Abstract
Purpose of Review
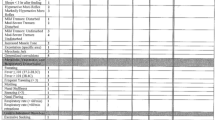
This review summarizes results of recent surveys that quantitate fetal exposure to various drugs and substances, discusses factors that influence transplacental passage of molecules, highlights evidence that speaks to whether certain drugs are teratogenic or affect fetal growth, and outlines the consequences of fetal exposure to alcohol.
Recent Findings
Rates of use of alcohol and tobacco and misuse of prescription drugs and illicit substances are lower in women of child-bearing who are pregnant compared to non-pregnant women, but remain distressingly high. Mental health problems and adverse social determinants of health increase the likelihood that a pregnant woman will also have a co-existing substance use disorder. Legalization of marijuana has resulted in lower societal concern about potential long-term effects of fetal exposure. Reports that opioids, cocaine, amphetamines, and hallucinogens act as teratogens have not withstood scrutiny of larger better-controlled studies. Opioids and alcohol have been associated with reduced fetal somatic and cerebral growth.
Summary
Pregnant women should be advised to abstain from elective use of drugs and substances that can affect the growth of the fetus, neurobehavior of the newborn, and long-term functional potential of the growing child. Of all fetal exposures, alcohol results in the greatest cumulative cognitive deficit across all children and its effects are often silent until children reach school age.

Copyright 2023, Susan Astley Hemingway PhD, University of Washington.
Similar content being viewed by others
Data Availability
Not applicable.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Williams JF, Smith VC. Fetal alcohol spectrum disorders. Pediatrics. 2015;136:e1395–406. This paper presents a comprehensive review of the range of manifestations, diagnosis, neurocognitive and behavioral outcomes, and multidisciplinary approach to FASD. This article also discusses advocacy and public policy implementation to assist children, their families, and the community to address FASD and to curb alcohol consumption during pregnancy.
Patrick SW, Barfield WD, Poindexter BB, Committee On Fetus and Newborn, Committee on Substance Abuse and Prevention. Neonatal opioid withdrawal syndrome. Pediatrics. 2020;146. This clinical report provides an overview of the effect of the opioid crisis on the mother-infant dyad as well as recommendations for management of the infant with opioid exposure, including clinical presentation, assessment, treatment, and discharge.
Hudak ML, Tan RC, Committee On Drugs, Committee On Fetus and Newborn American Academy of Pediatrics. Neonatal drug withdrawal. Pediatrics. 2012;129:e540–60. This clinical guideline set the stage for quality improvement efforts with respect to improving outcomes of newborns with NAS and emphasized that non-pharmacologic care was the essential first element of treatment. This paper also contains guidance on how to wean infants from iatrogenic withdrawal syndromes due to in-hospital use of opioids and benzodiazepines.
Kocherlakota P. Neonatal abstinence syndrome. Pediatrics. 2014;134:e547–61.
McQueen K, Murphy-Oikonen J. Neonatal abstinence syndrome. N Engl J Med. 2016;375:2468–79.
Holbrook BD, Rayburn WF. Teratogenic risks from exposure to illicit drugs. Obstet Gynecol Clin North Am. 2014;41:229–39.
Larson JJ, Graham DL, Singer LT, Beckwith AM, Terplan M, Davis JM, Martinez J and Bada HS. Cognitive and behavioral impact on children exposed to opioids during pregnancy. Pediatrics. 2019;144(2):e20190514. This article provides a summary of an expert panel discussion on substance abuse and mental health that highlights the effects of perinatal opioid exposure on childhood development. Despite the challenges in reporting and statistical analysis, emerging evidence shows that intrauterine opioid exposure is associated with adverse neurocognitive, behavioral, and developmental outcomes.
Benninger KL, Borghese T, Kovalcik JB, et al. Prenatal exposures are associated with worse neurodevelopmental outcomes in infants with neonatal opioid withdrawal syndrome. Front Pediatr. 2020;8:462.
