Abstract
Introduction
Skin ulcers (SU) represent one of the most frequent manifestations of systemic sclerosis (SSc), occurring in almost 50% of scleroderma patients. SSc-SU are often particularly difficult to treat with conventional systemic and local therapies. In this study, a preliminary evaluation of the role and effectiveness of blue light photobiomodulation (PBM) therapy with EmoLED® in the treatment of scleroderma skin ulcers (SSc-SU) was performed.
Methods
We retrospectively analyzed 12 consecutive SSc patients with a total of 15 SU on finger hands. All patients were treated with adequate systemic therapy and local treatment for SU; after a standard skin ulcer bed preparation with debridement of all lesions, EmoLED® was performed. All patients were locally treated every week during 2 months of follow-up; SU data were collected after 4 weeks (T4) and 8 weeks (T8). Eight SSc patients with comparable SU were also evaluated as controls.
Results
The application of EmoLED® in addition to debridement apparently produced faster healing of SU. Complete healing of SU was recorded in 41.6% cases during EmoLED® treatment. Significant improvements in SU area, length, and width, wound bed, and related pain were observed in EmoLED® patients from T0 to T8. Control subjects treated with standard systemic/local therapies merely showed an amelioration of SU area and width at the end of the follow-up. No procedural or post-procedural adverse events were reported.
Conclusions
The positive clinical results and the absence of side effects suggest that EmoLED® could be a promising tool in the management of SSc-SU, with an interesting role to play in the healing process in addition to conventional systemic and local treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Skin ulcers represent one of the most frequent manifestations of systemic sclerosis. They are painful, recurrent, hard to heal, carry an increased risk of infection, and are frequently responsible for pain and disability. |
Photobiomodulation (PBM) with blue light was recently studied in the management of hard-to-heal wounds. |
Our project could be considered a pilot study that primarily served to assess the feasibility and safety of the EmoLED® device; we also aimed to evaluate the treatment efficacy in the heterogeneous framework of SSc-SU. |
The application of blue light PBM with EmoLED® in addition to debridement apparently produced faster healing of SU, with the formation of granulation tissue and regularization of margins. |
EmoLED® could be a promising safe, effective, noninvasive tool to treat SSc-SU, with an interesting role to play in the healing process in addition to conventional systemic and local therapies. |
Introduction
Systemic sclerosis (SSc) is a connective tissue disease characterized by endothelial dysfunction, autoimmunity abnormalities, and fibrosis of the skin and internal organs [1,2,3]. Skin ulcers (SU) represent one of the most frequent manifestations of SSc, occurring in almost 50% of SSc patients. SSc-SU are painful, recurrent, hard to heal, and carry an increased risk of infection, osteomyelitis, and gangrene, sometimes requiring amputation. They are frequently responsible for pain and disability, which can severely affect SSc patients’ quality of life [4,5,6,7,8,9]. Standard systemic and local approaches may support wound healing [9,10,11]. In our experience [12,13,14,15], the therapeutic approach for SSc-SU should be invariably tailored to the individual patient on the basis of both the general clinical conditions and careful evaluation of a single skin wound. Systemic and local treatments encompass both pathogenetic and symptomatic drugs, as well as different nonpharmacological measures [9]. However, a significant percentage of scleroderma skin ulcers still represent a challenge to clinicians. Photobiomodulation (PBM) with blue light was recently studied for the management of hard-to-heal wounds. Despite several published research papers, the mechanism underlying photobiomodulation is still not completely understood, and the application of blue light to improve wound healing is a relatively new research area [16,17,18,19,20,21,22]. In the setting of research into new therapies that support and stimulate the healing processes of wounds, a medical device emitting blue light (EmoLED®) has been developed. The principle of this medical device is based on light energy transfer from the tool to the patient. The light energy interacts with some endogenous chromophores in the blood and skin, activating the photobiomodulation mechanism and thus stimulating the physiological processes of wound healing. The application of medical devices utilizing blue LED light in animal models has been extensively analyzed [17, 23], and has demonstrated their efficacy and safety.
