Abstract
Purpose of Review
Pediatric sleep medicine is a developing field with recent advances in pathophysiology, diagnosis, and/or management of circadian rhythm disorders, obstructive sleep apnea, narcolepsy, and parasomnias. This article aims to provide a review and highlight recent updates in these specific sleep disorders.
Recent Findings
Our understanding of circadian rhythms and melatonin profiling is becoming clearer, which opens up new diagnostic possibilities and treatment refinement. In obstructive sleep apnea, symptoms do not clearly correlate with the apnea-hypopnea index, and other sleep measures need to be studied in order to understand how treatments may provide benefit to patients. There has been the first clinical treatment trial in pediatric narcolepsy and promising drugs are on the horizon. While parasomnia treatment has not advanced much, our understanding of its pathophysiology and associated diagnostic features is growing.
Summary
Advancements across a number of areas of pediatric sleep medicine offers exciting avenues for more accurate and timely diagnoses and evidence-based management to improve patient care.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Maski K, Steinhart E, Holbrook H, Katz ES, Kapur K, Stickgold R. Impaired memory consolidation in children with obstructive sleep disordered breathing. 2017;12(11):17.
Irwin MR, Opp MR. Sleep health: reciprocal regulation of sleep and innate immunity. Neuropsychopharmacol. 2017;42(1):129–55.
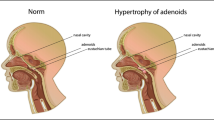
Dehlink E, Tan H-L. Update on paediatric obstructive sleep apnoea. J Thorac Dis. 2016;8(2):12.
Mindell JA, Kuhn B, Lewin DS, Meltzer LJ, Sadeh A. Behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep. 2006;29(10):1263–76.
Williamson AA, Mindell JA, Hiscock H, Quach J. Child sleep behaviors and sleep problems from infancy to school-age. Sleep Med. 2019;63:5–8.
Bartel KA, Gradisar M, Williamson P. Protective and risk factors for adolescent sleep: a meta-analytic review. Sleep Med Rev. 2015;21:72–85.
Taveras EM, Rifas-Shiman SL, Bub KL, Gillman MW, Oken E. Prospective study of insufficient sleep and neurobehavioral functioning among school-age children. Acad Pediatr. 2017;17(6):625–32.
Thorpy MJ, Krieger AC. Delayed diagnosis of narcolepsy: characterization and impact. Sleep Med. 2014;15(5):502–7.
Miano S, Peraita-Adrados R. Nocturnal frontal lobe epilepsy is often misdiagnosed as sleep disorders in children: a case series. Rev Neurol. 2013;56(5):257–67.
American Academy of Sleep Medicine. International classification of sleep disorders. 3rd ed. Darien: American Academy of Sleep Medicine; 2014.
Paine S-J, Fink J, Gander PH, Warman GR. Identifying advanced and delayed sleep phase disorders in the general population: a national survey of New Zealand adults. Chronobiol Int. 2014;31(5):627–36.
Danielsson K, Markström A, Broman J-E, von Knorring L, Jansson-Fröjmark M. Delayed sleep phase disorder in a Swedish cohort of adolescents and young adults: prevalence and associated factors. Chronobiol Int. 2016;33(10):1331–9.
Borbély AA, Daan S, Wirz-Justice A, Deboer T. The two-process model of sleep regulation: a reappraisal. J Sleep Res. 2016;25(2):131–43.
Carskadon MA, Vieira C, Acebo C. Association between puberty and delayed phase preference. Sleep. 1993;16(3):258–62.
Andrade M, Beneditosilva A, Domenice S, Arnhold I, Mennabarreto L. Sleep characteristics of adolescents: a longitudinal study. J Adolesc Health. 1993;14(5):401–6.
Tanner JM. Growth at adolescence. 2nd ed. Springfield: Thomas; 1962.
• Crowley SJ, Wolfson AR, Tarokh L, Carskadon MA. An update on adolescent sleep: new evidence informing the perfect storm model. J Adolesc. 2018;67:55–65 An interesting review of changes in adolescent sleep.
Taylor DJ, Jenni OG, Acebo C, Carskadon MA. Sleep tendency during extended wakefulness: insights into adolescent sleep regulation and behavior. J Sleep Res. 2005;14(3):239–44.