Konijnenberg C. Methodological issues in assessing the impact of prenatal drug exposure. Subst Abuse. 2015;9:39–44. This review discusses several reasons why the effects of prenatal drug exposure are difficult to determine, including variations in dose, timing, duration of exposure, polydrug use, unreliable measures of drug exposure, latent or “sleeper” effects, genetic factors, and socioenvironmental influences.
Flavin J, Paltrow LM. Punishing pregnant drug-using women: defying law, medicine, and common sense. J Addict Dis. 2010;29:231–44.
Angelotta C, Appelbaum PS. Criminal charges for child harm from substance use in pregnancy. J Am Acad Psychiatry Law. 2017;45:193–203.
Chang G. Screening for alcohol and drug use during pregnancy. Obstet Gynecol Clin North Am. 2014;41:205–12.
Committee opinion no. 633: Alcohol abuse and other substance use disorders: ethical issues in obstetric and gynecologic practice. Obstet Gynecol. 2015;125:1529–37.
Burns E, Gray R, Smith LA. Brief screening questionnaires to identify problem drinking during pregnancy: a systematic review. Addiction. 2010;105:601–14.
Yonkers KA, Gotman N, Kershaw T, Forray A, Howell HB, Rounsaville BJ. Screening for prenatal substance use: development of the Substance Use Risk Profile-Pregnancy scale. Obstet Gynecol. 2010;116:827–33.
Chasnoff IJ, Wells AM, McGourty RF, Bailey LK. Validation of the 4P’s Plus screen for substance use in pregnancy validation of the 4P’s Plus. J Perinatol. 2007;27:744–8.
Ostrea EM Jr, Brady M, Gause S, Raymundo AL, Stevens M. Drug screening of newborns by meconium analysis: a large-scale, prospective, epidemiologic study. Pediatrics. 1992;89:107–13.
Palmer KL, Krasowski MD. Alternate matrices: meconium, cord tissue, hair, and oral fluid. Methods Mol Biol. 2019;1872:191–7.
Wennig R. Potential problems with the interpretation of hair analysis results. Forensic Sci Int. 2000;107:5–12.
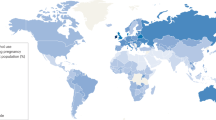
United Nations Office on Drugs and Crime (UNODC) (n.d.). 2022 World Drug Report. Unodc.org. Retrieved February, 2023, from https://www.unodc.org/unodc/data-and-analysis/world-drug-report-2022.html
Substance Abuse and Mental Health Services Administration (SAMHSA) United States Department of Health and Human Services (n.d.). 2020 National Survey on Drug Use and Health (NSDUH): Women. Samhsa.gov. Retrieved February, 2023, from https://www.samhsa.gov/data/sites/default/files/reports/slides-2020-nsduh/2020NSDUHWomenSlides072522.pdf
Substance Abuse and Mental Health Services Administration (SAMHSA) United States Department of Health and Human Services (n.d.). Results from the 2021 National Survey on Drug Use and Health (NSDUH): Graphics from the Key Findings Report. Samhsa.gov. Retrieved July, 2023, from https://www.samhsa.gov/data/sites/default/files/reports/rpt39443/2021_NNR_figure_slides.pdf
Galea S, Vlahov D. Social determinants and the health of drug users: socioeconomic status, homelessness, and incarceration. Public Health Rep. 2002;117(Suppl 1):S135–45.
Gaeta Gazzola M, Carmichael ID, Christian NJ, Zheng X, Madden LM, Barry DT. A national study of homelessness, social determinants of health, and treatment engagement among outpatient medication for opioid use disorder-seeking individuals in the United States. Subst Abus. 2023;44:62–72. Homelessness is an important social determinant of health (SDOH) that affects health outcomes for many medical conditions including opioid use disorder. This study reports that homelessness significantly and negatively affects adherence to treatment for OUD.
Hyer J, Ulrickson C, Yerelian E, Metz TD, Allshouse AA, Hoffman MC. Self-reported alcohol, tobacco, and marijuana use in pregnant women with depressive symptomatology. Am J Perinatol. 2020;37:1223–7.