The aim of this study was to evaluate the role and effectiveness of EmoLED® blue light photobiomodulation therapy, in addition to standard treatments, in the management of SSc-SU. Our project can be considered a pilot study that primarily served to assess the feasibility and safety of the device but also aimed to evaluate the efficacy of this treatment in the heterogeneous framework of SSc-SU.
Methods
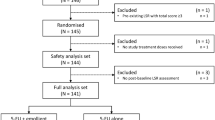
We retrospectively evaluated the effects of EmoLED® in the local treatment of SSc-SU in 12 consecutive SSc patients referred to our scleroderma unit during the last year. Over the same period, 8 SSc patients with comparable SU were also consecutively evaluated as controls. Eligible patients had ages between 18 and 80 years, at least 1 SSc-SU, and satisfied the ACR/EULAR 2013 classification criteria for systemic sclerosis [2]. Patients < 18 or > 80 years old were ruled out.
The patients’ clinical data were carefully evaluated on the basis of individual medical records, including demographic and clinical findings (Table 1), as well as SU features (dimension, depth, area, wound bed and perilesional skin aspects, presence of exudates and possible signs of infection, and a measure of pain). SSc-SU can be considered a “loss of substance involving epidermis, basement membrane, and dermis, and frequently deeper skin structures; lesions may be multiple, recurrent, and/or relapsing; they are localized at one or more skin areas, often acral zones of the hands and feet” [9]. We recruited patients with typical SSc digital ulcers of the hands (DU) located on the fingertips or close to the nails, according to the common definition and classification presented in the literature [9].
Cutaneous swabs were performed when needed at the level of lesion areas, with care taken to previously remove any dried exudates, slough, or dressing residue with saline solution or surgical debridement. Table 2 reports baseline SU features of our SSc cohort.
All patients were treated with standard systemic therapy for scleroderma vasculopathy [11] at the time of SU presentation, using one or more vasoactive drugs (Table 1). Local treatment of the SU was carried out according to the wound bed preparation model, mainly based on the TIME framework [10, 24, 25].
The blue LED device EmoLED® is a commercially available portable medical device produced in Sesto Fiorentino (Florence, Italy) and composed of six LED light sources that emit blue light at 400–430 nm, as already described in the literature [26, 27]. It has a power density of 120 mW/cm2 and an energy density of 7.2 J/cm2. The emitted continuous radiation is made uniform over the entire area by the optical system of the device.
The technical specifications of EmoLED® are summarized in Table 3.
After adequate wound bed preparation, EmoLED® was applied for 60 s at a distance of 4 cm from the lesion on every 50-mm-diameter circular sub-area, and a standard medication was subsequently applied according to each SU feature. Every EmoLED® administration was performed in our clinic, and patients were then instructed to apply standard medications daily at home. All patients were systematically re-evaluated and locally treated by trained rheumatologists every week during 2 months of follow-up; SU data (length, width, area, wound bed, perilesional skin features, presence/absence of lesion exudate) were collected after 4 and 8 weeks (Tables 4, 5).
Each patient was also instructed to record the following data during the follow-up period: pain level on a 0–10 mm scale (NRS: numeric rating scale), use of analgesics, possible adverse reactions to the treatment.
The study was approved by the local ethics committee Area Vasta Emilia Nord (protocol no. 275/16), and written informed consent was obtained from all participants.
Statistical Analysis
Data analysis was carried out using the SPSS statistical package (version 26.0, IBM Software, USA). Comparisons between values were performed using the ANOVA test and Fisher’s exact test for continuous and noncontinuous variables, respectively. All descriptive data are expressed as mean ± standard deviation (SD). p values ≤ 0.05 were considered statistically significant.