Tarokh L, Carskadon MA, Achermann P. Dissipation of sleep pressure is stable across adolescence. Neuroscience. 2012;216:167–77.
Paruthi S, Brooks LJ, D’Ambrosio C, Hall WA, Kotagal S, Lloyd RM, et al. Consensus statement of the American Academy of Sleep Medicine on the recommended amount of sleep for healthy children: methodology and discussion. JCSM. 2016;12(11):1549–61.
Keyes KM, Maslowsky J, Hamilton A, Schulenberg J. The great sleep recession: changes in sleep duration among US adolescents, 1991-2012. PEDIATRICS. 2015;135(3):460–8.
• Chinoy ED, Duffy JF, Czeisler CA. Unrestricted evening use of light-emitting tablet computers delays self-selected bedtime and disrupts circadian timing and alertness. Physiol Rep. 2018;6(10):e13692 An attempt to quantify the effects of artificial light on alertness, sleep, and melatonin secretion.
van der Lely S, Frey S, Garbazza C, Wirz-Justice A, Jenni OG, Steiner R, et al. Blue blocker glasses as a countermeasure for alerting effects of evening light-emitting diode screen exposure in male teenagers. J Adolesc Health. 2015;56(1):113–9.
Sivertsen B, Pallesen S, Stormark KM, Bøe T, Lundervold AJ, Hysing M. Delayed sleep phase syndrome in adolescents: prevalence and correlates in a large population based study. BMC Public Health. 2013;13(1):1163.
Bartlett DJ, Biggs SN, Armstrong SM. Circadian rhythm disorders among adolescents: assessment and treatment options. Med J Aust. 2013 Oct [cited 2019 Dec 6];199(S8). Available from: https://onlinelibrary.wiley.com/doi/abs/10.5694/mja13.10912
Crowley SJ, Suh C, Molina TA, Fogg LF, Sharkey KM, Carskadon MA. Estimating the dim light melatonin onset of adolescents within a 6-h sampling window: the impact of sampling rate and threshold method. Sleep Med. 2016;20:59–66.
Keijzer H, Smits MG, Duffy JF, Curfs LMG. Why the dim light melatonin onset (DLMO) should be measured before treatment of patients with circadian rhythm sleep disorders. Sleep Med Rev. 2014;18(4):333–9.
Burgess HJ, Revell VL, Molina TA, Eastman CI. Human phase response curves to three days of daily melatonin: 0.5 mg versus 3.0 mg. J Clin Endocrinol Metab. 2010;95(7):3325–31.
Erland LAE, Saxena PK. Melatonin natural health products and supplements: presence of serotonin and significant variability of melatonin content. JCSM. 2017;13(02):275–81.
Wahlstrom KL, Berger AT, Widome R. Relationships between school start time, sleep duration, and adolescent behaviors. Sleep Health. 2017;3(3):216–21.
•• Marx R, Tanner-Smith EE, Davison CM, Ufholz L-A, Freeman J, Shankar R, et al. Later school start times for supporting the education, health, and well-being of high school students. Cochrane Public Health Group, editor. Cochrane Database Syst Rev. 2017 Jul 3 [cited 2019 Dec 12]; Available from: https://doi.org/10.1002/14651858.CD009467.pub2A comprehensive review of the effect of changes in school start times on sleep through 2017.
Honaker SM, Meltzer LJ. Sleep in pediatric primary care: a review of the literature. Sleep Med Rev. 2016;25:31–9.
Pliska BT, Lee J, Chadha NK. Prevalence of malocclusion in children with sleep-disordered breathing. JDSM. 2017;04(02):41–4.
Anderson ICW, Sedaghat AR, McGinley BM, Redett RJ, Boss EF, Ishman SL. Prevalence and severity of obstructive sleep apnea and snoring in infants with Pierre Robin sequence. Cleft Palate-Craniofac J. 2011;48(5):614–8.
Sedky K, Bennett DS, Pumariega A. Prader Willi syndrome and obstructive sleep apnea: co-occurrence in the Pediatric Population. JCSM [Internet]. 2014 Apr 15 [cited 2019 Nov 21]; Available from: http://jcsm.aasm.org/ViewAbstract.aspx?pid=29433
Rosen D, Lombardo A, Skotko B, Davidson EJ. Parental perceptions of sleep disturbances and sleep-disordered breathing in children with Down syndrome. Clin Pediatr (Phila). 2011;50(2):121–5.
