Abstract
Purpose of Review
The Jenkins Sleep Scale (JSS) is a widely used self-report measure for assessing sleep difficulties. While the original English version of the JSS has demonstrated sound psychometric properties, research on translated versions is limited. We conducted a reliability generalization meta-analysis to systematically review and quantify the internal consistency and test–retest reliability of the JSS across all available translations.
Recent Findings
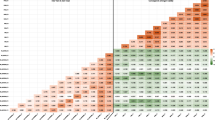
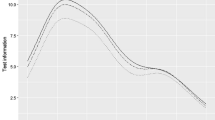
A systematic literature review identified k = 12 studies involving 90,173 participants reporting reliability statistics for eight different language versions of the JSS. Random-effects meta-analysis found acceptable mean internal consistency (α = 0.80) and excellent test–retest reliability (r = 0.93) across translations. Moderator analyses revealed that participant characteristics and demographics did not affect the results.
Summary
The findings support the cross-language utility of the scale but highlight the importance of high-quality translation procedures, particularly when assessing stability over time. Recommendations are provided to guide future worldwide adaptation, validation, and clinical use of the JSS.







Similar content being viewed by others
Data Availability
Data are made available in supplemental materials File 40675_2024_292_MOESM3_ESM.txt.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Krystal AD, Prather AA, Ashbrook LH. The assessment and management of insomnia: an update. World Psychiatry. 2019;18(3):337–52. https://doi.org/10.1002/wps.20674.
Fabbri M, Beracci A, Martoni M, Meneo D, Tonetti L, Natale V. Measuring subjective sleep quality: a review. Int J Environ Res Public Health. 2021;18(3). https://doi.org/10.3390/ijerph18031082.
Wardle-Pinkston S, Slavish DC, Taylor DJ. Insomnia and cognitive performance: a systematic review and meta-analysis. Sleep Med Rev. 2019;48: 101205.
Rémi J, Pollmächer T, Spiegelhalder K, Trenkwalder C, Young P. Sleep-related disorders in neurology and psychiatry. Dtsch Arztebl Int. 2019;116(41):681–8. https://doi.org/10.3238/arztebl.2019.0681.
Fekih-Romdhane F, Hallit S, Cheour M, Jahrami H. The nature, consequences, mechanisms, and management of sleep disturbances in individuals at-risk for psychosis. Front Psychiatry. 2022;13:1011963. https://doi.org/10.3389/fpsyt.2022.1011963.
Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiat. 2016;80(1):40–52.
Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32(12):1484–92.
Grandner MA, Patel NP. From sleep duration to mortality: implications of meta-analysis and future directions. J Sleep Res. 2009;18(2):145.
Ballesio A, Zagaria A, Baccini F, Micheli F, Di Nardo G, Lombardo C. A meta-analysis on sleep quality in inflammatory bowel disease. Sleep Med Rev. 2021;60: 101518.
Sella E, Miola L, Toffalini E, Borella E. The relationship between sleep quality and quality of life in aging: a systematic review and meta-analysis. Health Psychol Rev. 2023;17(1):169–91.
Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18(2):148–58.
Litwiller B, Snyder LA, Taylor WD, Steele LM. The relationship between sleep and work: a meta-analysis. J Appl Psychol. 2017;102(4):682.
Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bögels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: a meta-analytic review. Sleep Med Rev. 2010;14(3):179–89.
Musshafen LA, Tyrone RS, Abdelaziz A, Sims-Gomillia CE, Pongetti LS, Teng F, et al. Associations between sleep and academic performance in US adolescents: a systematic review and meta-analysis. Sleep Med. 2021;83:71–82.
Bowers JM, Moyer A. Effects of school start time on students’ sleep duration, daytime sleepiness, and attendance: a meta-analysis. Sleep Health. 2017;3(6):423–31.
Boardman JM, Porcheret K, Clark JW, Andrillon T, Cai AW, Anderson C, et al. The impact of sleep loss on performance monitoring and error-monitoring: a systematic review and meta-analysis. Sleep Med Rev. 2021;58: 101490.
Moradi A, Nazari SSH, Rahmani K. Sleepiness and the risk of road traffic accidents: a systematic review and meta-analysis of previous studies. Transport Res F: Traffic Psychol Behav. 2019;65:620–9.
Manzar MD, Jahrami HA, Bahammam AS. Structural validity of the Insomnia Severity Index: a systematic review and meta-analysis. Sleep Med Rev. 2021;60: 101531. https://doi.org/10.1016/j.smrv.2021.101531.