Results
Comparable clinical features of SSc patients and SU were observed in both the EmoLED® group (F/M 8/4, lc/dc subsets 6/6, mean age ± SD 62.7 ± 8.3 years (44–72), mean disease duration ± SD 12.5 ± 7.1 years (0.5–24)) and in the control group (F/M 6/2, lc/dc subsets 5/3, mean age ± SD 68.0 ± 10.5 years (55–82), mean disease duration ± SD 16.5 ± 12.5 years (4–36)). Table 1 highlights the main features of our SSc population; in particular, the EmoLED® patients are compared with the control group.
No significant difference between the groups was recorded for treatments (iv prostanoids: p = 0.400; calcium channel blockers (CCBs): p = 0.307; endothelin receptor antagonists (ERAs): p = 0.307; phosphodiesterase-5 (PDE 5) inhibitors: p = 0.465; classic DMARDs: p = 0.465; biologic DMARDs: p = 0.600; analgesics: p = 0.612).
All skin lesions were localized on finger hands, mainly on fingertips. SU duration did not differ between the groups (p = 0.327). The features and response of the SU to EmoLED® treatment are reported in Tables 4 and 5.
The application of blue light PBM with EmoLED® apparently produced faster healing of the SU, with the formation of granulation tissue and regularization of margins, when used in addition to debridement. Complete healing of SU was recorded in 5/12 (41.6%) cases during EmoLED® treatment. In detail, improvements in SU area (p = 0.012), length (p = 0.008), and width (p = 0.001), wound bed re-epithelization (p = 0.019), and related pain (p = 0.054) were observed from T0 to T8 in EmoLED® patients. Control patients treated with standard systemic/local therapies merely showed amelioration of SU width (p = 0.039) and a trend toward an improvement in SU area (p = 0.088) at the end of the follow-up; see Tables 4 and 5.
At baseline, 1 patient in each group showed clear signs of infection; the involved bacteria were Staphylococcus aureus (1 case) and Escherichia coli (1 case). Systemic oral antibiotic therapy was required and no additional or relapsing infections were observed during the follow-up period in the EmoLED®-treated patient; in the control group, a relapse of SU infection was reported.
Furthermore, upon comparing the EmoLED® and control group patients from T0 to T8, we observed significant differences in SU exudate presence (3/12 vs. 6/8, p = 0.040) and perilesional skin assessment, in particular maceration/excoriation presence (1/12 vs 5/8, p = 0.018). Finally, EmoLED® treatment was well tolerated by all subjects, none of whom complained about any procedural or post-procedural adverse events from light irradiation. Subjects reported only a mild sensation of warmth. In Figs. 1 and 2 we show the EmoLED® device and the treatment efficacy in 1 patient with SU from baseline to the end of follow-up.
Discussion
The presence of skin ulcers may severely affect the quality of life of SSc patients; these ulcers have a significant impact on daily activities and ability to work, and they are associated with pain and disability. Frequently, SSc-SU become infected and resist standard treatments. Based on our experience, we have developed a holistic approach to SU treatment, from a global patient assessment to local and systemic SU treatment and innovative regenerative therapy [12,13,14,15]. Nevertheless, a significant percentage of scleroderma skin ulcers still represent a challenging clinical problem.
The results of our preliminary study encourage further investigations of the application of blue light photobiomodulation with EmoLED® as a potentially helpful additional treatment in the management of SSc-SU. EmoLED® therapy was associated with faster healing of SU when used in addition to standard treatments, in particular wound bed debridement. In our experience, complete healing of SU was recorded in 5 cases during PBM treatment, together with improvements in SU features, progression of edges, wound bed granulation, and integrity of the perilesional skin in the majority of SU. EmoLED® patients also reported an improvement in pain at the end of the follow-up in comparison with control subjects treated with standard systemic/local therapies alone. According to previous observations, the therapeutic strategy for SSc-SU has included both systemic and local pharmacological approaches, as well as a number of nonpharmacological procedures [9, 25, 28]. Integrated local treatments are often crucial to SSc-SU healing; these are mainly based on wound bed preparation as summarized in the TIME principles [10, 24, 29]. However, despite the application of integrated and innovative treatments, SSc-SU sometimes continue to be hard-to-heal lesions.