Polat. Assessment of sleep-related breathing disorders in patients with Duchenne muscular dystrophy. J Clin Med Res. 2012 [cited 2019 Nov 21]; Available from: http://www.jocmr.org/index.php/JOCMR/article/view/1075
Al-Biltagi MA. Childhood epilepsy and sleep. WJCP. 2014;3(3):45–53.
Andersen IG, Holm J, Homøe P. Obstructive sleep apnea in obese children and adolescents, treatment methods and outcome of treatment – a systematic review. Int J Pediatr Otorhinolaryngol. 2016;87:190–7.
Amin R, Anthony L, Somers V, Fenchel M, McConnell K, Jefferies J, et al. Growth velocity predicts recurrence of sleep-disordered breathing 1 year after adenotonsillectomy. Am J Respir Crit Care Med. 2008;177(6):654–9.
Nieminen P, Tolonen U, Löppönen H. Snoring and obstructive sleep apnea in children: a 6-month follow-up study. Arch Otolaryngol Head Neck Surg. 2000;126(4):481–6.
Goodwin JL, Morgan J. Clinical screening of school children for polysomnography to detect sleep-disordered breathing—the Tucson Children’s Assessment of Sleep Apnea Study (TuCASA). 2005;15.
Melendres CS. Daytime sleepiness and hyperactivity in children with suspected sleep-disordered breathing. PEDIATRICS. 2004;114(3):768–75.
Sedky K, Bennett DS, Carvalho KS. Attention deficit hyperactivity disorder and sleep disordered breathing in pediatric populations: a meta-analysis. Sleep Med Rev. 2014;18(4):349–56.
Choudhary B, Patil R, Bhatt GC, Pakhare AP, Goyal A, P A, et al. Association of sleep disordered breathing with mono-symptomatic nocturnal enuresis: a study among school children of central India. Aggarwal AN, editor. PLoS ONE. 2016;11(5):e0155808.
Spruyt K, Gozal D. Pediatric sleep questionnaires as diagnostic or epidemiological tools: a review of currently available instruments. Sleep Med Rev. 2011;15(1):19–32.
• da Silva Gusmão Cardoso T, Pompéia S, Miranda MC. Cognitive and behavioral effects of obstructive sleep apnea syndrome in children: a systematic literature review. Sleep Med. 2018;46:46–55 An interesting review detailing the cognitive and behavioral associations of obstructive sleep apnea.
Philby MF, Macey PM, Ma RA, Kumar R, Gozal D, Kheirandish-Gozal L. Reduced regional grey matter volumes in pediatric obstructive sleep apnea. Sci Rep. 2017;7(1):44566.
Marcus CL, Moore RH, Rosen CL, Giordani B, Garetz SL, Taylor HG, et al. A randomized trial of adenotonsillectomy for childhood sleep apnea. N Engl J Med. 2013;368(25):2366–76.
Rosen CL, Wang R, Taylor HG, Marcus CL, Katz ES, Paruthi S, et al. Utility of symptoms to predict treatment outcomes in obstructive sleep apnea syndrome 2015;135(3):12.
Section on pediatric pulmonary and subcommittee on obstructive sleep apnea syndrome. Clinical Practice Guideline: Diagnosis and Management of Childhood Obstructive Sleep Apnea Syndrome. Pediatrics. 2002;109:704–12.
Huang Y-S, Guilleminault C, Lee L-A, Lin C-H, Hwang F-M. Treatment outcomes of adenotonsillectomy for children with obstructive sleep apnea: a prospective longitudinal study. Sleep. 2014;37(1):71–6.
Borgström A, Nerfeldt P, Friberg D. Adenotonsillotomy versus adenotonsillectomy in pediatric obstructive sleep apnea: an RCT. Pediatrics. 2017;139(4):e20163314.
Marcus CL. Adherence to and effectiveness of positive airway pressure therapy in children with obstructive sleep apnea. PEDIATRICS. 2006;117(3):e442–51.
Roberts SD, Kapadia H, Greenlee G, Chen ML. Midfacial and dental changes associated with nasal positive airway pressure in children with obstructive sleep apnea and craniofacial conditions. J Clin Sleep Med. 2016;12(04):469–75.