Brown RA, Dakkak H, Gilliland J, Seabrook JA. Predictors of drug use during pregnancy: The relative effects of socioeconomic, demographic, and mental health risk factors. J Neonatal Perinatal Med. 2019;12:179–87.
Faherty LJ, Matone M, Passarella M, Lorch S. Mental health of mothers of infants with neonatal abstinence syndrome and prenatal opioid exposure. Matern Child Health J. 2018;22:841–8. This study highlights the associations of maternal mental health disorders with OUD and NAS. Depression and anxiety were more prevalent in mothers whose infants were diagnosed with NAS than controls.
Kar P, Tomfohr-Madsen L, Giesbrecht G, Bagshawe M, Lebel C. Alcohol and substance use in pregnancy during the COVID-19 pandemic. Drug Alcohol Depend. 2021;225:108760.
Hall W, Lynskey M. Evaluating the public health impacts of legalizing recreational cannabis use in the United States. Addiction. 2016;111:1764–73.
Martin GI. Marijuana: the effects on pregnancy, the fetus, and the newborn. J Perinatol. 2020;40:1470–6.
Grigsby TM, Hoffmann LM, Moss MJ. Marijuana use and potential implications of marijuana legalization. Pediatr Rev. 2020;41:61–72.
Stewart SB, Bhatia D, Burns EK, et al. Association of marijuana, mental health, and tobacco in Colorado. J Addict Med. 2020;14:48–55.
Guy GP Jr, Zhang K, Bohm MK, et al. Vital Signs: Changes in opioid prescribing in the United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66:697–704.
Patrick SW, Dudley J, Martin PR, et al. Prescription opioid epidemic and infant outcomes. Pediatrics. 2015;135:842–50.
Patrick SW, Schumacher RE, Benneyworth BD, Krans EE, McAllister JM, Davis MM. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000–2009. JAMA. 2012;307:1934–40.
Patrick SW, Faherty LJ, Dick AW, Scott TA, Dudley J, Stein BD. Association among county-level economic factors, clinician supply, metropolitan or rural location, and neonatal abstinence syndrome. JAMA. 2019;321:385–93.
Bada HS, Bann CM, Whitaker TM, et al. Protective factors can mitigate behavior problems after prenatal cocaine and other drug exposures. Pediatrics. 2012;130:e1479–88. This longitudinal study reports on long-term outcomes of children following prenatal cocaine exposure and other drugs compared with a non-exposed cohort. A key finding was that even thoughadverse outcomes are associated with prenatal drug exposure, there are variables at the individual, family, and community level that attenuate the negative impact of drug exposure.
Callaghan T, Crimmins J, Schweitzer RD. Children of substance-using mothers: child health engagement and child protection outcomes. J Paediatr Child Health. 2011;47:223–7.
Hair NL, Hanson JL, Wolfe BL, Pollak SD. Association of child poverty, brain development, and academic achievement. JAMA Pediatr. 2015;169:822–9.
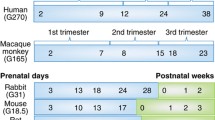
Garland M. Pharmacology of drug transfer across the placenta. Obstet Gynecol Clin North Am. 1998;25:21–42.
Syme MR, Paxton JW, Keelan JA. Drug transfer and metabolism by the human placenta. Clin Pharmacokinet. 2004;43:487–514. This review offers a comprehensive discussion on the placenta’s role in drug metabolism, transfer, and clearance from the mother to the fetus. The placenta provides a link between the circulations of two distinct individuals but also acts as a barrier to protect the fetus from xenobiotics in the maternal blood.
Rasheed A, Hines RN, McCarver-May DG. Variation in induction of human placental CYP2E1: possible role in susceptibility to fetal alcohol syndrome? Toxicol Appl Pharmacol. 1997;144:396–400.
