Abstract
Purpose of Review
Treatment of obstructive sleep apnea (OSA) has historically been centered on outpatients given sleep testing is performed on an outpatient basis. Much of this practice originates from insurers only covering sleep testing on an outpatient basis. Over the last decade, there have been innovations made in the portability of sleep monitors which have allowed sleep testing on inpatients to be facilitated. There is also emerging data that inpatient sleep testing may reduce readmissions and healthcare costs in certain cardiovascular conditions. Accordingly, this review aims to provide comprehensive coverage of recent advances in the practice of inpatient sleep medicine and its effect on reducing the burden of cardiovascular disease.
Recent Findings
Chief cardiovascular diseases that intersect with OSA in inpatients are stroke, atrial fibrillation, and heart failure. There is data from the National Inpatient Sample comparing arrhythmia burdens in patients with OSA and HFpEF showing that OSA patients have higher mortality rates, hospital durations, and medical costs. Also, OSA is associated with higher burdens of arrhythmia. It is currently unknown whether treatment of inpatients with PAP therapy lowers the occurrence of arrhythmias. Recent data suggests that costs for heart failure patients with OSA that are readmitted are higher than those for heart failure patients without OSA. A recent analysis of patients with HFpEF (heart failure with preserved ejection fraction) and OSA showed that the PAP adherent patients had fewer healthcare related costs, lower readmission rates, and fewer emergency room visits than those that were non-adherent. In broader terms, rapid initiation of PAP therapy in a large administration database query of 23 million Medicare patients appears to reduce annual healthcare costs and reduce readmissions although further study is required.
Summary
OSA is globally underdiagnosed, with an estimated 1 billion individuals affected. OSA’s pathogenesis involves a combination of risk factors, such as obesity, age, and increased neck circumference that contribute to fragmented sleep patterns and, in turn, numerous cardiovascular comorbidities, such as stroke, atrial fibrillation, and coronary artery disease. Recently, inpatient sleep medicine programs have emerged as a promising avenue for improving diagnosis, patient safety, and potentially reducing readmissions. Integrating inpatient sleep medicine into healthcare systems to address the significant health and economic burden associated with undiagnosed OSA. Improved coverage of inpatient sleep testing and services will be a key driver of addressing inpatient gaps in sleep medicine care. The current research findings provide a bedrock from which further investigations may proceed in a prospective and randomized, controlled fashion to further clarify the effects of treatment of OSA on cardiovascular outcomes of inpatients.

Similar content being viewed by others
Change history
23 February 2024
A Correction to this paper has been published: https://doi.org/10.1007/s40675-024-00286-9
References
Lv R, Liu X, Zhang Y, Dong N, Wang X, He Y, et al. Pathophysiological mechanisms and therapeutic approaches in obstructive sleep apnea syndrome. Signal Transduct Target Ther. 2023;8(1):218. https://doi.org/10.1038/s41392-023-01496-3.
Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81. https://doi.org/10.1016/j.smrv.2016.07.002.
Suen C, Wong J, Ryan CM, Goh S, Got T, Chaudhry R, et al. Prevalence of undiagnosed obstructive sleep apnea among patients hospitalized for cardiovascular disease and associated in-hospital outcomes: a scoping review. J Clin Med. 2020;9(4):989. https://doi.org/10.3390/jcm9040989.
Kapur V, Strohl KP, Redline S, Iber C, O’Connor G, Nieto J. Underdiagnosis of sleep apnea syndrome in U.S. communities. Sleep Breath. 2002;6(2):49–54. https://doi.org/10.1007/s11325-002-0049-5.
Sofer T. Overcoming the underdiagnosis of obstructive sleep apnea to empower genetic association analyses. Sleep. 2023;46(3):zsac312. https://doi.org/10.1093/sleep/zsac312.
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019;7(8):687–98. https://doi.org/10.1016/s2213-2600(19)30198-5.
Young T, Skatrud J, Peppard PE. Risk factors for obstructive sleep apnea in adults. JAMA. 2004;291(16):2013–6. https://doi.org/10.1001/jama.291.16.2013.
