Abstract
Purpose of Review
We reviewed and discussed studies on the role of oropharyngeal exercises in the treatment of children with obstructive sleep-disordered breathing (SDB).
Recent Findings
There has been increasing recent evidence on the role of oropharyngeal exercises in the stepwise therapeutic approach in children with SDB.
An oropharyngeal evaluation, targeted to explore the presence of orofacial muscle hypotonia, should be part in the assessment of children with SDB, in order to recognize potential oropharyngeal characteristics to be treated.
Summary
Current literature demonstrates that oropharyngeal exercises help to treat oropharyngeal muscle dysfunction that persists following the standard treatment of SDB, and improve symptoms and polysomnographic sleep variables SDB related in pediatric population.
New studies to compare different oropharyngeal exercise programs and to evaluate the long-term effects of this therapeutic approach could contribute to the indication of oropharyngeal exercises for the treatment of obstructive SDB in children.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Camacho M, Certal V, Abdullatif J, Zaghi S, Ruoff CM, Capasso R, et al. Myofunctional therapy to treat obstructive sleep apnea: a systematic review and meta-analysis. Sleep. 2015;38(5):669–75 First systematic review on myofunctional therapy reported data in the literature on the efficacy of myofunctional treatment as an adjunct to other obstructive sleep apnea treatments.
•• Guilleminault C, Huang YS, Mon teyrol PJ, Sato R, Quo S, Lin CH. Critical role of myofascial reeducation in pediatric sleep-disordered breathing. Sleep Med. 2013;14(6):518–25 The authors evaluated the impact of myofunctional reeducation in children with SDB referred for adenotonsillectomy, orthodontia, and myofunctional treatment in three different geographic areas.
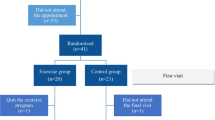
•• Villa MP, Brasili L, Ferretti A, Vitelli O, Rabasco J, Mazzotta AR, et al. Oropharyngeal exercises to reduce symptoms of OSA after AT. SleepBreath. 2015;19(1):281–9 The authors evaluated the efficacy of oropharyngeal exercises in children with symptoms of obstructive sleep apnea syndrome (OSA) after adenotonsillectomy.
Katz ES, D’Ambrosio CM. Pathophysiology of pediatric obstructive sleep apnea. Proc Am ThoracSoc. 2008;5:253–62.
•• Kaditis AG, Alonso Alvarez ML, Boudewyns A, Alexopoulos EI, Ersu R, Joosten K, et al. Obstructive sleep disordered breathing in 2- to 18-year-old children: diagnosis and management. Eur Respir J. 2016;47(1):69–94 This document summarizes the conclusions of a European Respiratory Society Task Force on the diagnosis and management of obstructive sleep-disordered breathing (SDB) in childhood and considered the myofunctional therapy as an adjunct to other obstructive sleep apnea treatments.
Marcus CL, Brooks LJ, Draper KA, Gozal D, Halbower AC, Jones J, et al. Clinical practice guideline. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130(3):576–84.
Kheirandish-Gozal L, Bhattacharjee R, Gozal D. Autonomic alterations and endothelial dysfunction in pediatric obstructive sleep apnea. SleepMed. 2010;11(7):714–20.
Chang SJ, Chae KY. Obstructive sleep apnea syndrome in children: epidemiology, pathophysiology, diagnosis and sequelae. Korean J Pediatr. 2010;53(10):863–71.
Villa MP, Castaldo R, Miano S, Paolino MC, Vitelli O, Tabarrini A, et al. Adenotonsillectomy and orthodontic therapy in pediatric obstructive sleep apnea. SleepBreath. 2014;18(3):533–9.
Kaditis A, Kheirandish-Gozal L, Gozal D. Algorithm for the diagnosis and treatment of pediatric OSA: a proposal of two pediatric sleep centers. Sleep Med. 2012;13(3):217–27.
Harvold EP, Tomer BS, Vargervik K, Chierici G. Primate experiments on oral respiration. Am J Orthod. 1981;79:359–72.
Miller AJ, Vargervik K, Chierici G. Experimentally induced neuromuscular changes during and after nasal airway obstruction. Am J Orthod. 1984;85:385–92.
Vargervik K, Miller AJ, Chierici G, Harvold E, Tomer BS. Morphologic response to changes in neuromuscular patterns experimentally induced by altered modes of respiration. Am J Orthod. 1984;85:115–24.
Huang YS, Guilleminault C. Pediatric obstructive sleep apnea and the critical role of oral-facial growth: evidences. Front Neurol. 2013;3:184.
•• de Felício CM, da Silva Dias FV, Trawitzki LVV. Obstructive sleep apnea: focus on myofunctional therapy. Nat Sci Sleep. 2018;10:271–286. eCollection 2018. Review. This review summarized and discussed the effects of OMT on OSA, the therapeutic programs employed, and their possible mechanisms of action.
Šujanská A, Ďurdík P, Rabasco J, Vitelli O, Pietropaoli N, Villa MP. Surgical and non-surgical therapy of obstructive sleep apnea syndrome in children. Acta Med (Hradec Kralove). 2014;57(4):135–41.
