Abstract
Purpose of Review
In this review, we aim to provide insight into the current state of spinal anesthesia (SA) in pediatric urologic surgery while also acknowledging its historical use in pediatric general and orthopedic procedures. More specifically, we will highlight our own institutional protocol and techniques aimed at prolonging the effects of spinal anesthesia for cases with an anticipated duration lasting > 60 min.
Recent Findings
Recent studies have described success rates of nearly 90% for a wide range of operative times, with the maximum duration reported to be nearly 3 h. Most studies include a variety of penoscrotal cases under a single-shot spinal block of bupivacaine with or without adjunct medications, preoperatively and intraoperatively, to prolong effects. However, an approach has been described for more complex cases including ureteral reimplantation, ureterocele repair, megaureter repair, open pyeloplasty, and feminizing genitoplasty, combining spinal injection and caudal catheter placement.
Summary
Spinal anesthesia for pediatric urologic surgery requires close collaboration between anesthesiology and surgical teams. In general, spinal anesthesia has been used to safely perform urologic cases lasting < 60 min in duration; however, adjunctive medications have been used to prolong effects for longer, more complex cases with excellent outcomes.

Similar content being viewed by others
Data Availability
The data that support the findings of this study are available on request from the corresponding author, [CFG].
Abbreviations
- SA:
-
Spinal anesthesia
- PUV:
-
Posterior urethral valve
- PACU:
-
Post-anesthesia care unit
- LOS:
-
Length of stay
- OR:
-
Operating room
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bainbridge WS. A report of twelve operations on infants and young children during spinal anesthesia. Arch Pediatr. 1901;18:570–4.
Lambertz A, Schalte G, Winter J, Roth A, Busch D, Ulmer TF, et al. Spinal anesthesia for inguinal hernia repair in infants: a feasible and safe method even in emergency cases. Pediatr Surg Int. 2014;30(10):1069–73.
Kachko L, Birk E, Simhi E, Tzeitlin E, Freud E, Katz J. Spinal anesthesia for noncardiac surgery in infants with congenital heart diseases. Paediatr Anaesth. 2012;22(7):647–53.
Bong CL, Yeo AS, Fabila T, Tan JS. A pilot study of dexmedetomidine sedation and caudal anesthesia for inguinal hernia repair in infants. Paediatr Anaesth. 2016;26(6):621–7.
Jones LJ, Craven PD, Lakkundi A, et al. Regional (spinal, epidural, caudal) versus general anaesthesia in preterm infants undergoing inguinal herniorrhaphy in early infancy. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD003669.pub2.
Batra YK, Lokesh VC, Panda NB, Rajeev S, Rao KL. Dose-response study of intrathecal fentanyl added to bupivacaine in infants undergoing lower abdominal and urologic surgery. Paediatr Anaesth. 2008;18(7):613–9.
Jevtovic-Todorovic V, Hartman RE, Izumi Y, Benshoff ND, Dikranian K, Zorumski CF, et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci. 2003;23(3):876–82.
Istaphanous GK, Ward CG, Nan X, Hughes EA, McCann JC, McAuliffe JJ, et al. Characterization and quantification of isoflurane-induced developmental apoptotic cell death in mouse cerebral cortex. Anesth Analg. 2013;116(4):845–54.
Paule MG, Li M, Allen RR, Liu F, Zou X, Hotchkiss C, et al. Ketamine anesthesia during the first week of life can cause long-lasting cognitive deficits in rhesus monkeys. Neurotoxicol Teratol. 2011;33(2):220–30.
Raper J, Alvarado MC, Murphy KL, Baxter MG. Multiple anesthetic exposure in infant monkeys alters emotional reactivity to an acute stressor. Anesthesiology. 2015;123(5):1084–92.
McCann ME, de Graaff JC, Dorris L, Disma N, Withington D, Bell G, et al. Neurodevelopmental outcome at 5 years of age after general anaesthesia or awake-regional anaesthesia in infancy (GAS): an international, multicentre, randomised, controlled equivalence trial. Lancet. 2019;393(10172):664–77.
Sun LS, Li G, Miller TL, Salorio C, Byrne MW, Bellinger DC, et al. Association between a single general anesthesia exposure before age 36 months and neurocognitive outcomes in later childhood. JAMA. 2016;315(21):2312–20.
Warner DO, Zaccariello MJ, Katusic SK, Schroeder DR, Hanson AC, Schulte PJ, et al. Neuropsychological and behavioral outcomes after exposure of young children to procedures requiring general anesthesia: the Mayo Anesthesia Safety in Kids (MASK) study. Anesthesiology. 2018;129(1):89–105.
