Abstract
Purpose of Review
Nightmares, vivid and distressing dreams leading to arousal, can significantly impact sleep and daytime functioning. Nightmare disorder can occur with or without psychiatric disorders and with or without a traumatic event. Effective management of nightmares is crucial not only for nightmare disorder but also to prevent the worsening of psychiatric disorders or complications, such as suicide. This review explores the range of available treatments, encompassing both pharmacological and non-pharmacological, for nightmare disorders and trauma-associated nightmares.
Recent Findings
Different interventions have shown their safety and effectiveness in the therapeutic management of nightmares, such as imagery rehearsal therapy; exposure, relaxation, and rescripting therapy; lucid dreaming therapy; desensitization and exposure therapy; self-exposure therapy; and Prazosin.
Summary
Imagery rehearsal therapy (IRT) stands out with robust evidence supporting its effectiveness in nightmare disorder as well as in trauma-associated nightmares and should be considered as a first-line choice for therapeutic management of nightmares. This psychotherapeutic intervention employs cognitive and behavioral techniques and involves practicing mental imagery during daytime to modify the content of nightmares. This review summarizes the core principles of IRT and presents comprehensive guidelines for clinical practice.


Similar content being viewed by others
Abbreviations
- AASM:
-
American Academy of Sleep Medicine
- CAPS:
-
Clinician-Administered PTSD Scale
- CBT:
-
Cognitive behavioral therapy
- CBT-I:
-
Cognitive behavioral therapy for insomnia
- CNS:
-
Central nervous system
- DDNSI:
-
Disturbing Dreams and Nightmare Severity Index
- DSM:
-
Diagnostic and statistical manual of mental disorders
- EMDR:
-
Eye movement desensitization and reprocessing
- ERRT:
-
Exposure, relaxation, and rescripting therapy
- HNQ:
-
Hamburg Nightmare Questionnaire
- ICSD:
-
International Classification of Sleep Disorders
- IRT:
-
Imagery rehearsal therapy
- LDT:
-
Lucid dreaming therapy
- MADRE:
-
Mannheim Dream Questionnaire
- NDIQ:
-
Nightmare Distress And Impact Questionnaire
- NDQ:
-
Nightmare Distress Questionnaire
- NFQ:
-
Nightmare Frequency Questionnaire
- NES:
-
Nightmare Effects Survey
- NREM sleep:
-
Non-rapid eye movement sleep
- NSI:
-
Nightmare severity index
- PSQI:
-
Pittsburgh Sleep Quality Index
- PTSD:
-
Post-traumatic stress disorder
- RCT:
-
Randomized controlled trial
- REM sleep:
-
Rapid eye movement sleep
- TRNS:
-
Trauma-Related Nightmare Survey
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
American Psychiatric Association (APA). DSM Library. 2013. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). https://doi.org/10.1176/appi.books.9780890425787
American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed. 2014. https://scholar.google.com/scholar_lookup?title=International+Classification+of+Sleep+Disorders&publication_year=2014&. Accessed 20 Sept 2023.
Spoormaker V. A cognitive model of recurrent nightmares. Int J Dream Res. 2008;1(1):15–22.
Gieselmann A, Ait Aoudia M, Carr M, Germain A, Gorzka R, Holzinger B, et al. Aetiology and treatment of nightmare disorder: state of the art and future perspectives. J Sleep Res. 2019;28(4):e12820.
Blaskovich B, Reichardt R, Gombos F, Spoormaker VI, Simor P. Cortical hyperarousal in NREM sleep normalizes from pre- to post-REM periods in individuals with frequent nightmares. Sleep. 2020;43(1):zsz201.
Sayk C, Saftien S, Koch N, HVV N, Junghanns K, Wilhelm I. Cortical hyperarousal in individuals with frequent nightmares. J Sleep Res. 2023;e14003. https://doi.org/10.1111/jsr.14003. This study presents cortical hyperarousal as a trait marker in patients with chronic nightmares, which can be modified by IRT
Sandman N, Valli K, Kronholm E, Ollila HM, Revonsuo A, Laatikainen T, et al. Nightmares: prevalence among the Finnish general adult population and war veterans during 1972-2007. Sleep. 2013;36(7):1041–50.