Ostrea EM Jr, Mantaring JB 3rd, Silvestre MA. Drugs that affect the fetus and newborn infant via the placenta or breast milk. Pediatr Clin North Am. 2004;51(539–79):vii.
van Hoogdalem MW, Wexelblatt SL, Akinbi HT, Vinks AA, Mizuno T. A review of pregnancy-induced changes in opioid pharmacokinetics, placental transfer, and fetal exposure: Towards fetomaternal physiologically-based pharmacokinetic modeling to improve the treatment of neonatal opioid withdrawal syndrome. Pharmacol Ther. 2022;234:108045.
Nanovskaya T, Deshmukh S, Brooks M, Ahmed MS. Transplacental transfer and metabolism of buprenorphine. J Pharmacol Exp Ther. 2002;300:26–33.
Giroux M, Teixera MG, Dumas JC, Desprats R, Grandjean H, Houin G. Influence of maternal blood flow on the placental transfer of three opioids–fentanyl, alfentanil, sufentanil. Biol Neonate. 1997;72:133–41.
Koepsell H. Polyspecific organic cation transporters: their functions and interactions with drugs. Trends Pharmacol Sci. 2004;25:375–81.
Ganapathy V, Prasad PD. Role of transporters in placental transfer of drugs. Toxicol Appl Pharmacol. 2005;207:381–7.
De Giovanni N, Marchetti D. Cocaine and its metabolites in the placenta: a systematic review of the literature. Reprod Toxicol. 2012;33:1–14.
Bailey DN. Cocaine and cocaethylene binding to human placenta in vitro. Am J Obstet Gynecol. 1997;177:527–31.
Burchfield DJ, Lucas VW, Abrams RM, Miller RL, DeVane CL. Disposition and pharmacodynamics of methamphetamine in pregnant sheep. JAMA. 1991;265:1968–73.
Little BB, VanBeveren TT. Placental transfer of selected substances of abuse. Semin Perinatol. 1996;20:147–53.
Hakkola J, Pelkonen O, Pasanen M, Raunio H. Xenobiotic-metabolizing cytochrome P450 enzymes in the human feto-placental unit: role in intrauterine toxicity. Crit Rev Toxicol. 1998;28:35–72.
Smith LM, Santos LS. Prenatal exposure: The effects of prenatal cocaine and methamphetamine exposure on the developing child. Birth Defects Res C Embryo Today. 2016;108:142–6.
Ramamoorthy JD, Ramamoorthy S, Leibach FH, Ganapathy V. Human placental monoamine transporters as targets for amphetamines. Am J Obstet Gynecol. 1995;173:1782–7.
Grant KS, Petroff R, Isoherranen N, Stella N, Burbacher TM. Cannabis use during pregnancy: Pharmacokinetics and effects on child development. Pharmacol Ther. 2018;182:133–51.
Thompson R, DeJong K, Lo J. Marijuana use in pregnancy: a review. Obstet Gynecol Surv. 2019;74:415–28.
Lind JN, Interrante JD, Ailes EC, Gilboa SM, et al. Maternal use of opioids during pregnancy and congenital malformations: a systematic review. Pediatrics. 2017;139(6):e20164131. https://doi.org/10.1542/peds.2016-4131.
Cutler AJ, Cox DF, Gabrielson SMB, Picarillo AP, Craig AK. Association of medication-assisted treatment and short acting opioids with newborn head circumference and birth weight. J Perinatol. 2023;43:277–82.
Soto E, Bahado-Singh R. Fetal abnormal growth associated with substance abuse. Clin Obstet Gynecol. 2013;56:142–53. This scoping review provides a summary of studies that highlight the negative effects of intrauterine drug exposure on birth weight and head circumference. Despite methodological challenges in controlling for confounders, it is evident that prenatal substance exposure is associated with fetal growth restriction.
Towers CV, Hyatt BW, Visconti KC, Chernicky L, Chattin K, Fortner KB. Neonatal head circumference in newborns with neonatal abstinence syndrome. Pediatrics. 2019;143.
Hudak ML, Makker K. Fetal opioid exposure and smaller birth head circumference: cause for concern? Pediatrics. 2019;143.