Jenkins CD, Stanton BA, Niemcryk SJ, Rose RM 1988 A scale for the estimation of sleep problems in clinical research. J Clin Epidemiol. 41(4):313–21. https://doi.org/10.1016/0895-4356(88)90138-2. This study provided data to the meta-analysis of the Internal Consistency and Test-Retest Reliability of the Jenkins Sleep Scale Across International Versions.
Reis C, Mestre C, Tecedeiro MMV, Paiva T. Translation, cross-cultural adaptation and psychometric properties of the Jenkins Sleep Scale in a sample of Portuguese shift workers. Laboratório de Psicologia. 2014;12:89–98. This study provided data to the meta-analysis of the Internal Consistency and Test-Retest Reliability of the Jenkins Sleep Scale Across International Versions. https://doi.org/10.14417/lp.894.
Salman M, Khan AH, Sulaiman SAS, Saleem F, Asif N, Mustafa ZU, et al. Psychometric validation of the Urdu version of the Jenkins sleep evaluation questionnaire. Journal of Pharmacy Practice and Community Medicine. 2018;4(1). This study provided data to the meta-analysis of the Internal Consistency and Test-Retest Reliability of the Jenkins Sleep Scale Across International Versions. https://doi.org/10.5530/jppcm.2018.1.2.
Duruöz MT, Ünal Ç, Ulutatar F, Sanal Toprak C, Gündüz OH. The validity and reliability of Turkish version of the Jenkins sleep evaluation scale in rheumatoid arthritis. Arch Rheumatol. 2018;33(2):160–7. https://doi.org/10.5606/ArchRheumatol.2018.6376. This study provided data to the meta-analysis of the Internal Consistency and Test-Retest Reliability of the Jenkins Sleep Scale Across International Versions.
Duruöz MT, Erdem D, Gencer K, Ulutatar F, Baklacıoğlu H. Validity and reliability of the Turkish version of the Jenkins Sleep Scale in psoriatic arthritis. Rheumatol Int. 2018;38(2):261–5. https://doi.org/10.1007/s00296-017-3911-2. This study provided data to the meta-analysis of the Internal Consistency and Test-Retest Reliability of the Jenkins Sleep Scale Across International Versions. https://doi.org/10.1007/s00296-017-3911-2.
Duruoz MT, Ulutatar F, Ozturk EC, Unal-Ulutatar C, Sanal Toprak C, Kayhan O. Assessment of the validity and reliability of the Jenkins Sleep Scale in ankylosing spondylitis. Int J Rheum Dis. 2019;22(2):275–9. https://doi.org/10.1111/1756-185x.13447. This study provided data to the meta-analysis of the Internal Consistency and Test-Retest Reliability of the Jenkins Sleep Scale Across International Versions.
Pallarés-Sanmartín A, Gonzalez FJC, Fiorentino F, Crespo MG. Validation of the sleep Jenkins questionnaire (SJQ) into Spanish: assessment of quality of sleep in patients with asthma. Chest. 2019;156(4):A1715. This study provided data to the meta-analysis of the Internal Consistency and Test-Retest Reliability of the Jenkins Sleep Scale Across International Versions. https://doi.org/10.1016/j.chest.2019.08.1501.
Tibubos AN, Zenger M, Schmalbach B, Beutel ME, Brähler E. Measurement invariance, validation and normative data of the Jenkins Sleep Scale-4 (JSS-4) in the German general population across the life span. J Psychosom Res. 2020;130:109933. https://doi.org/10.1016/j.jpsychores.2020.109933. This study provided data to the meta-analysis of the Internal Consistency and Test-Retest Reliability of the Jenkins Sleep Scale Across International Versions.
• Unal-Ulutatar C, Ozsoy-Unubol T. Psychometric properties of Turkish version of Jenkins sleep scale in fibromyalgia syndrome. Adv Rheumatol. 2020;60(1):22. https://doi.org/10.1186/s42358-020-0123-3. This study provided data to the meta-analysis of the Internal Consistency and Test-Retest Reliability of the Jenkins Sleep Scale Across International Versions.
Juhola J, Arokoski JPA, Ervasti J, Kivimäki M, Vahtera J, Myllyntausta S, et al. Internal consistency and factor structure of Jenkins Sleep Scale: cross-sectional cohort study among 80 000 adults. BMJ Open. 2021;11(1):e043276. https://doi.org/10.1136/bmjopen-2020-043276. This study provided data to the meta-analysis of the Internal Consistency and Test-Retest Reliability of the Jenkins Sleep Scale Across International Versions.