In this setting, searching for innovative therapies that support and promote ulcer healing is fundamental. Photobiomodulation (PBM) with blue light was recently investigated for the treatment of chronic wounds.
Light therapy has been used for years for healing and promoting health [18, 30]. Photobiomodulation (PBM) is the term used to describe the mechanistic/scientific basis for this photonic specialty, and photobiomodulation therapy (PBMT) is the term for its therapeutic application. It was first developed in the 1960s, but only in 2015 did the North American Association for Light Therapy and the World Association for Laser Therapy agree by consensus to promote PBM as a form of light treatment that utilizes nonionizing light sources and involves a nonthermal process and photochemical events at various biological scales. This treatment results in beneficial therapeutic effects, including the mitigation of pain or inflammation, immunomodulation, and promotion of wound healing and tissue regeneration [31]. In the 1990s, the introduction of high-efficiency LEDs revolutionized the lighting industry, including biomedical applications of light. The use of LEDs for PBM therapy has become more widespread, and its clinical effectiveness has been extensively illustrated [32]. In fact, many different conditions and fields of medical treatment are now becoming responsive to the beneficial effects of PBM [33].
Chronic wounds often stagnate in the inflammatory phase and/or experience an impaired proliferative phase. Wound healing is a dynamic process that involves several molecules, mediators, blood cells, parenchymal cells, and extracellular matrix [34]. Despite several reports, the exact mechanism underlying photobiomodulation and its role in wound healing promotion is a relatively new research area [16, 18].
A detailed review from Mosca et al. provides background on and studies evidence for the therapeutic application of light energy treatments for wound healing [18]. A range of light energy sources from LEDs to lasers have been used, with specific benefits and limitations. Noninvasive, economical, and multipurpose light tools represent challenging options for wound management. However, there is a lack of consensus on standardized treatment parameters, such as wavelengths, doses, and therapeutic outcomes in the reviewed studies. For that reason, there is an urgent need in the wound care community to establish clinical protocols and well-designed, rigorous research studies on this topic.
Based on various recent experiences in the field of PBM as an adjunct therapy in wound healing [35, 36], there is significant excitement in this research field.
PBM treatment was described as yielding promising results for many ischemic ulcers, mainly diabetic wounds [37, 38]. As regards to SSc, low-level light treatment (LTTT) for SSc digital ulcers was recently investigated by Hughes et al., who used three wavelengths (infrared, red, and violet from LEDs) in a novel custom-built device, achieved interesting results in terms of feasibility and safety, and tentatively proposed the use of this treatment for scleroderma digital ulcers [39].
Traditionally, red and near-infrared light have been used therapeutically; however, several reports indicate that other wavelengths within the visible spectrum could show advantageous effects, including blue and green light [40].
A systematic literature evaluation indicated that 72% of publications reported beneficial effects of blue light. Despite the increasing number of studies regarding the effect of blue light on tissues and cells, often only partial information is reported, and a clear understanding of the different approaches is rare [41, 42].
It is important to emphasize the need to assess exposure and treatment parameters in relation with extensive effects on a range of different chromophores within the body in order to better determine the full potential of PBM.
Blue LED light medical devices that use specific wavelengths in the blue range of the visible light spectrum have been extensively analyzed in animal models [17, 23], and the efficacy and safety of such devices have been demonstrated. Some authors have recently reported observations of an improved healing process when superficial wounds are treated with blue LED light with wavelengths in the range 410–430 nm, and a study in an animal model indicated that blue light led to a faster healing process in superficial lesions, with fibroblasts and myofibroblasts playing an important role [19]. After a critical literature review [22], further analyses of this group focused on the effects of blue light on fibroblasts and keratinocytes; it was observed that blue LED light may be used to modulate the metabolism and proliferation of human fibroblasts, and its effects on wound healing seemed to be particularly evident when studying fibroblast and keratinocyte co-cultures [20, 21].
