Abstract
Purpose of Review
This review sought to highlight the foundational principles of cognitive load for pediatric cardiologists and surgeons in high-stakes care environments.
Recent Findings
Measurement of cognitive load is evolving beyond retrospective and subjective numeric rating scales to include multimodal physiologic measurements that scale with cognitive load. Frequent interruptions, distractions, and task switching that characterize high-stakes cardiology environments increase cognitive load. Excessive cognitive load is increasingly associated with tangible consequences for patients, including medical errors.
Summary
Cognitive load theory is based on the idea that working memory resources are finite. When working memory demands exceed available capacity, such as under high cognitive load, task performance suffers. Psychometric, behavioral, and physiological methods can be used to measure cognitive load. Strategies for reducing cognitive load in high-stakes cardiology environments include increasing automation, improving visualization, leveraging machine learning for clinical decision support, promoting crisis resource management, utilizing simulation, and optimizing human factors/systems engineering.
Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Nemeth C, Blomberg J, Argenta C, Serio-Melvin ML, Salinas J, Pamplin J. Revealing ICU cognitive work through naturalistic decision-making methods. J Cogn Eng Decis Mak. 2016;10:350–68.
Institute of Medicine (US) Committee on Quality of Health Care in America. To err is human: building a safer health system. Washington, DC: National Academies Press. 2000
Rothschild JM, Landrigan CP, Cronin JW, et al. The critical care safety study: the incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med. 2005;33:1694–700.
Graber ML, Kissam S, Payne VL, Meyer AND, Sorensen A, Lenfestey N, et al. Cognitive interventions to reduce diagnostic error: a narrative review. BMJ Qual Saf. 2012;21:535–57.
Paas F, Tuovinen JE, Tabbers H, Van Gerven PWM. Cognitive load measurement as a means to advance cognitive load theory. Educ Psychol. 2003;38:63–71.
Sweller J, van Merrienboer JJG, Paas FGWC. Cognitive architecture and instructional design. Educ Psychol Rev. 1998;10:251–96.
van Merriënboer JJG, Sweller J. Cognitive load theory in health professional education: design principles and strategies. Med Educ. 2010;44:85–93.
Sweller J. Element interactivity and intrinsic, extraneous, and germane cognitive load. Educ Psychol Rev. 2010;22:123–38.
Reason J. Human error: models and management. BMJ. 2000;320:768–70.
Byrne MD, Kirlik A. Using computational cognitive modeling to diagnose possible sources of aviation error. Int J Aviat Psychol. 2005;15:135–55.
Yanowitch RE. Joint committee on aviation pathology: IV. Crew behavior in accident causation. Aviat Space Environ Med. 1977;48:918–21.
Helmreich RL. Managing human error in aviation. Sci Am. 1997;276:62–7.
Barnett A. Aviation safety: a whole new world? Transp Sci. 2020;54:84–96.
Laxmisan A, Hakimzada F, Sayan OR, Green RA, Zhang J, Patel VL. The multitasking clinician: decision-making and cognitive demand during and after team handoffs in emergency care. Int J Med Inform. 2007;76:801–11.
Pham JC, Story JL, Hicks RW, Shore AD, Morlock LL, Cheung DS, et al. National study on the frequency, types, causes, and consequences of voluntarily reported emergency department medication errors. J Emerg Med. 2011;40:485–92.
Lou SS, Kim S, Harford D, Warner BC, Payne PRO, Abraham J, et al. Effect of clinician attention switching on workload and wrong-patient errors. Br J Anaesth. 2022;129:e22–4. This retrospective observational study defined attention switching, identified continuous EHR use time through audit logs, and measured wrong-patient errors using the validated retract-and-reorder decision rule. Using their definition and stated matrices, after adjusting for patient load and order volume, an increase in the rate of attention switching was found to significantly increase the risk for wrong-patient errors, as well as total EHR time for frontline APPs across multiple surgical ICUs in a single institution.
Yurko YY, Scerbo MW, Prabhu AS, Acker CE, Stefanidis D. Higher mental workload is associated with poorer laparoscopic performance as measured by the NASA-TLX tool. Simul Healthc. 2010;5:267–71.
Manor-Shulman O, Beyene J, Frndova H, Parshuram CS. Quantifying the volume of documented clinical information in critical illness. J Crit Care. 2008;23:245–50.
Held N, Neumeier A, Amass T, Harry E, Huie TJ, Moss M. Extraneous load events correlate with cognitive burden amongst multidisciplinary providers during intensive care unit rounds. In: TP19. TP019 quality, process, and outcomes in acute and critical care. Am Thorac Soc. 2021; A1683–A1683.
Friedman ML, McBride ME. Changes in cognitive function after pediatric intensive care unit rounds: a prospective study. Diagnosis (Berl). 2016;3:123–8.
