FDA). FDA Briefing Document Novavax COVID-19 Vaccine. Vaccines and Related Biological Products Advisory Committee Meeting June 7, 2022 https://www.fda.gov/media/158912/download Accessed 25 Aug 2022.
Li X, Ostropolets A, Makadia R, Shoaibi A, Rao G, Sena AG, Martinez-Hernandez E, Delmestri A, Verhamme K, Rijnbeek PR, Duarte-Salles T, Suchard MA, Ryan PB, Hripcsak G, Prieto-Alhambra D. Characterising the background incidence rates of adverse events of special interest for covid-19 vaccines in eight countries: multinational network cohort study. BMJ. 2021;373: n1435.
Vojdani A, Kharrazian D. Potential antigenic cross-reactivity between SARS-CoV-2 and human tissue with a possible link to an increase in autoimmune diseases. Clin Immunol. 2020;217: 108480.
Heymans S, Cooper LT. Myocarditis after COVID-19 mRNA vaccination: clinical observations and potential mechanisms. Nat Rev Cardiol. 2022;19(2):75–7.
Tsilingiris D, Vallianou NG, Karampela I, Liu J, Dalamaga M. Potential implications of lipid nanoparticles in the pathogenesis of myocarditis associated with the use of mRNA vaccines against SARS-CoV-2. Metabol Open. 2022;13: 100159.
Bozkurt B, Kamat I, Hotez PJ. Myocarditis With COVID-19 mRNA Vaccines. Circulation. 2021;144(6):471–84.
Kytö V, Sipilä J, Rautava P. Clinical profile and influences on outcomes in patients hospitalized for acute pericarditis. Circulation. 2014;130:1601–6.
Goldman SA. Limitations and strengths of spontaneous reports data. Clin Ther. 1998;20 Suppl C:C40–4.
Caster O, Aoki Y, Gattepaille LM, Grundmark B. Disproportionality analysis for pharmacovigilance signal detection in small databases or subsets: recommendations for limiting false-positive associations. Drug Saf. 2020;43(5):479–87.
Acknowledgements
We thank the Uppsala Monitoring Centre (UMC; Uppsala, Sweden) and the Pan American Network of Pharmacovigilance for their valuable support. We also thank Dr. Salvador Alvarado from the UMC for the helpful suggestions and comments on sensitivity analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
CIBERSAM, Valencia, Spain provided the necessary funds for the publication of this research.
Conflict of interest
The authors declare that they have no conflict of interest. The opinions expressed in this article are those of the authors and do not necessarily reflect the views of the Pan American Health Organization (PAHO), its Board of Directors or the countries they represent.
Ethics approval
Information on all cases gathered from the VigiBase database of individual case safety reports is deidentified, and ethical approval is not needed.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
The dataset used in this study is publicly available at the following URL: https://osf.io/g958w/?view_only=1994d666ab7c4a09a0d413dbdfd18cc0.
Code availability
Not applicable.
Author contributions
DMS and JLC conceived and designed the study. DMS and JFM investigated and analyzed the data. DMS and MTI drafted the manuscript. RT and JFM reviewed the manuscript and supervised the work. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Macías Saint-Gerons, D., Ibarz, M.T., Castro, J.L. et al. Myopericarditis Associated with the Novavax COVID-19 Vaccine (NVX-CoV2373): A Retrospective Analysis of Individual Case Safety Reports from VigiBase. Drugs - Real World Outcomes 10, 263–270 (2023). https://doi.org/10.1007/s40801-023-00355-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-023-00355-5