FDA Drug Safety Communication. FDA review results in new warnings about using general anesthetics and sedation drugs in young children and pregnant women. U.S. Food & Drug Administration; 2016. updated 03/08/2018. Available from: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-review-results-newwarnings-about-using-general-anesthetics-and
Whitaker EE, Wiemann BZ, DaJusta DG, Alpert SA, Ching CB, McLeod DJ, et al. Spinal anesthesia for pediatric urological surgery: reducing the theoretic neurotoxic effects of general anesthesia. J Pediatr Urol. 2017;13(4):396–400.
Ebert KM, Jayanthi VR, Alpert SA, Ching CB, DaJusta DG, Fuchs ME, et al. Benefits of spinal anesthesia for urologic surgery in the youngest of patients. J Pediatr Urol. 2019;15(1):49 e1-e5.
•• Trifa M, Tumin D, Whitaker EE, Bhalla T, Jayanthi VR, Tobias JD. Spinal anesthesia for surgery longer than 60 min in infants: experience from the first 2 years of a spinal anesthesia program. J Anesth. 2018;32(4):637–40. This study highlights the safe and effective use of SA for urologic cases with an operative time of 60+ min. The SA protocol used at this institution includes intrathecal clonidine and epinephrine in addition to bupivacaine to prolong anesthetic effects.
Davidson AJ, Sun LS. Clinical evidence for any effect of anesthesia on the developing brain. Anesthesiology. 2018;128(4):840–53.
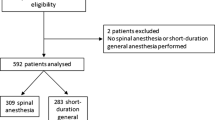
•• Handlogten K, Warner L, Granberg C, Gargollo P, Thalji L, Haile D. Implementation of a spinal anesthesia and sedation protocol that reliably prolongs infant spinal anesthesia: case series of 102 infants who received spinal anesthesia for urologic surgery. Paediatr Anaesth. 2020;30(12):1355–62. This study outlines an SA protocol that has been safely implemented for prolonged urologic surgery with a low failure rate. When compared to their general anesthesia counterparts, SA patients had shorter anesthetic, operative, and recovery times.
Fiadjoe JE, Nishisaki A, Jagannathan N, Hunyady AI, Greenberg RS, Reynolds PI, et al. Airway management complications in children with difficult tracheal intubation from the Pediatric Difficult Intubation (PeDI) registry: a prospective cohort analysis. Lancet Respir Med. 2016;4(1):37–48.
Holzki J, Laschat M, Puder C. Iatrogenic damage to the pediatric airway. Mechanisms and scar development. Paediatr Anaesth. 2009;19(Suppl 1):131–46.
Schedlbauer EM, Todt I, Ernst A, Seidl RO. Iatrogenic tracheal rupture in children: a retrospective study. Laryngoscope. 2009;119(3):571–5.
•• Jayanthi VR, Spisak K, Smith AE, Martin DP, Ching CB, Bhalla T, et al. Combined spinal/caudal catheter anesthesia: extending the boundaries of regional anesthesia for complex pediatric urological surgery. J Pediatr Urol. 2019;15(5):442–7. This study describes a combined SA and caudal catheter technique for complex urologic surgery, effectively expanding the scope of abdominopelvic surgery under regional anesthesia. Cases ranging 1–3 h were safely performed with a low risk of conversion to general anesthesia.
Oddby E, Englund S, Lönnqvist PA. Postoperative nausea and vomiting in paediatric ambulatory surgery: sevoflurane versus spinal anaesthesia with propofol sedation. Paediatr Anaesth. 2001;11(3):337–42.
Imbelloni LE, Vieira EM, Sperni F, Guizellini RH, Tolentino AP. Spinal anesthesia in children with isobaric local anesthetics: report on 307 patients under 13 years of age. Paediatr Anaesth. 2006;16(1):43–8.
Kachko L, Simhi E, Freud E, Dlugy E, Katz J. Impact of spinal anesthesia for open pyloromyotomy on operating room time. J Pediatr Surg. 2009;44(10):1942–6.
Ing C, Sun LS, Friend AF, Roh A, Lei S, Andrews H, et al. Adverse events and resource utilization after spinal and general anesthesia in infants undergoing pyloromyotomy. Reg Anesth Pain Med. 2016;41(4):532–7.
Suresh S, Ecoffey C, Bosenberg A, Lonnqvist PA, de Oliveira GS Jr, de Leon Casasola O, et al. The European Society of Regional Anaesthesia and Pain Therapy/American Society of Regional Anesthesia and Pain Medicine recommendations on local anesthetics and adjuvants dosage in pediatric regional anesthesia. Reg Anesth Pain Med. 2018;43(2):211–6.