Kheirandish-Gozal L, Bhattacharjee R, Bandla HPR, Gozal D. Antiinflammatory therapy outcomes for mild OSA in children. Chest. 2014;146(1):88–95.
Camacho M, Chang ET, Song SA, Abdullatif J, Zaghi S, Pirelli P, et al. Rapid maxillary expansion for pediatric obstructive sleep apnea: a systematic review and meta-analysis. Laryngoscope. 2017;127(7):1712–9.
Zhu Y, Long H, Jian F, Lin J, Zhu J, Gao M, et al. The effectiveness of oral appliances for obstructive sleep apnea syndrome: a meta-analysis. J Dent. 2015;43(12):1394–402.
Chen J, He S. Drug-induced sleep endoscopy-directed adenotonsillectomy in pediatric obstructive sleep apnea with small tonsils. Parham K, editor. PLoS ONE. 2019;14(2):e0212317.
• Isaiah A, Kiss E, Olomu P, Koral K, Mitchell RB. Characterization of upper airway obstruction using cine MRI in children with residual obstructive sleep apnea after adenotonsillectomy. Sleep Med. 2018;50:79–86 A study which explores the usefulness of cine MRI in OSA treatment.
Manickam PV, Shott SR, Boss EF, Cohen AP, Meinzen-Derr JK, Amin RS, et al. Systematic review of site of obstruction identification and non-CPAP treatment options for children with persistent pediatric obstructive sleep apnea. Laryngoscope. 2016;126(2):491–500.
• Boudewyns A, Saldien V, Van de Heyning P, Verhulst S. Drug-induced sedation endoscopy in surgically naïve infants and children with obstructive sleep apnea: impact on treatment decision and outcome. Sleep Breath. 2018;22(2):503–10 A study which helps to show the potential benefit for DISE prior to an initial surgery.
Caloway CL, Diercks GR, Keamy D, de Guzman V, Soose R, Raol N, et al. Update on hypoglossal nerve stimulation in children with down syndrome and obstructive sleep apnea. Laryngoscope. 2019;lary.28138.
Longstreth WT, Koepsell TD, Ton TG, Hendrickson AF, van Belle G. The epidemiology of narcolepsy. Sleep. 2007;30(1):13–26.
Tió E, Gaig C, Giner-Soriano M, Romero O, Jurado M-J, Sansa G, et al. The prevalence of narcolepsy in Catalunya (Spain). J Sleep Res. 2018;27(5):e12640.
Kryger MH, Walld R, Manfreda J. Diagnoses received by narcolepsy patients in the year prior to diagnosis by a sleep specialist. Sleep. 2002;25(1):36–41.
Maski K, Steinhart E, Williams D, Scammell T, Flygare J, McCleary K, et al. Listening to the patient voice in narcolepsy: diagnostic delay, disease burden, and treatment efficacy. JCSM. 2017;13(03):419–25.
Reading PJ. Update on narcolepsy. J Neurol. 2019;266(7):1809–15.
Mignot E, Lin L, Rogers W, Honda Y, Qiu X, Lin X, et al. Complex HLA-DR and -DQ interactions confer risk of narcolepsy-cataplexy in three ethnic groups. Am J Hum Genet. 2001;68(3):686–99.
Aran A, Lin L, Nevsimalova S, Plazzi G, Hong SC, Weiner K, et al. Elevated anti-streptococcal antibodies in patients with recent narcolepsy onset 2009;32(8):5.
Partinen M, Saarenpää-Heikkilä O, Ilveskoski I, Hublin C, Linna M, Olsén P, et al. Increased incidence and clinical picture of childhood narcolepsy following the 2009 H1N1 pandemic vaccination campaign in Finland. Cowling BJ, editor. PLoS ONE. 2012;7(3):e33723.
Pedersen NW, Holm A, Kristensen NP, Bjerregaard A-M, Bentzen AK, Marquard AM, et al. CD8+ T cells from patients with narcolepsy and healthy controls recognize hypocretin neuron-specific antigens. Nat Commun. 2019;10(1):837.
Latorre D, Kallweit U, Armentani E, Foglierini M, Mele F, Cassotta A, et al. T cells in patients with narcolepsy target self-antigens of hypocretin neurons. Nature. 2018;562(7725):63–8.