In this research setting, the blue-light-emitting medical device EmoLED® was developed. The functioning of this medical device is based on light energy transfer from the tool to the patient, and the interaction of this light energy with some endogenous chromophores in the blood and skin is able to activate the photobiomodulation mechanism, stimulating the physiological processes of wound healing. Each chromophore has a different absorption spectrum and a different sensitivity to various wavelengths, which can produce varying photophysical and photochemical effects when they are absorbed by tissues. It is possible that blue light is absorbed by mitochondrial chromophores in the same way as red/infrared light; however, there are several other plausible chromophores for blue light. Because of the width of a typical absorption band, it is probable that blue light is absorbed by several distinct chromophores [43].
The B.L.U.R. study aimed to determine if blue light photobiomodulation with EmoLED® in addition to the standard of care was more effective than the standard of care alone in promoting re-epithelialization of chronic wounds of lower limbs. At week 10, the wounds treated with additional EmoLED® showed a smaller residual wound area compared to the lesions treated with the standard of care alone, especially for venous leg ulcers [27]. Also, Marchelli et al. recently described the use of this tool in patients affected by chronic wounds of different etiologies that did not respond to standard treatments. Of the 19 ulcers evaluated (venous, ischemic, post-traumatic, vasculitic), 84% responded to the treatment during the period of observation, and the treatment showed a good safety profile [44].
Several authors described the role of photobiomodulation in treating xerostomia in a pediatric patient affected by SSc. After this therapy, an increase in salivary flow and an improvement in mastication and swallowing were recorded [45]. Nevertheless, to our knowledge, this is the first study to report the effectiveness of EmoLED® treatment in the management of SSc-SU. The results of our preliminary report encourage further exploration of EmoLED® as a potentially helpful additional treatment in the management of SSc-SU. In our experience, the most favorable results were mainly observed for SU dimensions, signs of infections, and related pain without incurring adverse effects. In detail, the wound bed conditions rapidly improved, with reduced fibrin, growth of granulation tissue, re-epithelization of the edges, and infection control. Possible mechanisms for these beneficial effects on cutaneous wound healing and the restoration of the epidermal barrier have already been mentioned [16,17,18,19,20,21,22]. Low levels of blue light seem to stimulate the metabolic activity and differentiation of cultured keratinocytes, and opsin expression might be involved too. Dermal opsins have been identified in many animals as well as humans. Current evidence suggests that opsins have a biological role beyond light response. In nonhuman animals, opsins seem to be involved in processes crucial to survival. In humans, these receptors are involved in many skin functions in the epidermis and dermis, although the underlying molecular mechanisms remain elusive. Several reports have demonstrated that opsins modulate various physiological cutaneous processes, such as melanogenesis, photoaging, hair growth, and wound healing in terms of the newly regenerating epidermis following wounding. Since keratinocytes and fibroblasts retain their expression in culture, they could offer a valid model to better examine the mechanism for the response of wound healing to blue light [46, 47].
The present study has some limitations, which are mainly related to the small size of the enrolled SSc population. Larger randomized controlled trials are needed to further elucidate the potential clinical applications of photobiomodulation in the intriguing scenario of SSc-SU management.
Conclusions
In conclusion, the positive clinical results of this approach, along with the absence of significant side effects, suggest that EmoLED® could be a safe, effective, noninvasive tool to treat SSc-SU, with an interesting role to play in the healing process in addition to conventional systemic and local therapies.
References
Hachulla E, Launay D. Diagnosis and classification of systemic sclerosis. Clin Rev Allergy Immunol. 2011;40(2):78–83. https://doi.org/10.1007/s12016-010-8198-y (PMID: 20143182).
van den Hoogen F, Khanna D, Fransen J, Johnson SR, Baron M, Tyndall A, et al. 2013 Classification criteria for systemic sclerosis: an American College of Rheumatology/European League against Rheumatism collaborative initiative. Arthritis Rheumatol. 2013;65(11):2737–47.
Ferri C, Sebastiani M, Lo Monaco A, Iudici M, Giuggioli D, Furini F, et al. Systemic sclerosis evolution of disease pathomorphosis and survival. Our experience on Italian patients’ population and review of the literature. Autoimmun Rev. 2014;13(10):1026–34.