Mahe V, Ecoffey C. Spinal anesthesia with isobaric bupivacaine in infants. Anesthesiology. 1988;68(4):601–3.
Gupta A, Saha U. Spinal anesthesia in children: a review. J Anaesthesiol Clin Pharmacol. 2014;30(1):10–8.
Williams RK, Adams DC, Aladjem EV, Kreutz JM, Sartorelli KH, Vane DW, et al. The safety and efficacy of spinal anesthesia for surgery in infants: the Vermont Infant Spinal Registry. Anesth Analg. 2006;102(1):67–71.
Dontukurthy S, Tobias JD. Update on local anesthetic toxicity, prevention and treatment during regional anesthesia in infants and children. J Pediatr Pharmacol Ther. 2021;26(5):445–54.
Wright TE, Orr RJ, Haberkern CM, Walbergh EJ. Complications during spinal anesthesia in infants: high spinal blockade. Anesthesiology. 1990;73(6):1290–2.
• Osmani F, Ferrer F, Barnett NR. Regional anesthesia for ambulatory pediatric penoscrotal procedures. J Pediatr Urol. 2021;17(6):836–44. https://doi.org/10.1016/j.jpurol.2021.07.017. This review highlights the various strategies for regional anesthesia in penoscrotal surgery, including but not limited to peripheral nerve blocks and neuraxial anesthesia.
Eisenach JC, De Kock M, Klimscha W. α2-Adrenergic agonists for regional anesthesia. A clinical review of clonidine (1984–1995). Anesthesiology. 1996;85(3):655–74.
Gabriel JS, Gordin V. Alpha 2 agonists in regional anesthesia and analgesia. Curr Opin Anaesthesiol. 2001;14(6):751–3.
Rochette A, Raux O, Troncin R, Dadure C, Verdier R, Capdevila X. Clonidine prolongs spinal anesthesia in newborns: a prospective dose-ranging study. Anesth Analg. 2004;98(1):56–9.
Cao JP, Miao XY, Liu J, Shi XY. An evaluation of intrathecal bupivacaine combined with intrathecal or intravenous clonidine in children undergoing orthopedic surgery: a randomized double-blinded study. Paediatr Anaesth. 2011;21(4):399–405.
Kaabachi O, Ben Rajeb A, Mebazaa M, Safi H, Jelel C, Ben Ghachem M, et al. Spinal anesthesia in children: comparative study of hyperbaric bupivacaine with or without clonidine. Ann Fr Anesth Reanim. 2002;21(8):617–21.
Rice LJ, DeMars PD, Whalen TV, Crooms JC, Parkinson SK. Duration of spinal anesthesia in infants less than one year of age. Comparison of three hyperbaric techniques. Reg Anesth. 1994;19(5):325–9.
Poonai N, Spohn J, Vandermeer B, et al. Intranasal dexmedetomidine for procedural distress in children: a systematic review. Pediatrics. 2020;145(1):e20191623.
Lam F, Bhutta AT, Tobias JD, Gossett JM, Morales L, Gupta P. Hemodynamic effects of dexmedetomidine in critically ill neonates and infants with heart disease. Pediatr Cardiol. 2012;33(7):1069–77.
Arends J, Tobias JD. Hypothermia following spinal anesthesia in an infant: potential impact of intravenous dexmedetomidine and intrathecal clonidine. J Med Cases. 2019;10(11):319–22.
Finkel JC, Quezado ZM. Hypothermia-induced bradycardia in a neonate receiving dexmedetomidine. J Clin Anesth. 2007;19(4):290–2.
Batra YK, Rakesh SV, Panda NB, Lokesh VC, Subramanyam R. Intrathecal clonidine decreases propofol sedation requirements during spinal anesthesia in infants. Paediatr Anaesth. 2010;20(7):625–32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Bridget L. Findlay declares that she has no conflict of interest. Francis A. Jefferson declares that he has no conflict of interest. Patricio C. Gargollo declares that he has no conflict of interest. Dawit Haile declares that he has no conflict of interest. Candace F. Granberg declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Urology
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Findlay, B.L., Jefferson, F.A., Gargollo, P.C. et al. Review of Spinal Anesthesia for Pediatric Genitourinary Surgery. Curr Treat Options Peds 9, 81–92 (2023). https://doi.org/10.1007/s40746-023-00269-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40746-023-00269-y