Schredl M. Nightmare frequency and nightmare topics in a representative German sample. Eur Arch Psychiatry Clin Neurosci. 2010;260(8):565–70.
Kerkhof GA. Epidemiology of sleep and sleep disorders in The Netherlands. Sleep Med. 2017;30:229–39.
Li SX, Zhang B, Li AM, Wing YK. Prevalence and correlates of frequent nightmares: a community-based 2-phase study. Sleep. 2010;33(6):774–80.
Akkaoui MA, Lejoyeux M, d’Ortho MP, Geoffroy PA. Nightmares in patients with major depressive disorder, bipolar disorder, and psychotic disorders: a systematic review. J Clin Med. 2020;9(12):3990. In psychiatric disorders, nightmare distress was associated with disorder severity and nightmare frequency was associated with suicidal behaviors
Ambar Akkaoui M, D’ortho MP, Gourevitch R, Pham-Scottez A, Benhamou P, Atoui Y, et al. A study of nightmares in patients with psychiatric disorders. Psychiatry Clin Neurosci. 2022 Mar;76(3):89–91. Chronic nightmares are highly prevalent in psychiatric disorders other than PTSD
Swart ML, van Schagen AM, Lancee J, van den Bout J. Prevalence of nightmare disorder in psychiatric outpatients. Psychother Psychosom. 2013;82(4):267–8.
Woodward SH, Arsenault NJ, Murray C, Bliwise DL. Laboratory sleep correlates of nightmare complaint in PTSD inpatients. Biol Psychiatry. 2000;48(11):1081–7.
Krakow B, Hollifield M, Schrader R, Koss M, Tandberg D, Lauriello J, et al. Nightmare Frequency Questionnaire. 2019. https://doi.org/10.1037/t72712-000
Krakow B, Schrader R, Tandberg D, Hollifield M, Koss MP, Yau CL, et al. Nightmare frequency in sexual assault survivors with PTSD. J Anxiety Disord. 2002;16(2):175–90.
Schredl M, Berres S, Klingauf A, Schellhaas S, Göritz AS. The Mannheim Dream Questionnaire (MADRE): retest reliability, age and gender effects. Int J Dream Res. 2014;7(2):141–7.
Gorzka RJ, Rebling K, Höllmer H, Schulz H, Knaust T, Protic S, et al. Psychometric evaluation of the Hamburg Nightmare Questionnaire (HNQ). Eur J Psychotraumatol. 2019;10(1):1592393.
Kelly WE, Mathe JR. A brief self-report measure for frequent distressing nightmares: the Nightmare Experience Scale (NExS). Dreaming. 2019;29(2):180–95.
Dietch JR, Taylor DJ, Pruiksma K, Wardle-Pinkston S, Slavish DC, Messman B, et al. The Nightmare Disorder Index: development and initial validation in a sample of nurses. Sleep. 2021;44(5):zsaa254.
Geoffroy PA, Stern E, Maruani J, Cornic R, Bazin B, Clerici E, et al. The nightmare severity index (NSI): a short new multidimensional tool for assessing nightmares. J Sleep Res. 2023;e14065. https://doi.org/10.1111/jsr.14065. Dreams alterations and nightmares may be prodromal signs of suicidal crisis
Schredl M. Questionnaires and diaries as research instruments in dream research: Methodological issues. Dreaming. 2002;12(1):17–26.
Cranston CC, Miller KE, Davis JL, Rhudy JL. Preliminary validation of a brief measure of the frequency and severity of nightmares: the Trauma-Related Nightmare Survey. J Trauma Dissociation. 2017;18(1):88–99.
Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a Clinician-Administered PTSD Scale. J Trauma Stress. 1995;8(1):75–90.
Spoormaker VI, Schredl M, van den Bout J. Nightmares: from anxiety symptom to sleep disorder. Sleep Med Rev. 2006;10(1):19–31.