Camacho M, Guilleminault C, Wei JM, Song SA, Noller MW, Reckley LK, et al. Oropharyngeal and tongue exercises (myofunctional therapy) for snoring: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2018;275(4):849–55. https://doi.org/10.1007/s00405-017-4848-5 Review.
Huang YS, Guilleminault C. Pediatric obstructive sleep apnea: where do we stand? Adv Otorhinolaryngol. 2017;80:136–44. https://doi.org/10.1159/000470885 Review.
•• Villa MP, Evangelisti M, Martella S, Barreto M, Del Pozzo M. Can myofunctional therapy increase tongue tone and reduce symptoms in children with sleep-disordered breathing? Sleep Breath. 2017;21(4):1025–32. https://doi.org/10.1007/s11325-017-1489-2 The authors demonstrated that oropharyngeal exercises appear to effectively modify tongue tone, reduce SDB symptoms and oral breathing, and increase oxygen saturation, and may thus play a role in the treatment of SDB.
de Felício CM, da Silva Dias FV, Folha GA, de Almeida LA, de Souza JF, Anselmo-Lima WT, et al. Orofacial motor functions in pediatric obstructive sleep apnea and implications for myofunctional therapy. Int J Pediatr Otorhinolaryngol. 2016 Nov;90:5–11.
Chuang LC, Lian YC, Hervy-Auboiron M, Guilleminault C, Huang YS. Passive myofunctional therapy applied on children with obstructive sleep apnea: a 6-month follow-up. J Formos Med Assoc. 2017 Jul;116(7):536–41.
•• Lee SY, Guilleminault C, Chiu HY, Sullivan SS. Mouth breathing, "nasal disuse," and pediatric sleep-disordered breathing. Sleep Breath. 2015;19(4):1257–64 The authors assessed the presence of mouth breathing during sleep post-T&A in children with residual OSA. Persistence of mouth breathing post-T&A plays a role in progressive worsening through an increase of upper airway resistance during sleep with secondary impact on orofacial growth.
•• Cheng SY, Kwong SHW, Pang WM, Wan LY. Effects of an oral-pharyngeal motor training programme on children with obstructive sleep apnea syndrome in Hong Kong: a retrospective pilot study. Hong Kong J Occup Ther. 2017;30(1):1–5 The findings of this study support the role of occupational therapist in oromotor training modalities to improve the respiratory function for children with OSAS.
Bhattacharjee R, Kheirandish-Gozal L, Spruyt K, Mitchell RB, Promchiarak J, Simakajornboon N, et al. Adenotonsillectomy outcomes in treatment of obstructive sleep apnea in children: a multicenter retrospective study. Am J Respir Crit Care Med. 2010;182(5):676–83.
Ye J, Liu H, Zhang GH, Li P, Yang QT, Liu X, et al. Outcome of adenotonsillectomy for obstructive sleep apnea syndrome in children. Ann Otol Rhinol Laryngol. 2010;19(8):506–13.
Guimarães KC, Drager LF, Genta PR, Marcondes BF. Lorenzi-FilhoG . Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2009;179(10):962–6.
Fonteles CS, de MirandaMota AC, Lima RA, Borges PC, da Silveira A. Conservative management of severe open bite and feeding difficulties in patient with Noonan syndrome. Cleft Palate Craniofac J. 2013;50(2):242–8.
Abeleira MT, Seoane-Romero JM, Outumuro M, Caamaño F, Suárez D, Carmona IT. A multidisciplinary approach to the treatment of oral manifestations associated with Beckwith-Wiedemann syndrome: a long-term case report. J Am Dent Assoc. 2011;142(12):1357–64.
Folha GA, Valera FC, de Felício CM. Validity and reliability of a protocol of orofacial myofunctional evaluation for patients with obstructive sleep apnea. Eur J Oral Sci. 2015;123:165–72.
Potter NL, Short R. Maximal tongue strength in typically developing children and adolescents. Dysphagia. 2009;24(4):391–7.
Rappai M, Collop N, Kemp S, deShazo R. The nose and sleep-disordered breathing: what we know and what we do not know. Chest. 2003;124(6):2309–23 Review.
Van Dyck C, Dekeyser A, Vantricht E, Manders E, Goeleven A, Fieuws S, et al. The effect of orofacial myofunctional treatment in children with anterior open bite and tongue dysfunction: a pilot study. Eur J Orthod. 2016;38(3):227–34.
Peat JH. A cephalometric study of tongue position. Am J Orthod. 1968;54:339–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Villa Maria Pia and Evangelisti Melania each declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Sleep and Otolaryngology
Rights and permissions
About this article
Cite this article
Villa, M.P., Evangelisti, M. Oropharyngeal Exercises for Treatment of Pediatric Obstructive Sleep-Disordered Breathing. Curr Sleep Medicine Rep 5, 33–40 (2019). https://doi.org/10.1007/s40675-019-00136-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40675-019-00136-z