Cogswell AC, Maski K, Scammell TE, Tucker D, Orban ZS, Koralnik IJ. Children with narcolepsy type 1 have increased T-cell responses to orexins. Ann Clin Transl Neurol. 2019;6(12):2566–72.
Luo G, Ambati A, Lin L, Bonvalet M, Partinen M, Ji X, et al. Autoimmunity to hypocretin and molecular mimicry to flu in type 1 narcolepsy. Proc Natl Acad Sci U S A. 2018;115(52):E12323–32.
Alakuijala A, Sarkanen T, Partinen M. Hypocretin-1 levels associate with fragmented sleep in patients with narcolepsy type 1. Sleep. 2016;39(5):1047–50.
Overeem S, van Nues SJ, van der Zande WL, Donjacour CE, van Mierlo P, Lammers GJ. The clinical features of cataplexy: a questionnaire study in narcolepsy patients with and without hypocretin-1 deficiency. Sleep Med. 2011;12(1):12–8.
Serra L, Montagna P, Mignot E, Lugaresi E, Plazzi G. Cataplexy features in childhood narcolepsy. Mov Disord. 2008;23(6):858–65.
Ohayon MM, Priest RG, Caulet M, Guilleminault C. Hypnagogic and hypnopompic hallucinations: pathological phenomena? Br J Psychiatry. 1996;169(4):459–67.
Wamsley E, Donjacour CEHM, Scammell TE, Lammers GJ, Stickgold R. Delusional confusion of dreaming and reality in narcolepsy. Sleep. 2014;37(2):419–22.
Antelmi E, Pizza F, Vandi S, Neccia G, Ferri R, Bruni O, et al. The spectrum of REM sleep-related episodes in children with type 1 narcolepsy. Brain. 2017;140(6):1669–79.
Plazzi G, Serra L, Ferri R. Nocturnal aspects of narcolepsy with cataplexy. Sleep Med Rev. 2008;12(2):109–28.
Drake C, Nickel C, Burduvali E, Roth T, Jefferson C, Badia P. The Pediatric Daytime Sleepiness Scale (PDSS): sleep habits and school outcomes in middle-school children. Sleep. 2003 Jun 1 [cited 2019 Nov 10]; Available from: https://academic.oup.com/sleep/article/26/4/455/2707859/The-Pediatric-Daytime-Sleepiness-Scale-PDSS-Sleep
Spilsbury JC, Drotar D, Rosen CL, Redline S. The Cleveland Adolescent Sleepiness Questionnaire: a new measure to assess excessive daytime sleepiness in adolescents 2007;3(6):10.
•• Pizza F, Barateau L, Jaussent I, Vandi S, Antelmi E, Mignot E, et al. Validation of multiple sleep latency test for the diagnosis of pediatric narcolepsy type 1. Neurology. 2019;93(11):e1034–44 A validation study for PSG/MSLT in the pediatric population.
• Lopez R, Doukkali A, Barateau L, Evangelista E, Chenini S, Jaussent I, et al. Test–retest reliability of the multiple sleep latency test in central disorders of hypersomnolence. Sleep. 2017 Dec 1 [cited 2020 Jan 10];40(12). Available from: http://academic.oup.com/sleep/article/doi/10.1093/sleep/zsx164/4584523An article following the stability of diagnosis of hypersomnia disorders on repeated testing.
Ruoff C, Pizza F, Trotti LM, Sonka K, Vandi S, Cheung J, et al. The MSLT is repeatable in narcolepsy type 1 but not narcolepsy type 2: a retrospective patient study. JCSM. 2018;14(01):65–74.
Jin L, Shi L, Zhang Y, Chen B-B, Wang X-L, Liu Y-H. Antidepressants for the treatment of narcolepsy: a prospective study of 148 patients in northern China. J Clin Neurosci. 2019;63:27–31.
Littner MR, Kushida C, Wise M, G. Davila D, Morgenthaler T, Lee-Chiong T, et al. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep. 2005;28(1):113–121.
Lecendreux M, Lavault S, Lopez R, Inocente CO, Konofal E, Cortese S, et al. Attention-deficit/hyperactivity disorder (ADHD) symptoms in pediatric narcolepsy: a cross-sectional study. Sleep. 2015;38(8):1285–95.