Steen V, Denton CP, Pope JE, Matucci-Cerinic M. Digital ulcers: overt vascular disease in systemic sclerosis. Rheumatology. 2009;48(Suppl 3):19–24.
Amanzi L, Braschi F, Fiori G, Galluccio F, Miniati I, Guiducci S, et al. Digital ulcers in scleroderma: staging, characteristics and sub-setting through observation of 1614 digital lesions. Rheumatology (Oxford). 2010;49:1374–82.
Giuggioli D, Manfredi A, Colaci M, Lumetti F, Ferri C. Scleroderma digital ulcers complicated by infection with fecal pathogens. Arthritis Care Res (Hoboken). 2011;64:295–7.
Giuggioli D, Manfredi A, Vacchi C, Sebastiani M, Spinella A, Ferri C. Procedural pain management in the treatment of scleroderma digital ulcers. Clin Exp Rheumatol. 2015;33:5–10.
Matucci-Cerinic M, Krieg T, Guillevin L, Schwierin B, Rosenberg D, Cornelisse P, et al. Elucidating the burden of recurrent and chronic digital ulcers in systemic sclerosis: long-term results from the DUO Registry. Ann Rheum Dis. 2016;75:1770–6.
Giuggioli D, Manfredi A, Lumetti F, Colaci M, Ferri C. Scleroderma skin ulcers definition, classification and treatment strategies our experience and review of the literature. Autoimmun Rev. 2018;17:155–64.
Schultz GS, Sibbald RG, Falanga V, Ayello EA, Dowsett C, Harding K, et al. Wound bed preparation: a systematic approach to wound management. Wound Repair Regen. 2003;11:S1-28.
Kowal-Bielecka O, Landewé R, Avouac J, Chwiesko S, Miniati I, Czirjak L, et al. EULAR recommendations for the treatment of systemic sclerosis: a report from the EULAR Scleroderma Trials and Research Group (EUSTAR). Ann Rheum Dis. 2009;68:620–8.
Giuggioli D, Lumetti F, Spinella A, Cocchiara E, Sighinolfi G, Citriniti G, et al. Use of neem oil and Hypericum perforatum for treatment of calcinosis-related skin ulcers in systemic sclerosis. J Int Med Res. 2020;48(4):300060519882176.
Pignatti M, Spinella A, Cocchiara E, Boscaini G, Lusetti IL, Citriniti G, et al. Autologous fat grafting for the oral and digital complications of systemic sclerosis: results of a prospective study. Aesthet Plast Surg. 2020;44(5):1820–32.
Pignatti M, Spinella A, Cocchiara E, Boscaini G, Lusetti IL, Citriniti G, et al. Invited response on: Comments on “Autologous fat grafting for the oral and digital complications of systemic sclerosis: results of a prospective study.” Aesthet Plast Surg. 2021;45(3):1344–5.
Giuggioli D, Spinella A, Cocchiara E, de Pinto M, Pinelli M, Parenti L, et al. Autologous fat grafting in the treatment of a scleroderma stump-skin ulcer: a case report. Case reports. Plast Surg Hand Surg. 2021;8(1):18–22.
Kuffler DP. Photobiomodulation in promoting wound healing: a review. Regen Med. 2016;11(1):107–22. https://doi.org/10.2217/rme.15.82 (Epub 2015 Dec 18 PMID: 26681143).
Cicchi R, Rossi F, Alfieri D, Bacci S, Tatini F, De Siena G. Observation of an improved healing process in superficial skin wounds after irradiation with a blue-LED haemostatic device. J Biophotonics. 2016;9(6):645–55.
Mosca RC, Ong AA, Albasha O, Bass K, Arany P. Photobiomodulation therapy for wound care: a potent, noninvasive photoceutical approach. Adv Skin Wound Care. 2019;32(4):157–67.