Villarreal-Zegarra D, Torres-Puente R, Otazú-Alfaro S, Al-Kassab-Córdova A, Rey de Castro J, Mezones-Holguín E. Spanish version of Jenkins Sleep Scale in physicians and nurses: psychometric properties from a Peruvian nationally representative sample. J Psychosom Res. 2022;157:110759. https://doi.org/10.1016/j.jpsychores.2022.110759. This study provided data to the meta-analysis of the Internal Consistency and Test-Retest Reliability of the Jenkins Sleep Scale Across International Versions.
eProvide: https://eprovide.mapi-trust.org/instruments/jenkins-sleep-evaluation-questionnaire (2023). Accessed October 1 2023.
Sánchez-Meca J, Marín-Martínez F, López-López JA, Núñez-Núñez RM, Rubio-Aparicio M, López-García JJ, et al. Improving the reporting quality of reliability generalization meta-analyses: the REGEMA checklist. Res Synth Methods. 2021;12(4):516–36. https://doi.org/10.1002/jrsm.1487.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71. https://doi.org/10.1136/bmj.n71.
Mokkink LB, Prinsen CA, Bouter LM, Vet HC, Terwee CB. The COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) and how to select an outcome measurement instrument. Braz J Phys Ther. 2016;20(2):105–13. https://doi.org/10.1590/bjpt-rbf.2014.0143.
McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12(1):55–61. https://doi.org/10.1002/jrsm.1411.
Doi SA, Thalib L. A quality-effects model for meta-analysis. Epidemiology. 2008;19(1):94–100. https://doi.org/10.1097/EDE.0b013e31815c24e7.
Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11(2):193.
Baker WL, Michael White C, Cappelleri JC, Kluger J, Coleman CI, From the Health Outcomes P, et al. Understanding heterogeneity in meta-analysis: the role of meta-regression. Int J Clin Pract. 2009;63(10):1426–34.
Viechtbauer W, Cheung MW. Outlier and influence diagnostics for meta-analysis. Res Synth Methods. 2010;1(2):112–25. https://doi.org/10.1002/jrsm.11.
Viechtbauer W, Viechtbauer MW. Package ‘metafor’. The Comprehensive R Archive Network Package ‘metafor’ https://cranr-projectorg/web/packages/metafor/metaphor.pdf. 2015.
Morris CN. Parametric empirical Bayes inference: theory and applications. J Am Stat Assoc. 1983;78(381):47–55. https://doi.org/10.1080/01621459.1983.10477920.
Sterne JA, Becker BJ, Egger M. The funnel plot. Publication bias in meta‐analysis: prevention, assessment and adjustments. 2005:73–98. https://doi.org/10.1002/0470870168.ch5
Schwarzer G. meta: an R package for meta-analysis. R news. 2007;7(3):40–5.
Cerri LQ, Justo MC, Clemente V, Gomes AA, Pereira AS, Marques DR. Insomnia Severity Index: a reliability generalisation meta-analysis. J Sleep Res. 2023;32(4): e13835. https://doi.org/10.1111/jsr.13835.
Jahrami H, Trabelsi K, Saif Z, Manzar MD, BaHammam AS, Vitiello MV. Reliability generalization meta-analysis of the Athens Insomnia Scale and its translations: examining internal consistency and test-retest validity. Sleep Med. 2023;111:133–45. https://doi.org/10.1016/j.sleep.2023.09.015.
Gonçalves MT, Malafaia S, Moutinho Dos Santos J, Roth T, Marques DR. Epworth sleepiness scale: a meta-analytic study on the internal consistency. Sleep Med. 2023;109:261–9. https://doi.org/10.1016/j.sleep.2023.07.008.
Hofmeister D, Schulte T, Hinz A. Sleep problems in cancer patients: a comparison between the Jenkins Sleep Scale and the single-item sleep scale of the EORTC QLQ-C30. Sleep Med. 2020;71:59–65. https://doi.org/10.1016/j.sleep.2019.12.033.
Author information
Authors and Affiliations
Contributions
HJ and ZS designed the review and performed literature search and data extraction. KT and HG validated the data. HJ performed all analyses. HJ, KT, HG, SRT, and MVV wrote the manuscript. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the original authors have been previously published and complied with all applicable ethical standards (including the Helsinki Declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlight
• The Jenkins Sleep Scale (JSS) has excellent test-retest reliability across languages.
• Participant demographics did not affect reliability results.
• Recommendations are provided to guide future adaptation and validation of the worldwide use of this sleep instrument.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jahrami, H., Trabelsi, K., Ghazzawi, H. et al. Internal Consistency and Test–Retest Reliability of the Jenkins Sleep Scale Across International Versions: A Reliability Generalization Meta-analysis. Curr Sleep Medicine Rep (2024). https://doi.org/10.1007/s40675-024-00292-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s40675-024-00292-x