Pigeon WR, Campbell CE, Possemato K, Ouimette P. Longitudinal relationships of insomnia, nightmares, and PTSD severity in recent combat veterans. J Psychosom Res. 2013;75(6):546–50.
Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. 2012;73(9):e1160–7.
Faccini J, Joshi V, Graziani P, Del-Monte J. Non-constructive ruminations, insomnia and nightmares: trio of vulnerabilities to suicide risk. Nat Sci Sleep. 2022;14:433–41.
Bernert RA, Joiner TE, Cukrowicz KC, Schmidt NB, Krakow B. Suicidality and sleep disturbances. Sleep. 2005;28(9):1135–41.
Tanskanen A, Tuomilehto J, Viinamäki H, Vartiainen E, Lehtonen J, Puska P. Nightmares as predictors of suicide. Sleep. 2001;24(7):844–7.
Fisher HL, Lereya ST, Thompson A, Lewis G, Zammit S, Wolke D. Childhood parasomnias and psychotic experiences at age 12 years in a United Kingdom birth cohort. Sleep. 2014;37(3):475–82.
Geoffroy PA, Borand R, Ambar Akkaoui M, Yung S, Atoui Y, Fontenoy E, et al. Bad dreams and nightmares preceding suicidal behaviors. J Clin Psychiatry. 2022;84(1):22m14448. Nightmare Severity Index (NSI) is a new tool that can be used to assess frequency, emotional impact, diurnal impact, and nocturnal impact of nightmares
Aurora RN, Zak RS, Auerbach SH, Casey KR, Chowdhuri S, Karippot A, et al. Best practice guide for the treatment of nightmare disorder in adults. J Clin Sleep Med. 2010;6(4):389–401.
Morgenthaler TI, Auerbach S, Casey KR, Kristo D, Maganti R, Ramar K, et al. Position paper for the treatment of nightmare disorder in adults: an American Academy of Sleep Medicine position paper. J Clin Sleep Med. 2018;14(6):1041–55.
Krakow B, Hollifield M, Johnston L, Koss M, Schrader R, Warner TD, et al. Imagery rehearsal therapy for chronic nightmares in sexual assault survivors with posttraumatic stress disorder: a randomized controlled trial. JAMA. 2001;286(5):537–45.
Krakow B, Kellner R, Pathak D, Lambert L. Long term reduction of nightmares with imagery rehearsal treatment. Behav Cogn Psychother. 1996;24(2):135–48.
Kellner R, Neidhardt J, Krakow B, Pathak D. Changes in chronic nightmares after one session of desensitization or rehearsal instructions. Am J Psychiatry. 1992;149(5):659–63.
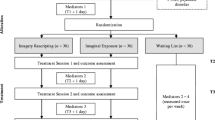
Schmid C, Hansen K, Kröner-Borowik T, Steil R. Imagery rescripting and imaginal exposure in nightmare disorder compared to positive imagery: a randomized controlled trial. Psychother Psychosom. 2021;90(5):328–40. This study shows that positive imagery alone has an effect on nightmares distress and frequency
Davis JL, Wright DC. Randomized clinical trial for treatment of chronic nightmares in trauma-exposed adults. J Trauma Stress. 2007;20(2):123–33.
Davis JL, Rhudy JL, Pruiksma KE, Byrd P, Williams AE, McCabe KM, et al. Physiological predictors of response to exposure, relaxation, and rescripting therapy for chronic nightmares in a randomized clinical trial. J Clin Sleep Med. 2011;7(6):622–31.
Pruiksma KE, Cranston CC, Rhudy JL, Micol RL, Davis JL. Randomized controlled trial to dismantle exposure, relaxation, and rescripting therapy (ERRT) for trauma-related nightmares. Psychol Trauma. 2018;10(1):67–75.
Spoormaker VI, van den Bout J. Lucid dreaming treatment for nightmares: a pilot study. Psychother Psychosom. 2006;75(6):389–94.
Holzinger B, Klösch G, Saletu B. Studies with lucid dreaming as add-on therapy to Gestalt therapy. Acta Neurol Scand. 2015;131(6):355–63.