Magni G, Tatini F, Bacci S, Paroli G, De Siena G, Cicchi R, et al. Blue LED light modulates inflammatory infiltrate and improves the healing of superficial wounds. Photodermatol Photoimmunol Photomed. 2020;36(2):166–8.
Magni G, Banchelli M, Cherchi F, Coppi E, Fraccalvieri M, Rossi M, et al. Experimental study on blue light interaction with human keloid-derived fibroblasts. Biomedicines. 2020;8(12):573.
Rossi F, Magni G, Tatini F, Banchelli M, Cherchi F, Rossi M, et al. Photobiomodulation of human fibroblasts and keratinocytes with blue light: implications in wound healing. Biomedicines. 2021;9(1):41.
de Abreu PTR, de Arruda JAA, Mesquita RA, Abreu LG, Diniz IMA, Silva TA. Photobiomodulation effects on keratinocytes cultured in vitro: a critical review. Lasers Med Sci. 2019;34(9):1725–34.
Lopez A, Brundage C. Wound photobiomodulation treatment outcomes in animal models. J Vet Med. 2019;28(2019):6320515.
Leaper DJ, Schultz G, Carville K, Fletcher J, Swanson T, Drake R. Extending the TIME concept: what have we learned in the past 10 years? Int Wound J. 2012;9(Suppl 2):1–19.
Denton CP, Hughes M, Gak N, Vila J, Buch MH, Chakravarty K, et al. BSR and BHPR Standards, Guidelines and Audit Working Group. BSR and BHPR guideline for the treatment of systemic sclerosis. Rheumatology (Oxford). 2016;55:1906–10.
Dini V, Romanelli M, Oranges T, Davini G, Janowska A. Blue light emission in the management of hard-to-heal wounds. Ital J Dermatol Venerol. 2021;156(6):709–13.
Fraccalvieri M, Amadeo G, Bortolotti P, Ciliberti M, Garrubba A, Mosti G et al. Effectiveness of blue light photobiomodulation therapy in the treatment of chronic wounds. Results of the Blue Light for Ulcer Reduction (B.L.U.R.) Study. Ital J Dermatol Venerol. 2021.
Galluccio F, Allanore Y, Czirjak L, Furst DE, Khanna D, Matucci-Cerinic M. Points to consider for skin ulcers in systemic sclerosis. Rheumatology (Oxford). 2017;56:v67-71.
Fujimoto M, Asano Y, Ishii T, Ogawa F, Kawakami T, Kodera M, et al. The wound/burn guidelines—4: guidelines for the management of skin ulcers associated with connective tissue disease/vasculitis. J Dermatol. 2016;43:729–57.
Grzybowski A, Sak J, Pawlikowski J. A brief report on the history of phototherapy. Clin Dermatol. 2016;34(5):532–7.
Anders JJ, Lanzafame RJ, Arany PR. Low-level light/laser therapy versus photobiomodulation therapy. Photomed Laser Surg. 2015;33(4):183–4.
Zhu Y, Xu G, Yuan J, Jo J, Gandikota G, Demirci H, et al. Light emitting diodes based photoacoustic imaging and potential clinical applications. Sci Rep. 2018;8(1):9885.
Hamblin MR, de Sousa MVP, Agrawal T. Handbook of low-level laser therapy. New York: Pan Stanford; 2016.
Martin P. Wound healing—aiming for perfect skin regeneration. Science. 1997;276(5309):75–81.
Nair HKR, Chong SSY, Selvaraj DDJ. Photobiomodulation as an adjunct therapy in wound healing. Int J Low Extreme Wounds. 2021;11:15347346211004186.
Mosca RC, Santos SN, Nogueira GEC, Pereira DL, Costa FC, Pereira JX, et al. The efficacy of photobiomodulation therapy in improving tissue resilience and healing of radiation skin damage. Photonics. 2022;9(1):10.
Maiya AG, Kumar AS, Hazari A, Jadhav R, Ramachandra L, Hande HM, Rajgopal SK, et al. Photobiomodulation therapy in neuroischaemic diabetic foot ulcers: a novel method of limb salvage. J Wound Care. 2018;27(12):837–42.