Feferkorn I, Badeghiesh A, Baghlaf H, Dahan MH. The relation between cigarette smoking with delivery outcomes. An evaluation of a database of more than nine million deliveries. J Perinat Med. 2022;50:56–62. This large retrospective population-based cohort study database confirms the findings of previous smaller studies: smoking decreases the risk of preeclampsia while increasing the rate of preterm birth and small for gestational age neonates.
(2014, January 17). Smoking in Pregnancy Confirmed as a Cause of Oral Cleft Birth Defects. March of Dimes. Retrieved July 3, 2023, from https://www.marchofdimes.org/about/news/smoking-pregnancy-confirmed-cause-oral-cleft-birth-defects
Sutliff RL, Gayheart-Walsten PA, Snyder DL, Roberts J, Johnson MD. Cardiovascular effects of acute and chronic cocaine administration in pregnant and nonpregnant rabbits. Toxicol Appl Pharmacol. 1999;158:278–87.
Stek AM, Fisher BK, Baker RS, Lang U, Tseng CY, Clark KE. Maternal and fetal cardiovascular responses to methamphetamine in the pregnant sheep. Am J Obstet Gynecol. 1993;169:888–97.
Woods JR Jr, Plessinger MA, Clark KE. Effect of cocaine on uterine blood flow and fetal oxygenation. JAMA. 1987;257:957–61.
Gouin K, Murphy K, Shah PS. Effects of cocaine use during pregnancy on low birthweight and preterm birth: systematic review and meta-analyses. Am J Obstet Gynecol. 2011;204:340 e1–12. This systematic review includes 31 studies and shows the negative effects of prenatal cocaine exposure on fetal development. Cocaine exposure is significantly associated with fetal growth restriction including lower birth weight and smaller head circumference compared to non-exposed controls.
Ladhani NN, Shah PS, Murphy KE. Prenatal amphetamine exposure and birth outcomes: a systematic review and metaanalysis. Am J Obstet Gynecol. 2011;205(219):e1-7.
Gratacos E, Torres PJ, Antolin E. Use of cocaine during pregnancy. N Engl J Med. 1993;329:667.
Bauer CR, Langer JC, Shankaran S, et al. Acute neonatal effects of cocaine exposure during pregnancy. Arch Pediatr Adolesc Med. 2005;159:824–34.
Huybrechts KF, Broms G, Christensen LB, et al. Association between methylphenidate and amphetamine use in pregnancy and risk of congenital malformations: a cohort study from the International Pregnancy Safety Study Consortium. JAMA Psychiatry. 2018;75:167–75. In this large international cohort study, the authors report a slightly higher risk of congenital heart malformations among infants with methylphenidate but not amphetamine exposure in utero.
McElhatton PR, Bateman DN, Evans C, Pughe KR, Thomas SH. Congenital anomalies after prenatal ecstasy exposure. Lancet. 1999;354:1441–2.
Strauss AA, Modaniou HD, Bosu SK. Neonatal manifestations of maternal phencyclidine (PCP) abuse. Pediatrics. 1981;68:550–2.
Golden NL, Sokol RJ, Rubin IL. Angel dust: possible effects on the fetus. Pediatrics. 1980;65:18–20.
Michaud J, Mizrahi EM, Urich H. Agenesis of the vermis with fusion of the cerebellar hemispheres, septo-optic dysplasia and associated anomalies. Rep Case Acta Neuropathol. 1982;56:161–6.
Arnold GL, Kirby RS, Langendoerfer S, Wilkins-Haug L. Toluene embryopathy: clinical delineation and developmental follow-up. Pediatrics. 1994;93:216–20.
Jones KL, Smith DW. Recognition of the fetal alcohol syndrome in early infancy. Lancet. 1973;302:999–1001.
Sokol RJ, Delaney-Black V, Nordstrom B. Fetal alcohol spectrum disorder. JAMA. 2003;290:2996–9.
Wozniak JR, Riley EP, Charness ME. Clinical presentation, diagnosis, and management of fetal alcohol spectrum disorder. Lancet Neurol. 2019;18:760–70.
Lange S, Probst C, Gmel G, Rehm J, Burd L, Popova S. Global prevalence of fetal alcohol spectrum disorder among children and youth: a systematic review and meta-analysis. JAMA Pediatr. 2017;171:948–56.