Fundora MP, Liu J, Calamaro C, Mahle WT, Kc D. The association of workload and outcomes in the pediatric cardiac ICU. Pediatr Crit Care Med. 2021;22:683–91. This retrospective, single-center study performed a regression to study the influence of bed occupancy on orders, length of stay, and mortality. After controlling for a number of factors, it was found that an increased bed occupancy, which was posed as a surrogate for workload, and lower staffing were associated with increased mortality, length of stay, imaging orders, and laboratory turn-around time.
Collins R. Clinician cognitive overload and its implications for nurse leaders. Nurse Lead. 2020;18:44–7.
Ripp J. Cognitive load as a mediator of the relationship between workplace efficiency and well-being. Jt Comm J Qual Patient Saf. 2021;47:74–5. An editorial review of contemporary literature regarding the effects of increasing cognitive demand, measured by task load index, on quality of patient care, workplace efficiency, as well as burnout and provider well-being.
Paas FG, Van Merriënboer JJ, Adam JJ. Measurement of cognitive load in instructional research. Percept Mot Skills. 1994;79:419–30.
Hart SG, Staveland LE. Development of NASA-TLX (task load index): results of empirical and theoretical research. In: Hancock PA, Meshkati N (eds) Advances in psychology. North-Holland, Amsterdam; 1988; 139–183.
Hart SG. Nasa-task load index (NASA-TLX); 20 years later. Proc Hum Fact Ergon Soc Annu Meet. 2006;50:904–8.
Cohen AS, Dinzeo TJ, Donovan NJ, Brown CE, Morrison SC. Vocal acoustic analysis as a biometric indicator of information processing: implications for neurological and psychiatric disorders. Psychiatry Res. 2015;226:235–41.
Van Gerven PWM, Paas F, Van Merriënboer JJG, Schmidt HG. Memory load and the cognitive pupillary response in aging. Psychophysiology. 2004;41:167–74.
Antonenko P, Paas F, Grabner R, van Gog T. Using electroencephalography to measure cognitive load. Educ Psychol Rev. 2010;22:425–38.
Wilson GF, Eggemeier FT. Psychophysiological assessment of workload in multi-task environments. In: Damos D (ed) Multiple-task performance. CRC Press, Boca Raton. 1991
Whelan RR. Neuroimaging of cognitive load in instructional multimedia. Educ Res Rev. 2007;2:1–12.
Brünken R, Seufert T, Paas F. Measuring cognitive load. In: Plass JL, Moreno R, Brünken R, editors. Cognitive load theory. Cambridge: Cambridge University Press; 2010. p. 181–202.
Klepsch M, Schmitz F, Seufert T. Development and validation of two instruments measuring intrinsic, extraneous, and germane cognitive load. Front Psychol. 2017;8:1997.
Brünken R, Steinbacher S, Plass JL, Leutner D. Assessment of cognitive load in multimedia learning using dual-task methodology. Exp Psychol. 2002;49:109–19.
Park B, Brünken R. The rhythm method: A new method for measuring cognitive load-an experimental dual-task study. Appl Cogn Psychol. 2015;29:232–43.
Jaeggi SM, Buschkuehl M, Perrig WJ, Meier B. The concurrent validity of the N-back task as a working memory measure. Memory. 2010;18:394–412.
Paas FGWC, Paas FGW. Training strategies for attaining transfer of problem-solving skill in statistics: a cognitive-load approach. J Educ Psychol. 1992;84:429–34.
Paas FGWC, Van Merriënboer JJG. Variability of worked examples and transfer of geometrical problem-solving skills: a cognitive-load approach. J Educ Psychol. 1994;86:122–33.
Ayres P. Using subjective measures to detect variations of intrinsic cognitive load within problems. Learn Instr. 2006;16:389–400.
van Gog T, Paas F. Instructional efficiency: revisiting the original construct in educational research. Educ Psychol. 2008;43:16–26.
Barajas-Bustillos MA, Maldonado-Macías A, Serrano-Rosa MA, Hernandez-Arellano JL, Llamas-Alonso L, Balderrama-Armendariz O. Impact of experience on the sensitivity, acceptability, and intrusive of two subjective mental workload techniques: The NASA TLX and workload profile. Work. 2023. https://doi.org/10.3233/WOR-211324.
Wilson GF, Russell CA. Real-time assessment of mental workload using psychophysiological measures and artificial neural networks. Hum Factors. 2003;45:635–43.
Gevins A, Smith ME, Leong H, McEvoy L, Whitfield S, Du R, Rush G. Monitoring working memory load during computer-based tasks with EEG pattern recognition methods. Hum Factors. 1998;40:79–91.
Brouwer A-M, Hogervorst MA, van Erp JBF, Heffelaar T, Zimmerman PH, Oostenveld R. Estimating workload using EEG spectral power and ERPs in the n-back task. J Neural Eng. 2012;9:045008.