Holzinger B, Saletu B, Klösch G. Cognitions in sleep: lucid dreaming as an intervention for nightmares in patients with posttraumatic stress disorder. Front Psychol. 2020;(11):1826. This RCT describes the effects of lucid dreaming therapy in trauma-related nightmares
Hamilton NA, Russell JA, Youngren WA, Gallegos AM, Crean HF, Cerulli C, et al. CBT-I treatment attrition in patients with weekly nightmares. J Clin Sleep Med. 2023;19(11):1913–21.
Cellucci AJ, Lawrence PS. The efficacy of systematic desensitization in reducing nightmares. J Behav Ther Exp Psychiatry. 1978;9(2):109–14.
Kunze AE, Arntz A, Morina N, Kindt M, Lancee J. Efficacy of imagery rescripting and imaginal exposure for nightmares: a randomized wait-list controlled trial. Behav Res Ther. 2017;97:14–25.
Burgess M, Gill M, Marks I. Postal self-exposure treatment of recurrent nightmares. Randomised controlled trial. Br J Psychiatry. 1998;172:257–62.
Grandi S, Fabbri S, Panattoni N, Gonnella E, Marks I. Self-exposure treatment of recurrent nightmares: waiting-list-controlled trial and 4-year follow-up. Psychother Psychosom. 2006;75(6):384–8.
Kingsbury SJ. Brief hypnotic treatment of repetitive nightmares. Am J Clin Hypn. 1993;35(3):161–9.
Hauri PJ, Silber MH, Boeve BF. The treatment of parasomnias with hypnosis: a 5- year follow-up study. J Clin Sleep Med. 2007;3(4):369–73.
Silver SM, Brooks A, Obenchain J. Treatment of Vietnam War veterans with PTSD: a comparison of eye movement desensitization and reprocessing, biofeedback, and relaxation training. J Trauma Stress. 1995;8(2):337–42.
Ulmer CS, Edinger JD, Calhoun PS. A multi-component cognitive-behavioral intervention for sleep disturbance in veterans with PTSD: a pilot study. J Clin Sleep Med. 2011;7(1):57–68.
Margolies SO, Rybarczyk B, Vrana SR, Leszczyszyn DJ, Lynch J. Efficacy of a cognitive-behavioral treatment for insomnia and nightmares in Afghanistan and Iraq veterans with PTSD. J Clin Psychol. 2013;69(10):1026–42.
Bishop TM, Britton PC, Knox KL, Pigeon WR. Cognitive behavioral therapy for insomnia and imagery rehearsal in combat veterans with comorbid posttraumatic stress: a case series. Mil Behav Health. 2016;4(1):58–64.
Hardy L, Jones JG, Gould D. Understanding psychological preparation for sport: Theory and practice of elite performers, vol. xvi. Hoboken: John Wiley & Sons, Inc.; 1996. p. 346.
Krakow B, Kellner R, Pathak D, Lambert L. Imagery rehearsal treatment for chronic nightmares. Behav Res Ther. 1995;33(7):837–43.
Krakow B, Zadra A. Imagery rehearsal therapy: principles and practice. Sleep Med Clin. 2010;5(2):289–98.
Augedal AW, Hansen KS, Kronhaug CR, Harvey AG, Pallesen S. Randomized controlled trials of psychological and pharmacological treatments for nightmares: a meta-analysis. Sleep Med Rev. 2013;17(2):143–52.
Casement MD, Swanson LM. A meta-analysis of imagery rehearsal for post-trauma nightmares: effects on nightmare frequency, sleep quality, and posttraumatic stress. Clin Psychol Rev. 2012;32(6):566–74.
Zhang Y, Ren R, Vitiello MV, Yang L, Zhang H, Shi Y, et al. Efficacy and acceptability of psychotherapeutic and pharmacological interventions for trauma-related nightmares: a systematic review and network meta-analysis. Neurosci Biobehav Rev. 2022;139:104717. This meta-analysis shows that IRT and Prazosin are the most effective interventions for trauma-associated nightmares
Davis JL, Wright DC. Exposure, relaxation, and rescripting treatment for trauma-related nighmares. J Trauma Dissociation. 2006;7(1):5–18.