Arnaud C, Bochaton T, Pépin J-L, Belaidi E. Obstructive sleep apnoea and cardiovascular consequences: pathophysiological mechanisms. Arch Cardiovasc Dis. 2020;113(5):350–8. https://doi.org/10.1016/j.acvd.2020.01.003.
Lévy P, Kohler M, McNicholas WT, Barbé F, McEvoy RD, Somers VK, et al. Obstructive sleep apnoea syndrome. Nat Rev Dis Primers. 2015;1:15015. https://doi.org/10.1038/nrdp.2015.15.
Lavie L. Oxidative stress in obstructive sleep apnea and intermittent hypoxia—revisited—the bad ugly and good: implications to the heart and brain. Sleep Med Rev. 2015;20:27–45. https://doi.org/10.1016/j.smrv.2014.07.003.
Drager LF, McEvoy RD, Barbe F, Lorenzi-Filho G, Redline S. Sleep apnea and cardiovascular disease: lessons from recent trials and need for team science. Circulation. 2017;136(19):1840–50. https://doi.org/10.1161/circulationaha.117.029400.
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(03):479–504. https://doi.org/10.5664/jcsm.6506.
Rundo JV. Obstructive sleep apnea basics. Cleve Clin J Med. 2019;86(9 Suppl 1):2–9. https://doi.org/10.3949/ccjm.86.s1.02.
Peker Y, Akdeniz B, Altay S, Balcan B, Başaran Ö, Baysal E, et al. Obstructive sleep apnea and cardiovascular disease: where do we stand? Anatol J Cardiol. 2023;27(7):375–89. https://doi.org/10.14744/AnatolJCardiol.2023.3307.
Collop NA, Anderson WM, Boehlecke B, Claman D, Goldberg R, Gottlieb DJ, et al. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients Portable. Monitoring Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2007;3(7):737–47.
Morsy NE, Farrag NS, Zaki NFW, Badawy AY, Abdelhafez SA, El-Gilany A-H, et al. Obstructive sleep apnea: personal, societal, public health, and legal implications. Rev Environ Health. 2019;34(2):153–69. https://doi.org/10.1515/reveh-2018-0068.
Rico CDP, Stansbury R. Inpatient sleep medicine: an invaluable service for hospital medicine [Internet]. 2023. Available from: https://www.mdedge.com/chestphysician/article/259239/society-news/inpatient-sleep-medicine-invaluable-service-hospital.
Sharma S, Mather PJ, Efird JT, Kahn D, Shiue KY, Cheema M, et al. Obstructive sleep apnea in obese hospitalized patients: a single center experience. J Clin Sleep Med. 2015;11(7):717–23. https://doi.org/10.5664/jcsm.4842.
Sharma S, Mukhtar U, Kelly C, Mather P, Quan SF. Recognition and treatment of sleep-disordered breathing in obese hospitalized patients may improve survival. The HoSMed Database Am J Med. 2017;130(10):1184–91. https://doi.org/10.1016/j.amjmed.2017.03.055.
Rives-Sanchez M, Quintos A, Prillaman B, Willes L, Swaminathan N, Niroula A, et al. Sleep disordered breathing in hospitalized African-Americans. J Natl Med Assoc. 2020;112(3):262–7. https://doi.org/10.1016/j.jnma.2020.03.011.
Sharma S, Stansbury R. Sleep-disordered breathing in hospitalized patients: a game changer? Chest. 2022;161(4):1083–91. https://doi.org/10.1016/j.chest.2021.10.016.
Tan A, Yin JDC, Tan LWL, van Dam RM, Cheung YY, Lee C-H. Using the Berlin Questionnaire to predict obstructive sleep apnea in the general population. J Clin Sleep Med. 2017;13(03):427–32.