Hoyme HE, Kalberg WO, Elliott AJ, et al. Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders. Pediatrics. 2016;138. Physical manifestations of FASD can sometimes be confusing andoverlap with other conditions. This article furnishes clinicians with consensus-derived clinical guidelines in diagnosing FASD to increase precision and accuracy.
O’Leary CM, Nassar N, Kurinczuk JJ, et al. Prenatal alcohol exposure and risk of birth defects. Pediatrics. 2010;126:e843–50.
Boronat S, Sanchez-Montanez A, Gomez-Barros N, et al. Correlation between morphological MRI findings and specific diagnostic categories in fetal alcohol spectrum disorders. Eur J Med Genet. 2017;60:65–71.
Nguyen VT, Chong S, Tieng QM, Mardon K, Galloway GJ, Kurniawan ND. Radiological studies of fetal alcohol spectrum disorders in humans and animal models: An updated comprehensive review. Magn Reson Imaging. 2017;43:10–26.
Andersen AM, Andersen PK, Olsen J, Gronbaek M, Strandberg-Larsen K. Moderate alcohol intake during pregnancy and risk of fetal death. Int J Epidemiol. 2012;41:405–13.
O’Leary CM, Jacoby PJ, Bartu A, D’Antoine H, Bower C. Maternal alcohol use and sudden infant death syndrome and infant mortality excluding SIDS. Pediatrics. 2013;131:e770–8.
Landgren M, Svensson L, Stromland K, Andersson Gronlund M. Prenatal alcohol exposure and neurodevelopmental disorders in children adopted from eastern Europe. Pediatrics. 2010;125:e1178–85. Findings from this study underline the common occurrence of adverse neurodevelopmental outcomes in children with FASD. Maternal consumption of alcohol during pregnancy has long-lasting unfavorable effects and causes structural abnormalities and behavioral and cognitive impairments.
Coles CD, Kable JA, Taddeo E. Math performance and behavior problems in children affected by prenatal alcohol exposure: intervention and follow-up. J Dev Behav Pediatr. 2009;30:7–15.
Mattson SN, Bernes GA, Doyle LR. Fetal alcohol spectrum disorders: a review of the neurobehavioral deficits associated with prenatal alcohol exposure. Alcohol Clin Exp Res. 2019;43:1046–62.
Pei J, Denys K, Hughes J, Rasmussen C. Mental health issues in fetal alcohol spectrum disorder. J Ment Health. 2011;20:438–48.
Peadon E, Elliott EJ. Distinguishing between attention-deficit hyperactivity and fetal alcohol spectrum disorders in children: clinical guidelines. Neuropsychiatr Dis Treat. 2010;6:509–15.
Zhou D, Lebel C, Lepage C, et al. Developmental cortical thinning in fetal alcohol spectrum disorders. Neuroimage. 2011;58:16–25.
Astley SJ (2011) Diagnosing Fetal Alcohol Spectrum Disorders (FASD) In: Prenatal Alcohol Use and Fetal Alcohol Spectrum Disorders: Diagnosis, Assessment and New Directions in Research and Multimodal Treatment (S. A. Adubato & D. E. Cohen, Eds.) (pp. 3–29). Bentham Books. https://doi.org/10.2174/97816080503141110101
Author information
Authors and Affiliations
Contributions
Dr. Cortez wrote the initial draft of the paper. Dr. Hudak critically reviewed and revised the paper. Both authors approve the paper in its final form.
Corresponding author
Ethics declarations
Conflict of Interest
Josef Cortez declares that he has no conflict of interest. Mark L. Hudak declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cortez, J., Hudak, M.L. Intrauterine Drug Exposure—What the Pediatrician Needs to Know. Part 1: General Overview, Transplacental Drug Transfer, Teratogenicity, and Fetal Alcohol Spectrum Disorder. Curr Treat Options Peds 9, 370–387 (2023). https://doi.org/10.1007/s40746-023-00279-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40746-023-00279-w