Saunders DT, Roe CA, Smith G, Clegg H. Lucid dreaming incidence: a quality effects meta-analysis of 50 years of research. Conscious Cogn. 2016;43:197–215.
Zadra AL, Donderi DC, Pihl RO. Efficacy of lucid dream induction for lucid and non-lucid dreamers. Dreaming. 1992;2(2):85–97.
Tholey P. Techniques for inducing and manipulating lucid dreams. Percept Mot Skills. 1983;57(1):79–90.
Stumbrys T, Erlacher D, Schädlich M, Schredl M. Induction of lucid dreams: a systematic review of evidence. Conscious Cogn. 2012;21(3):1456–75.
Mallett R, Sowin L, Raider R, Konkoly KR, Paller KA. Benefits and concerns of seeking and experiencing lucid dreams: benefits are tied to successful induction and dream control. Sleep Adv. 2022;3(1):zpac027.
Morin CM, Espie CA, editors. Cognitive therapy. In: Insomnia: a clinical guide to assessment and treatment. Boston: Springer US; 2004. p. 77–99. https://doi.org/10.1007/0-306-47896-X_6
Miller WR, DiPilato M. Treatment of nightmares via relaxation and desensitization: a controlled evaluation. J Consult Clin Psychol. 1983;51(6):870–7.
Boehnlein JK, Kinzie JD. Pharmacologic reduction of CNS noradrenergic activity in PTSD: the case for clonidine and prazosin. J Psychiatr Pract. 2007;13(2):72–8.
Ahmadpanah M, Sabzeiee P, Hosseini SM, Torabian S, Haghighi M, Jahangard L, et al. Comparing the effect of prazosin and hydroxyzine on sleep quality in patients suffering from posttraumatic stress disorder. Neuropsychobiology. 2014;69(4):235–42.
Germain A, Richardson R, Moul DE, Mammen O, Haas G, Forman SD, et al. Placebo-controlled comparison of prazosin and cognitive-behavioral treatments for sleep disturbances in US Military Veterans. J Psychosom Res. 2012;72(2):89–96.
Petrakis IL, Desai N, Gueorguieva R, Arias A, O’Brien E, Jane JS, et al. Prazosin for veterans with posttraumatic stress disorder and comorbid alcohol dependence: a clinical trial. Alcohol Clin Exp Res. 2016;40(1):178–86.
Raskind MA, Peskind ER, Chow B, Harris C, Davis-Karim A, Holmes HA, et al. Trial of Prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. 2018;378(6):507–17.
Raskind MA, Peskind ER, Hoff DJ, Hart KL, Holmes HA, Warren D, et al. A parallel group placebo controlled study of prazosin for trauma nightmares and sleep disturbance in combat veterans with post-traumatic stress disorder. Biol Psychiatry. 2007;61(8):928–34.
Raskind MA, Peterson K, Williams T, Hoff DJ, Hart K, Holmes H, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170(9):1003–10.
Simpson TL, Malte CA, Dietel B, Tell D, Pocock I, Lyons R, et al. A pilot trial of prazosin, an alpha-1 adrenergic antagonist, for comorbid alcohol dependence and posttraumatic stress disorder. Alcohol Clin Exp Res. 2015;39(5):808–17.
Taylor FB, Martin P, Thompson C, Williams J, Mellman TA, Gross C, et al. Prazosin effects on objective sleep measures and clinical symptoms in civilian trauma posttraumatic stress disorder: a placebo-controlled study. Biol Psychiatry. 2008;63(6):629–32.
Reist C, Streja E, Tang CC, Shapiro B, Mintz J, Hollifield M. Prazosin for treatment of post-traumatic stress disorder: a systematic review and meta-analysis. CNS Spectr. 2021;26(4):338–44.
Skeie-Larsen M, Stave R, Grønli J, Bjorvatn B, Wilhelmsen-Langeland A, Zandi A, et al. The effects of pharmacological treatment of nightmares: a systematic literature review and meta-analysis of placebo-controlled, randomized clinical trials. Int J Environ Res Public Health. 2022;20(1):777.