Ahmadi H, Amini A, FadaeiFathabady F, Mostafavinia A, Zare F, Ebrahimpour-Malekshah R, et al. Transplantation of photobiomodulation-preconditioned diabetic stem cells accelerates ischemic wound healing in diabetic rats. Stem Cell Res Ther. 2020;11(1):494.
Hughes M, Moore T, Manning J, Wilkinson J, Watson S, Samraj P, et al. A feasibility study of a novel low-level light therapy for digital ulcers in systemic sclerosis. J Dermatol Treat. 2019;30(3):251–7.
Serrate H, Heiskanen V, Palin WM, Cooper PR, Milward MR, Hadis M, et al. Under the spotlight: mechanisms of photobiomodulation concentrating on blue and green light. Photochem Photobiol Sci. 2019;18(8):1877–909.
Masson-Meyers DS, Bumah VV, Biener G, Raicu V, Enwemeka CS. The relative antimicrobial effect of blue 405 nm LED and blue 405 nm laser on methicillin-resistant Staphylococcus aureus in vitro. Lasers Med Sci. 2015;30(9):2265–71.
Niu T, Tian Y, Cai Q, Ren Q, Wei L. Red light combined with blue light irradiation regulates proliferation and apoptosis in skin keratinocytes in combination with low concentrations of curcumin. PLoS One. 2015;10(9).
Hamblin MR. Mechanisms and mitochondrial redox signaling in photobiomodulation. Photochem Photobiol. 2018;94(2):199–212.
Marchelli M, Perniciaro G, Granara D, et al. Photobiomodulation with blue light in non-healing wounds: case series evaluation. Wounds Int. 2019;10(3):63–6.
de Oliveira AB, Ferrisse TM, Salomão KB, Miranda ML, Bufalino A, Brighenti FL. Photobiomodulation in the treatment of xerostomia associated with hyposalivation in a pediatric patient with systemic scleroderma. Autops Case Rep. 2020;11:e2020220.
Castellano-Pellicena I, Uzunbajakava NE, Mignon C, Raafs B, Botchkarev VA, Thornton MJ. Does blue light restore human epidermal barrier function via activation of opsin during cutaneous wound healing? Lasers Surg Med. 2019;51(4):370–82.
Suh S, Choi EH, Atanaskova MN. The expression of opsins in the human skin and its implications for photobiomodulation: a systematic review. Photodermatol Photoimmunol Photomed. 2020;36(5):329–38.
Acknowledgements
We thank the participants of the study.
Funding
No funding or sponsorship was received for this study or the publication of this article. The Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All listed authors (Amelia Spinella, Marco de Pinto, Claudio Galluzzo, Sofia Testoni, Pierluca Macripò, Federica Lumetti, Luca Parenti, Luca Magnani, Gilda Sandri, Gianluigi Bajocchi, Marta Starnoni, Giorgio De Santis, Carlo Salvarani, Dilia Giuggioli) equally contributed to the development of the study, with particular regard to the concept and study design, statistical analysis, and substantial drafting of the manuscript.
Disclosures
All listed authors (Amelia Spinella, Marco de Pinto, Claudio Galluzzo, Sofia Testoni, Pierluca Macripò, Federica Lumetti, Luca Parenti, Luca Magnani, Gilda Sandri, Gianluigi Bajocchi, Marta Starnoni, Giorgio De Santis, Carlo Salvarani, Dilia Giuggioli) have nothing to disclose.
Compliance with Ethics Guidelines
The study was approved by the local ethics committee Area Vasta Emilia Nord (protocol no. 275/16), and written informed consent was obtained from all participants. The study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Spinella, A., de Pinto, M., Galluzzo, C. et al. Photobiomodulation Therapy: A New Light in the Treatment of Systemic Sclerosis Skin Ulcers. Rheumatol Ther 9, 891–905 (2022). https://doi.org/10.1007/s40744-022-00438-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-022-00438-9