Howard SJ, Burianová H, Ehrich J, Kervin L, Calleia A, Barkus E, et al. Behavioral and fMRI evidence of the differing cognitive load of domain-specific assessments. Neuroscience. 2015;297:38–46.
Bauer R, Jost L, Günther B, Jansen P. Pupillometry as a measure of cognitive load in mental rotation tasks with abstract and embodied figures. Psychol Res. 2022;86:1382–96.
Grassmann M, Vlemincx E, von Leupoldt A, Mittelstädt JM, Van den Bergh O. Respiratory changes in response to cognitive load: a systematic review. Neural Plast. 2016;2016:8146809.
Woody A, Hooker ED, Zoccola PM, Dickerson SS. Social-evaluative threat, cognitive load, and the cortisol and cardiovascular stress response. Psychoneuroendocrinology. 2018;97:149–55.
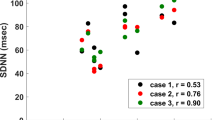
Visnovcova Z, Mestanik M, Javorka M, Mokra D, Gala M, Jurko A, et al. Complexity and time asymmetry of heart rate variability are altered in acute mental stress. Physiol Meas. 2014;35:1319–34.
Visnovcova Z, Mestanik M, Gala M, Mestanikova A, Tonhajzerova I. The complexity of electrodermal activity is altered in mental cognitive stressors. Comput Biol Med. 2016;79:123–9.
Romine WL, Schroeder NL, Graft J, Yang F, Sadeghi R, Zabihimayvan M, et al. Using machine learning to train a wearable device for measuring students’ cognitive load during problem-solving activities based on electrodermal activity, body temperature, and heart rate: development of a cognitive load tracker for both personal and classroom use. Sensors. 2020;20:4833.
Chen S, Epps J, Chen F. A comparison of four methods for cognitive load measurement. In: Proceedings of the 23rd Australian Computer-Human Interaction Conference. OzCHI '11: The Annual Meeting of the Australian Special Interest Group for Computer Human Interaction Canberra Australia 28 November 2011- 2 December 2011. Association for Computing Machinery. 2011; 76–79.
Gerstle CR. Parallels in safety between aviation and healthcare. J Pediatr Surg. 2018;53:875–8.
Helmreich RL, Merritt AC, Wilhelm JA. The evolution of Crew Resource Management training in commercial aviation. Int J Aviat Psychol. 1999;9:19–32.
Zayas-Cabán T, Haque SN, Kemper N. Identifying opportunities for workflow automation in health care: lessons learned from other industries. Appl Clin Inform. 2021;12:686–97.
Zhang J, Gajjala S, Agrawal P, Tison GH, Hallock LA, Beussink-Nelson L, et al. Fully automated echocardiogram interpretation in clinical practice. Circulation. 2018;138:1623–35.
Hahn J-O, Inan OT. Physiological closed-loop control in critical care: opportunities for innovations. Prog Biomed Eng. 2022;4: 033001.
Carayon P, Wetterneck TB, Alyousef B, Brown RL, Cartmill RS, McGuire K, et al. Impact of electronic health record technology on the work and workflow of physicians in the intensive care unit. Int J Med Inform. 2015;84:578–94.
Khairat SS, Dukkipati A, Lauria HA, Bice T, Travers D, Carson SS. The impact of visualization dashboards on quality of care and clinician satisfaction: integrative literature review. JMIR Hum Factors. 2018;5:e22.
Engelbrecht L, Botha A, Alberts R. Designing the visualization of information. Int J Image Graph. 2015;15:1540005.
Workman M, Lesser MF, Kim J. An exploratory study of cognitive load in diagnosing patient conditions. Int J Qual Health Care. 2007;19:127–33.
Faiola A, Srinivas P, Hillier S. Improving patient safety: integrating data visualization and communication into ICU workflow to reduce cognitive load. Proc Int Symp Hum Factors Ergon Health Care. 2015;4:55–61.
Pirracchio R, Cohen MJ, Malenica I, Cohen J, Chambaz A, Cannesson M, et al. Big data and targeted machine learning in action to assist medical decision in the ICU. Anaesth Crit Care Pain Med. 2019;38:377–84.
Pinsky MR, Dubrawski A, Clermont G. Intelligent clinical decision support. Sensors. 2022;22:1408.
Park SJ, Cho K-J, Kwon O, Park H, Lee Y, Shim WH, et al. Development and validation of a deep-learning-based pediatric early warning system: a single-center study. Biomed J. 2022;45:155–68. A single-center study that developed and validated a deep-learning pediatric early warning system for predicting cardiopulmonary arrest and unexpected need for transfer to the PICU using retrospective chart review. The system was validated against the pediatric early warning score (PEWS) and was found to be superior.