Pivetta B, Chen L, Nagappa M, Saripella A, Waseem R, Englesakis M, et al. Use and performance of the STOP-Bang Questionnaire for obstructive sleep apnea screening across geographic regions: a systematic review and meta-analysis. JAMA Network Open. 2021;4(3):e211009-e. https://doi.org/10.1001/jamanetworkopen.2021.1009.
Yang H, Watach A, Varrasse M, King TS, Sawyer AM. Clinical trial enrollment enrichment in resource-constrained research environments: multivariable apnea prediction (MAP) index in SCIP-PA trial. J Clin Sleep Med. 2018;14(2):173–81. https://doi.org/10.5664/jcsm.6926.
Jin J. Screening for obstructive sleep apnea. JAMA. 2022;328(19):1988. https://doi.org/10.1001/jama.2022.20142.
Onder R, Vermunicht P, Delesie M, Willemen M, Verbraecken J, et al. Usability and accuracy of polygraphy devices as a screening tool for obstructive sleep apnea in an atrial fibrillation population. EP Europace. 2023;25(Supplement_1):euad122.219. https://doi.org/10.1093/europace/euad122.219.
Barone DA, Krieger AC. Stroke and obstructive sleep apnea: a review. Curr Atheroscler Rep. 2013;15(7):334. https://doi.org/10.1007/s11883-013-0334-8.
Yaranov DM, Smyrlis A, Usatii N, Butler A, Petrini JR, Mendez J, et al. Effect of obstructive sleep apnea on frequency of stroke in patients with atrial fibrillation. Am J Cardiol. 2015;115(4):461–5. https://doi.org/10.1016/j.amjcard.2014.11.027.
Lipford MC, Flemming KD, Calvin AD, Mandrekar J, Brown RD Jr, Somers VK, et al. Associations between cardioembolic stroke and obstructive sleep apnea. Sleep. 2015;38(11):1699–705. https://doi.org/10.5665/sleep.5146.
Arzt M, Young T, Finn L, Skatrud JB, Bradley TD. Association of sleep-disordered breathing and the occurrence of stroke. Am J Respir Crit Care Med. 2005;172(11):1447–51. https://doi.org/10.1164/rccm.200505-702OC.
Htoo AK, Greenberg H, Tongia S, Chen G, Henderson T, Wilson D, et al. Activation of nuclear factor kappaB in obstructive sleep apnea: a pathway leading to systemic inflammation. Sleep Breath. 2006;10(1):43–50. https://doi.org/10.1007/s11325-005-0046-6.
Durgan DJ, Bryan RM Jr. Cerebrovascular consequences of obstructive sleep apnea. J Am Heart Assoc. 2012;1(4):e000091. https://doi.org/10.1161/jaha.111.000091.
Dong R, Dong Z, Liu H, Shi F, Du J. Prevalence, risk factors, outcomes, and treatment of obstructive sleep apnea in patients with cerebrovascular disease: a systematic review. J Stroke Cerebrovasc Dis. 2018;27(6):1471–80. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.12.048.
Davis AP, Billings ME, Longstreth WT Jr, Khot SP. Early diagnosis and treatment of obstructive sleep apnea after stroke: are we neglecting a modifiable stroke risk factor? Neurol Clin Pract. 2013;3(3):192–201. https://doi.org/10.1212/CPJ.0b013e318296f274.
Dyken ME, Im KB. Obstructive sleep apnea and stroke. Chest. 2009;136(6):1668–77. https://doi.org/10.1378/chest.08-1512.
Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365(9464):1046–53. https://doi.org/10.1016/s0140-6736(05)71141-7.
Parra O, Sánchez-Armengol A, Bonnin M, Arboix A, Campos-Rodríguez F, Pérez-Ronchel J, et al. Early treatment of obstructive apnoea and stroke outcome: a randomised controlled trial. Eur Respir J. 2011;37(5):1128–36. https://doi.org/10.1183/09031936.00034410.
Sandberg O, Franklin KA, Bucht G, Eriksson S, Gustafson Y. Nasal continuous positive airway pressure in stroke patients with sleep apnoea: a randomized treatment study. Eur Respir J. 2001;18(4):630–4. https://doi.org/10.1183/09031936.01.00070301.