Poli F, Pizza F, Mignot E, Ferri R, Pagotto U, Taheri S, et al. High prevalence of precocious puberty and obesity in childhood narcolepsy with cataplexy. Sleep. 2013;36(2):175–81.
Cohen A, Mandrekar J, St. Louis EK, Silber MH, Kotagal S. Comorbidities in a community sample of narcolepsy. Sleep Med 2018;43:14–18.
Moran LV, Ongur D, Hsu J, Castro VM, Perlis RH, Schneeweiss S. Psychosis with methylphenidate or amphetamine in patients with ADHD. N Engl J Med. 2019;380(12):1128–38.
Lecendreux M, Bruni O, Franco P, Gringras P, Konofal E, Nevsimalova S, et al. Clinical experience suggests that modafinil is an effective and safe treatment for paediatric narcolepsy. J Sleep Res. 2012;21(4):481–3.
•• Plazzi G, Ruoff C, Lecendreux M, Dauvilliers Y, Rosen CL, Black J, et al. Treatment of paediatric narcolepsy with sodium oxybate: a double-blind, placebo-controlled, randomised-withdrawal multicentre study and open-label investigation. Lancet Child Adolesc Health. 2018;2(7):483–94 A RCT of sodium oxybate in the pediatric population.
Szakacs Z, Dauvilliers Y, Mikhaylov V, Poverennova I, Krylov S, Jankovic S, et al. Safety and efficacy of pitolisant on cataplexy in patients with narcolepsy: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2017;16(3):200–7.
Thorpy MJ, Shapiro C, Mayer G, Corser BC, Emsellem H, Plazzi G, et al. A randomized study of solriamfetol for excessive sleepiness in narcolepsy. Ann Neurol. 2019;85(3):359–70.
Maski KM, Owens JM. Pediatric sleep disorders. [review]. CONTINUUM: Lifelong Learning in Neurology. 2018;24(1):210–27.
Frank NC, Spirito A, Stark L, Owens-Stively J. The use of scheduled awakenings to eliminate childhood sleepwalking. J Pediatr Psychol. 1997;22(3):345–53.
Kotagal S. Rapid eye movement sleep behavior disorder during childhood. Sleep Med Clin. 2015;10(2):163–7.
Moghadam KK, Pizza F, Primavera A, Ferri R, Plazzi G. Sodium oxybate for idiopathic REM sleep behavior disorder: a report on two patients. Sleep Med. 2017;32:16–21.
Raskind MA, Peskind ER, Chow B, Harris C, Davis-Karim A, Holmes HA, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. 2018;378(6):507–17.
Stallman HM, Kohler M. Prevalence of sleepwalking: a systematic review and meta-analysis. Arez AP, editor. PLoS ONE. 2016;11(11):e0164769.
Bjorvatn B, Grønli J, Pallesen S. Prevalence of different parasomnias in the general population. Sleep Med. 2010;11(10):1031–4.
Howell MJ. Parasomnias: an updated review. Neurotherapeutics. 2012;9(4):753–75.
Ekambaram V, Maski K. Non-rapid eye movement arousal parasomnias in children. Pediatr Ann. 2017;46(9):e327–31.
• Lopez R, Shen Y, Chenini S, Rassu AL, Evangelista E, Barateau L, et al. Diagnostic criteria for disorders of arousal: a video-polysomnographic assessment. Ann Neurol. 2018;83(2):341–51 A study exploring potential PSG markers for parasomnias.
Funding
This study was supported in part by the National Institutes of Neurological Disorders and Stroke (Grant K23 5K23NS104267-2 to Dr. Maski).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Maski reports grants from Jazz Pharmaceuticals and consulting honorarium from Harmony Biosciences, Uptodate, and Medscape outside the submitted work. Jazz Pharmaceuticals and Harmony Biosciences make drugs for narcolepsy and the article covers updates in narcolepsy treatments.
Dr. August has nothing to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Sleep and Sleep Apnea at the Extremes
Rights and permissions
About this article
Cite this article
August, J., Maski, K. Updates on Pediatric Sleep Disorders. Curr Sleep Medicine Rep 6, 163–175 (2020). https://doi.org/10.1007/s40675-020-00184-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40675-020-00184-w