Jentzer JC, Kashou AH, Murphree DH. Clinical applications of artificial intelligence and machine learning in the modern cardiac intensive care unit. Intell-Based Med. 2023;7:100089. This review article discusses existing and future machine learning applications in the CICU including mortality risk stratification, prognostication, non-fatal event prediction, diagnosis, phenotyping, electrocardiogram and echocardiogram interpretation to decrease provider cognitive load.
Hall KK. Making healthcare safer III: a critical analysis of existing and emerging patient safety practices. Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services, Washington, D.C. 2020.
Graber ML. Reaching 95%: decision support tools are the surest way to improve diagnosis now. BMJ Qual Saf. 2022;31:415–8.
Ehrmann DE, Gallant SN, Nagaraj S, Goodfellow SD, Eytan D, Goldenberg A, et al. Evaluating and reducing cognitive load should be a priority for machine learning in healthcare. Nat Med. 2022;28:1331–3.
DECIDE-AI Steering Group. DECIDE-AI: new reporting guidelines to bridge the development-to-implementation gap in clinical artificial intelligence. Nat Med. 2021;27:186–7.
Rusin CG, Acosta SI, Vu EL, Ahmed M, Brady KM, Penny DJ. Automated prediction of cardiorespiratory deterioration in patients with single ventricle. J Am Coll Cardiol. 2021;77:3184–92. Retrospective single-center study that developed and validated a real-time algorithm to predict cardiorespiratory deterioration in patients with single-ventricle physiology during interstage hospitalization. The algorithm provides 1-2 hours of advanced warning in 62% of cardiorespiratory deterioration events for the single-ventricle physiology population with minimal additional patient alarms.
Gaba DM. Anesthesia crisis management and human error in anesthesiology. Proc Hum Factors Soc Ann Meet. 1991;35:686–686.
Bishop R, Porges C, Carlisle M, Strickland R. Crisis resource management in medicine: a Clarion call for change. Curr Treat Options Pediatr. 2020;6:299–316.
Carne B, Kennedy M, Gray T. Review article: crisis resource management in emergency medicine. Emerg Med Australas. 2012;24:7–13.
Rajendram P, Notario L, Reid C, Wira CR, Suarez JI, Weingart SD, et al. Crisis resource management and high-performing teams in hyperacute stroke care. Neurocrit Care. 2020;33:338.
Huffman EM, Anton NE, Athanasiadis DI, Ahmed R, Cooper D, Stefanidis D, et al. Multidisciplinary simulation-based trauma team training with an emphasis on crisis resource management improves residents’ non-technical skills. Surgery. 2021;170:1083–6.
Gaba DM, Howard SK, Fish KJ, Smith BE, Sowb YA. Simulation-based training in anesthesia crisis resource management (ACRM): a decade of experience. Simul Gaming. 2001;32:175–93.
Szulewski A, Braund H, Egan R, Gegenfurtner A, Hall AK, Howes D, et al. Starting to think like an expert: an analysis of resident cognitive processes during simulation-based resuscitation examinations. Ann Emerg Med. 2019;74:647–59.
Ghanbari S, Haghani F, Barekatain M, Jamali A. A systematized review of cognitive load theory in health sciences education and a perspective from cognitive neuroscience. J Educ Health Promot. 2020;9:176.
Carayon P, Wooldridge A, Hose B-Z, Salwei M, Benneyan J. Challenges and opportunities for improving patient safety through human factors and systems engineering. Health Aff. 2018;37:1862–9.
Grayson D, Boxerman S, Potter P, et al. Do transient working conditions trigger medical errors? In: Henriksen K, Battles JB, Marks ES, et al., editors. Advances in patient safety: From research to implementation, vol. 1: Research Findings. Rockville (MD): Agency for Healthcare Research and Quality (US); 2005. https://www.ncbi.nlm.nih.gov/books/NBK20465/
Flohr L, Beaudry S, Johnson KT, West N, Burns CM, Ansermino JM, et al. Clinician-driven design of VitalPAD–an intelligent monitoring and communication device to improve patient safety in the intensive care unit. IEEE J Transl Eng Health Med. 2018;6:1–14.
Stansfeld SA, Matheson MP. Noise pollution: non-auditory effects on health. Br Med Bull. 2003;68:243–57.
Murthy VS, Malhotra SK, Bala I, Raghunathan M. Detrimental effects of noise on anaesthetists. Can J Anaesth. 1995;42:608–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schaffer, C., Goldart, E., Ligsay, A. et al. Take a Load Off: Understanding, Measuring, and Reducing Cognitive Load for Cardiologists in High-Stakes Care Environments. Curr Treat Options Peds 9, 122–135 (2023). https://doi.org/10.1007/s40746-023-00272-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40746-023-00272-3