Bravata DM, Concato J, Fried T, Ranjbar N, Sadarangani T, McClain V, et al. Continuous positive airway pressure: evaluation of a novel therapy for patients with acute ischemic stroke. Sleep. 2011;34(9):1271–7. https://doi.org/10.5665/sleep.1254.
Ryan CM, Bayley M, Green R, Murray BJ, Bradley TD. Influence of continuous positive airway pressure on outcomes of rehabilitation in stroke patients with obstructive sleep apnea. Stroke. 2011;42(4):1062–7. https://doi.org/10.1161/strokeaha.110.597468.
Brown DL, Durkalski V, Durmer JS, Broderick JP, Zahuranec DB, Levine DA, et al. Sleep for Stroke Management and Recovery Trial (Sleep SMART): rationale and methods. Int J Stroke. 2020;15(8):923–9. https://doi.org/10.1177/1747493020903979.
Moula AI, Parrini I, Tetta C, Lucà F, Parise G, Rao CM, et al. Obstructive sleep apnea and atrial fibrillation. J Clin Med. 2022;11(5):1242. https://doi.org/10.3390/jcm11051242.
Kendzerska T, Gershon AS, Atzema C, Dorian P, Mangat I, Hawker G, et al. Sleep apnea increases the risk of new hospitalized atrial fibrillation: a historical cohort study. Chest. 2018;154(6):1330–9. https://doi.org/10.1016/j.chest.2018.08.1075.
Monahan K, Brewster J, Wang L, Parvez B, Goyal S, Roden DM, et al. Relation of the severity of obstructive sleep apnea in response to anti-arrhythmic drugs in patients with atrial fibrillation or atrial flutter. Am J Cardiol. 2012;110(3):369–72. https://doi.org/10.1016/j.amjcard.2012.03.037.
Kanagala R, Murali NS, Friedman PA, Ammash NM, Gersh BJ, Ballman KV, et al. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation. 2003;107(20):2589–94. https://doi.org/10.1161/01.Cir.0000068337.25994.21.
Fein AS, Shvilkin A, Shah D, Haffajee CI, Das S, Kumar K, et al. Treatment of obstructive sleep apnea reduces the risk of atrial fibrillation recurrence after catheter ablation. J Am Coll Cardiol. 2013;62(4):300–5. https://doi.org/10.1016/j.jacc.2013.03.052.
Shukla A, Aizer A, Holmes D, Fowler S, Park DS, Bernstein S, et al. Effect of obstructive sleep apnea treatment on atrial fibrillation recurrence: a meta-analysis. JACC: Clin Electrophysiol. 2015;1(1):41–51. https://doi.org/10.1016/j.jacep.2015.02.014.
Gill J, Wu C. In-hospital outcomes and arrhythmia burden in patients with obstructive sleep apnea and heart failure with preserved ejection fraction. J Innov Card Rhythm Manag. 2022;13(6):5033–40. https://doi.org/10.19102/icrm.2022.130602.
Brgdar A, Yi J, Awan A, Taha M, Ogunti R, Gharbin J, et al. Impact of obstructive sleep apnea on in-hospital outcomes in patients with atrial fibrillation: a retrospective analysis of the national inpatient sample. Cureus. 2021;13(12):e20770. https://doi.org/10.7759/cureus.20770.
Khattak HK, Hayat F, Pamboukian SV, Hahn HS, Schwartz BP, Stein PK. Obstructive sleep apnea in heart failure: review of prevalence, treatment with continuous positive airway pressure, and prognosis. Tex Heart Inst J. 2018;45(3):151–61. https://doi.org/10.14503/thij-15-5678.
Holt A, Bjerre J, Zareini B, Koch H, Tønnesen P, Gislason GH, et al. Sleep apnea, the risk of developing heart failure, and potential benefits of continuous positive airway pressure (CPAP) therapy. J Am Heart Assoc. 2018;7(13):e008684. https://doi.org/10.1161/jaha.118.008684.
