Abstract
Introduction
South Africa urgently needs more doctors. We examined perceptions of patients and students to provide evidence for optimum student-patient ratios and substantiate solutions for this dilemma.
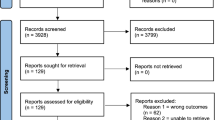
Methods
We interviewed 118 patients and invited 120 students to complete a self-administered questionnaire from four specialities in an academic hospital in Johannesburg.
Results
The total sample size was 238 participants. A total of 91/118 (77%) patients and 78/120 (65%) students were female. Almost all the patients had some level of education, with most patients having received at least a secondary education (71/120). More than half of the students (69/120) were final year students. A third (41/118) of the patients were unaware they were admitted to a teaching hospital. Half of the patients (60/118) thought they had the right to refuse interaction with students. Patients and students preferred smaller groups of between 1–3 and 4–8 students at a bedside tutorial (p < 0.001), although patients preferred smaller groups (1–3) compared with the students (4–8). Majority of patients said they never refused consent to students, while a third of students reported at least up to three patients refusing consent to be examined. The most frequent reason cited by students for refusal of consent by patients was the exposure to excessive numbers of students and healthcare professionals.
Conclusion
Medical schools should consider patient safeguards while responding to the country’s need for more doctors. The Medical Council and medical schools need to draw up professional guidelines on patient–student interactions, including the role of patients in this setting.
Similar content being viewed by others
References
Econex. Identifying the determinants of and solutions to the shortage of doctors in South Africa: is there a role for the private sector in medical education? [Internet]. 2015 [cited 2019 Jul 10]. Available from: http://www.mm3admin.co.za/documents/docmanager/f447b607-3c8f-4eb7-8da4-11bca747079f/00106942.pdf.
World Health Organization. World health statistics 2019: monitoring health for the SDGs, sustainable development goals. [Internet]. 2019 [cited 2019 Jul 10]. Available from: https://apps.who.int/iris/bitstream/handle/10665/324835/9789241565707-eng.pdf?ua = 1
Mahlathi P, Dlamini J. From brain drain to brain gain: understanding and managing the movement of medical doctors in the South African Health System [Internet]. WHO. 2017 [cited 2019 Jul 12]. p. 1–14. Available from: https://www.who.int/workforcealliance/brain-drain-brain-gain/17-304-south-africa-case-studies2017-09-26-justified.pdf?ua=1
Waterbury JT. Refuting patients’ obligations to clinical training: a critical analysis of the arguments for an obligation of patients to participate in the clinical education of medical students. Med Educ. 2001;35(3):286–94.
Lowe M, Kerridge I, Mcphee J, Hart C. Do patients have an obligation to participate in student teaching? Med Educ. 2008;42(3):237–41.
Khan M, Jawaid M, Hafeez K. Patients’ receptiveness for medical students during consultation in outpatient department of a teaching hospital. Pak J Medi Sci. 2013;29(2):454–7.
Onotai LO, Asuquo EO, Amadi E, Amadi-Oparelli A, Ali DU. Patients’ perception and attitude towards medical students’ involvement in patients care at a Nigerian University Teaching Hospital. Educ Res. 2012;3(9):732–43.
Sayed-Hassan R, Bashour H, Koudsi A. Patient attitudes towards medical students at Damascus University teaching hospitals. BMC Med Educ. 2012;12(1):13.
Awad A, Younis F. Patients’ attitude towards undergraduate medical students at university charity teaching hospital in Sudan. Int J Med. 2014;2(1):28–31.
HPCSA. Protecting the public and guiding the professions [Internet]. [cited 2019 Jul 6]. Available from: https://www.hpcsa.co.za/Committees/ETQA
Constitution of the Republic of South Africa [Internet]. 1996 [cited 2019 Jul 10]. p. 1–250. Available from: http://www.justice.gov.za/legislation/constitution/SAConstitution-web-eng.pdf
National Health Amendment Act. National Health Amendment Act 61 of 2003 [Internet]. Constitution of South Africa. 2013 [cited 2019 Jul 10]. p. 1–88. Available from: http://www.hpcsa.co.za/Uploads/editor/UserFiles/downloads/legislations/acts/nati_heal_act_61_2003.pdf
National Department of Health. The Patients’ Rights Charter Participation in decision-making [Internet]. 1996 [cited 2019 Jul 10]. Available from: http://www.justice.gov.za/VC/docs/policy/Patient Rights Charter.pdf
Niekerk M van Bioethics M, Law H, Dhai A, Bch MB, Sa F, et al. Is there a foundation in South African legislation to require students to disclose their academic status to patients when involved in their care ? 2014;7(1):9–13.
Marwan Y, Al-Saddique M, Hassan A, Karim J, Al-Saleh M. Are medical students accepted by patients in teaching hospitals? Med Educ Online. 2012;17(1).
Bashour H, Sayed-Hassan R, Koudsi A. Involving patients in medical education: ethical issues experienced by Syrian patients. Educ Health (Abingdon). 2012;25(2):87–91.
Goerl K, Ofei-Dodoo S. Patient perception of medical learners and medical education during clinical consultation at a family medicine residency. Kansas J Med. 2018;11(4):102–5.
Salah AB, El Mhamdi S, Bouanene I, Sriha A, Soltani M. Patients’ attitude towards bedside teaching in Tunisia. Int J Med Educ. 2015;6:201–7.
Bagg W, Adams J, Anderson L, Malpas P, Thorn M, Tulloch D, et al. Medical Students and informed consent. NZMJ. 2015;128(1414):27–35.
General Medical Council and Medical Schools Council. Achieving good medical practice: guidance for medical students [Internet]. 2016. Available from: https://www.gmc-uk.org/-/media/documents/Achieving_good_medical_practice_0816.pdf_66086678.pdf
Irish Medical Council. Guidelines for Medical Schools on Ethical Standards and Behaviour appropriate for Medical Students [Internet]. [cited 2019 Jul 14]. Available from: https://www.medicalcouncil.ie/Education/Career-Stage-Undergraduate/Guidelines-for-Medical-Schools-on-Ethical-Standards-and-Behaviour-appropriate-for-Medical-Students.pdf
HPCSA. Guidelines for Good Practice in the Healthcare Professions -Seeking Patients’ Informed Consent: the Ethical Considerations [Internet]. 2016 [cited 2019 Jul 30]. Available from: https://www.hpcsa.co.za/Uploads/editor/UserFiles/downloads/ethical_rules/Booklet 4 Informed Consent September 2016.pdf
Acknowledgements
This study was conducted in fulfilment of the requirements of CNM’s MSc in Bioethics and Health Law with the University of the Witwatersrand, Johannesburg
Author information
Authors and Affiliations
Contributions
CNM conceived and designed the study. CNM and NT collected the data. CNM prepared the manuscript. DM and CD assisted with statistical analysis. CNM, DM, CD, and AD were responsible for critical revision of the final manuscript.
Corresponding author
Ethics declarations
Approval to conduct the study was received from the University of the Witwatersrand Human Research Ethics Committee (M1704106). Permission was obtained from the Assistant Dean of Teaching and Student Support, the Heads of Departments of Internal Medicine, Surgery, Paediatrics, Obstetrics and Gynaecology and the office of the Chief Executive Officer at the Chris Hani Baragwanath Academic Hospital.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Menezes, C.N., Dhai, A., Tshabalala, N. et al. Perceptions of patients and medical students towards each other in the setting of patient care—a South African perspective. Med.Sci.Educ. 30, 933–942 (2020). https://doi.org/10.1007/s40670-020-00976-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-020-00976-3