Singh B, Hughes AJ, Mehta G, Erwin PJ, Parsaik AK. Efficacy of Prazosin in posttraumatic stress disorder: a systematic review and meta-analysis. Prim Care Companion CNS Disord. 2016;18(4). https://doi.org/10.4088/PCC.16r01943, https://www.psychiatrist.com/pcc/efficacy-of-prazosin-in-ptsd/.
George KC, Kebejian L, Ruth LJ, Miller CWT, Himelhoch S. Meta-analysis of the efficacy and safety of prazosin versus placebo for the treatment of nightmares and sleep disturbances in adults with posttraumatic stress disorder. J Trauma Dissociation. 2016;17(4):494–510.
Zhang Y, Ren R, Sanford LD, Yang L, Ni Y, Zhou J, et al. The effects of prazosin on sleep disturbances in post-traumatic stress disorder: a systematic review and meta-analysis. Sleep Med. 2020;67:225–31. This meta-analysis describes the effects of Prazosin on nightmares and other PTSD symptoms compared to placebo
Zhang Y, Ren R, Sanford LD, Tang X. Commentary on Yücel DE et al. Downgrading recommendation level of prazosin for treating trauma-related nightmares: should decision be based on a single study? Sleep Med Rev. 2020 Jun;1(51):101285.
Yücel DE, van Emmerik AAP, Souama C, Lancee J. Comparative efficacy of imagery rehearsal therapy and prazosin in the treatment of trauma-related nightmares in adults: a meta-analysis of randomized controlled trials. Sleep Med Rev. 2020;50:101248. This meta-analysis shows comparable effectiveness between Prazosin and IRT for trauma-related nightmares
Cates ME, Bishop MH, Davis LL, Lowe JS, Woolley TW. Clonazepam for treatment of sleep disturbances associated with combat-related posttraumatic stress disorder. Ann Pharmacother. 2004;38(9):1395–9.
Stein DJ, Pedersen R, Rothbaum BO, Baldwin DS, Ahmed S, Musgnung J, et al. Onset of activity and time to response on individual CAPS-SX17 items in patients treated for post-traumatic stress disorder with venlafaxine ER: a pooled analysis. Int J Neuropsychopharmacol. 2009;12(1):23–31.
Thompson DF, Pierce DR. Drug-induced nightmares. Ann Pharmacother. 1999;33(1):93–8.
Pagel JF, Helfter P. Drug induced nightmares--an etiology based review. Hum Psychopharmacol. 2003;18(1):59–67.
Shapiro F, Maxfield L. Eye Movement Desensitization and Reprocessing (EMDR): information processing in the treatment of trauma. J Clin Psychol. 2002;58(8):933–46.
Seda G, Sanchez-Ortuno MM, Welsh CH, Halbower AC, Edinger JD. Comparative meta-analysis of prazosin and imagery rehearsal therapy for nightmare frequency, sleep quality, and posttraumatic stress. J Clin Sleep Med. 2015;11(1):11–22.
Geldenhuys C, van den Heuvel LL, Steyn P, Seedat S. Pharmacological management of nightmares associated with posttraumatic stress disorder. CNS Drugs. 2022;36(7):721–37.
Phelps AJ, Kanaan RAA, Worsnop C, Redston S, Ralph N, Forbes D. An ambulatory polysomnography study of the post-traumatic nightmares of post-traumatic stress disorder. Sleep. 2018;41(1):zsx188. https://doi.org/10.1093/sleep/zsx188.
Mysliwiec V, Brock MS, Creamer JL, O’Reilly BM, Germain A, Roth BJ. Trauma associated sleep disorder: a parasomnia induced by trauma. Sleep Med Rev. 2018;37:94–104.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
Studies with human subjects performed by the authors and included in this review were approved by research ethics committees. This article does not contain any studies with animal subjects.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Romier, A., Clerici, E., Stern, E. et al. Therapeutic Management of Nightmares: Practice Guide for Imagery Rehearsal Therapy (IRT). Curr Sleep Medicine Rep (2024). https://doi.org/10.1007/s40675-024-00287-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s40675-024-00287-8