Khayat R, Abraham W, Patt B, Brinkman V, Wannemacher J, Porter K, et al. Central sleep apnea is a predictor of cardiac readmission in hospitalized patients with systolic heart failure. J Card Fail. 2012;18(7):534–40. https://doi.org/10.1016/j.cardfail.2012.05.003.
Khayat R, Jarjoura D, Porter K, Sow A, Wannemacher J, Dohar R, et al. Sleep disordered breathing and post-discharge mortality in patients with acute heart failure. Eur Heart J. 2015;36(23):1463–9. https://doi.org/10.1093/eurheartj/ehu522.
Khayat RN, Porter K, Germany RE, McKane SW, Healy W, Randerath W. Clinical and financial impact of sleep disordered breathing on heart failure admissions. Sleep and Breathing. 2023;27(5):1917–24. https://doi.org/10.1007/s11325-023-02813-4.
Javaheri S, Caref EB, Chen E, Tong KB, Abraham WT. Sleep apnea testing and outcomes in a large cohort of Medicare beneficiaries with newly diagnosed heart failure. Am J Respir Crit Care Med. 2011;183(4):539–46. https://doi.org/10.1164/rccm.201003-0406OC.
Egea CJ, Aizpuru F, Pinto JA, Ayuela JM, Ballester E, Zamarrón C, et al. Cardiac function after CPAP therapy in patients with chronic heart failure and sleep apnea: a multicenter study. Sleep Med. 2008;9(6):660–6. https://doi.org/10.1016/j.sleep.2007.06.018.
Aurora RN, Patil SP, Punjabi NM. Portable sleep monitoring for diagnosing sleep apnea in hospitalized patients with heart failure. Chest. 2018;154(1):91–8. https://doi.org/10.1016/j.chest.2018.04.008.
Khayat RN, Javaheri S, Porter K, Sow A, Holt R, Randerath W, et al. In-hospital management of sleep apnea during heart failure hospitalization: a randomized controlled trial. J Card Fail. 2020;26(8):705–12. https://doi.org/10.1016/j.cardfail.2020.06.007.
Mokhlesi B. Obesity hypoventilation syndrome: a state-of-the-art review. Respir Care. 2010;55(10):1347–65.
Afshar M, Brozek JL, Soghier I, Kakazu MT, Wilson KC, Masa JF, et al. The role of positive airway pressure therapy in adults with obesity hypoventilation syndrome A systematic review and meta-analysis. Ann Am Thorac Soc. 2020;17(3):344–60. https://doi.org/10.1513/AnnalsATS.201907-528OC.
Soghier I, Brożek JL, Afshar M, Tamae Kakazu M, Wilson KC, Masa JF, et al. Noninvasive ventilation versus CPAP as initial treatment of obesity hypoventilation syndrome. Ann Am Thorac Soc. 2019;16(10):1295–303. https://doi.org/10.1513/AnnalsATS.201905-380OC.
Agossou M, Awanou B, Inamo J, Rejaudry-Lacavalerie M, Arnal JM, Dramé M. Impact of previous continuous positive airway pressure use on noninvasive ventilation adherence and quality in obesity hypoventilation syndrome: a pragmatic single-center cross-sectional study in Martinique. Biomedicines. 2023;11(10):2753. https://doi.org/10.3390/biomedicines11102753.
Mokhlesi B, Masa JF, Afshar M, Almadana Pacheco V, Berlowitz DJ, Borel JC, et al. The effect of hospital discharge with empiric noninvasive ventilation on mortality in hospitalized patients with obesity hypoventilation syndrome An individual patient data meta-analysis. Ann Am Thorac Soc. 2020;17(5):627–37. https://doi.org/10.1513/AnnalsATS.201912-887OC.
Cistulli PA, Malhotra A, Cole KV, Malik AS, Pépin JL, Sert Kuniyoshi FH, et al. Positive airway pressure therapy adherence and health care resource use in patients with obstructive sleep apnea and heart failure with preserved ejection fraction. J Am Heart Assoc. 2023;12(14):e028733. https://doi.org/10.1161/jaha.122.028733.
Healy WJ, Khayat R, Kwon Y. Breathe better and preserve heart. J Am Heart Assoc. 2023;12(14):e030806. https://doi.org/10.1161/jaha.123.030806.
Bock JM, Needham KA, Gregory DA, Ekono MM, Wickwire EM, Somers VK, et al. Continuous positive airway pressure adherence and treatment cost in patients with obstructive sleep apnea and cardiovascular disease. Mayo Clin Proc Innov Qual Outcomes. 2022;6(2):166–75. https://doi.org/10.1016/j.mayocpiqo.2022.01.002.
Bailey MD, Wickwire EM, Somers VK, Albrecht JS. Adherence to continuous positive airway pressure reduces the risk of 30-day hospital readmission among older adults with comorbid obstructive sleep apnea and cardiovascular disease. J Clin Sleep Med. 2022;18(12):2739–44. https://doi.org/10.5664/jcsm.10196.
Brooks R, Trimble M. The future of sleep technology: report from an American Association of Sleep Technologists summit meeting. J Clin Sleep Med. 2014;10(5):589–93. https://doi.org/10.5664/jcsm.3720.
Supriya KJ, Gulnur C, Xinyu T, Kristi KP, Rithea J, Charles B, et al. Role of a respiratory therapist in improving adherence to positive airway pressure treatment in a pediatric sleep apnea clinic. Respir Care. 2013;58(12):2038. https://doi.org/10.4187/respcare.02312.
Colvin LJ, Cartwright A, Freedman N, Rogers AE, Vana KD. Nurse practitioners and physician assistants are qualified to perform home sleep apnea test clinical evaluations. J Clin Sleep Med. 2018;14(2):293. https://doi.org/10.5664/jcsm.6958.
Jeznach-Steinhagen A, Okręglicka K, Nitsch-Osuch A, Czerwonogrodzka-Senczyna A, Barnaś M. Nutritional status and dietary patterns in adults with severe obstructive sleep apnea. Adv Exp Med Biol. 2020;1279:71–9. https://doi.org/10.1007/5584_2020_507.
Basheti MM, Gordon C, Bawa Z, Grunstein R, Saini B. Sleep health management in community pharmacy: where are we and where should we be heading? Res Social Adm Pharm. 2021;17(11):1945–56. https://doi.org/10.1016/j.sapharm.2021.02.011.
Haynes PL. The role of behavioral sleep medicine in the assessment and treatment of sleep disordered breathing. Clin Psychol Rev. 2005;25(5):673–705. https://doi.org/10.1016/j.cpr.2005.04.009.
Colten HR, Altevogt BM, Institute of Medicine (US) Committee on Sleep Medicine and Research (eds). Sleep disorders and sleep deprivation: an unmet public health problem. Washington (DC): National Academies Press (US). 2006.
Pena-Orbea C, Wang L, Srisawart P, Foldvary-Schaefer N, Mehra R. Sex-specific differences in diagnostic approaches of inpatient sleep testing for obstructive sleep apnea. Sleep Med. 2023;102:157–64. https://doi.org/10.1016/j.sleep.2022.12.011.
Author information
Authors and Affiliations
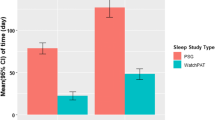
Contributions
A.B., M.A., R.M., N.Z., Y.C., Y.K., W.H. wrote the main manuscript. A.B, W.H., R.M, and M.A prepared the tables. A. B. prepared the figure. All authors revised the manuscript. All authors approved the final version to be published. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bhatt, A., Azam, M.U., Munagala, R. et al. The Emergence of Inpatient Sleep Medicine: Screening for Sleep Disordered Breathing to Reduce the Burden of Cardiovascular Disease. Curr Sleep Medicine Rep 10, 51–61 (2024). https://doi.org/10.1007/s40675-024-00275-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40675-024-00275-y