Abstract
Introduction
The prevalence of mental health disorders including anxiety and depression is increasing and is linked to hypertension in healthy individuals. However, the relationship of psychosocial patient-reported outcomes on blood pressure (BP) in primary proteinuric glomerulopathies is not well characterized. This study explored longitudinal relationships between psychosocial patient-reported outcomes and BP status among individuals with proteinuric glomerulopathies.
Methods
An observational cohort study was performed using data from 745 adults and children enrolled in the Nephrotic Syndrome Study Network (NEPTUNE). General Estimating Equations for linear regression and binary logistic analysis for odds ratios were performed to analyze relationships between the exposures, longitudinal Patient-Reported Outcome Measurement Information System (PROMIS) measures and BP and hypertension status as outcomes.
Results
In adults, more anxiety was longitudinally associated with higher systolic and hypertensive BP. In children, fatigue was longitudinally associated with increased odds of hypertensive BP regardless of the PROMIS report method. More stress, anxiety, and depression were longitudinally associated with higher systolic BP index, higher diastolic BP index, and increased odds of hypertensive BP index in children with parent-proxy patient-reported outcomes.
Discussion/conclusion
Chronically poor psychosocial patient-reported outcomes may be significantly associated with higher BP and hypertension in adults and children with primary proteinuric glomerulopathies. This interaction appears strong in children but should be interpreted with caution, as multiple confounders related to glomerular disease may influence both mental health and BP independently. That said, access to mental health resources may help control BP, and proper disease and BP management may improve overall mental health.
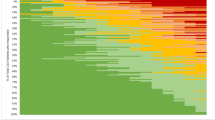
Graphical abstract


Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
Bitsko RH, Claussen AH, Lichstein J et al (2022) Mental Health Surveillance among children—United States, 2013–2019. MMWR Suppl 71(2):1–42. https://doi.org/10.15585/mmwr.su7102a1
Auerbach RP, Mortier P, Bruffaerts R et al (2018) WHO World Mental Health Surveys International College Student Project: prevalence and distribution of mental disorders. J Abnorm Psychol 127(7):623–638. https://doi.org/10.1037/abn0000362
Villarroel MA, Terlizzi EP (2020) Symptoms of depression among adults: United States, 2019. NCHS Data Brief. no. 379
Perou R, Bitsko RH, Blumberg SJ et al (2013) Mental health surveillance among children—United States, 2005–2011. MMWR Supplements 62(2):1–35
Cobham VE, Hickling A, Kimball H et al (2020) Systematic review: anxiety in children and adolescents with chronic medical conditions. J Am Acad Child Adolesc Psychiatry 59(5):595–618. https://doi.org/10.1016/j.jaac.2019.10.010
Katon WJ (2011) Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin Neurosci 13(1):7–23. https://doi.org/10.31887/DCNS.2011.13.1/wkaton
Shirazian S (2019) Depression in CKD: understanding the mechanisms of disease. Kidney Int Rep 4(2):189–190. https://doi.org/10.1016/j.ekir.2018.11.013
Libóro AB, Santos JP, Minete NF et al (2012) Proteinuria is associated with quality of life and depression in adults with primary glomerulopathy and preserved renal function. PLoS One 7(5):e37763. https://doi.org/10.1371/journal.pone.0037763
Troost JP, Waldo A, Carlozzi NE et al (2020) The longitudinal relationship between patient-reported outcomes and clinical characteristics among patients with focal segmental glomerulosclerosis in the Nephrotic Syndrome Study Network. Clin Kidney J 13(4):597–606. https://doi.org/10.1093/ckj/sfz092
Ohrnberger J, Fichera E, Sutton M et al (2017) The relationship between physical and mental health: a mediation analysis. Soc Sci Med 195:42–49. https://doi.org/10.1016/j.socscimed.2017.11.008
Luo MS, Chui EWT, Li LW (2020) The longitudinal associations between physical health and mental health among older adults. Aging Ment Health 24(12):1990–1998. https://doi.org/10.1080/13607863.2019.1655706
Yin S, Njai R, Barker L et al (2016) Summarizing health-related quality of life (HRQOL): development and testing of a one-factor model. Popul Health Metr 14:22. https://doi.org/10.1186/s12963-016-0091-3
Selewski DT, Troost JP, Cummings D et al (2017) Responsiveness of the PROMIS® measures to changes in disease status among pediatric nephrotic syndrome patients: a Midwest pediatric nephrology consortium study. Health Qual Life Outcomes 15:166. https://doi.org/10.1186/s12955-017-0737-2
Murphy SL, Mahan JD, Troost JP et al (2020) Longitudinal changes in health-related quality of life in primary glomerular disease: results from the CureGN study. Kidney Int Rep 5(10):1679–1689. https://doi.org/10.1016/j.ekir.2020.06.041
Canetta PA, Troost JP, Mahoney S (2019) Health-related quality of life in glomerular disease. Kidney Int 95(5):1209–1224. https://doi.org/10.1016/j.kint.2018.12.018
Krissberg JR, Helmuth ME, Almaani S et al (2021) Racial-ethnic differences in health-related quality of life among adults and children with glomerular disease. Glomerular Dis 1(3):105–117. https://doi.org/10.1159/000516832
Gadegbeku CA, Gipson DS, Holzman L et al (2013) Design of the Nephrotic Syndrome Study Network (NEPTUNE) to evaluate primary glomerular nephropathy by a multidisciplinary approach. Kidney Int 83(4):749–756. https://doi.org/10.1038/ki.2012.428
Cella D, Yount S, Rothrock NE et al (2007) The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Med Care 45(5 Suppl 1):S3–S11. https://doi.org/10.1097/01.mlr.0000258615.42478.55
Varni JW, Thissen D, Stucky BD et al (2014) PROMIS® Parent Proxy Report Scales for children ages 5–7 years: an item response theory analysis of differential item functioning across age groups. Qual Life Res 23(1):349–361. https://doi.org/10.1007/s11136-013-0439-0
Birnie KA, Richardson PA, Rajagopalan AV, Bhandari RP (2020) Factors related to agreement between child and caregiver report of child functioning with chronic pain: PROMIS pediatric and parent Proxy report. Clin J Pain 36(3):203–212. https://doi.org/10.1097/AJP.0000000000000794
Rothrock NE, Amtmann D, Cook KF (2020) Development and validation of an interpretive guide for PROMIS scores. J Patient Rep Outcomes 4(1):16. https://doi.org/10.1186/s41687-020-0181-7
Flynn JT, Kaelber DC, Baker-Smith CM et al (2017) Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 140(3)
Whelton PK, Carey RM, Aronow WS et al (2018) ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 71(6):1269–1324. https://doi.org/10.1161/HYP.0000000000000066
Hales CM, Carroll MD, Fryar CD, Ogden CL (2017) Prevalence of obesity among adults and youth: United States, 2015–2016. NCHS Data Brief 288:1–8
Weir CB, Jan A (2021) BMI classification percentile and cut off points. StatPearls, 2021. Accessed July 6, 2022. https://pubmed.ncbi.nlm.nih.gov/31082114/
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006
Schwartz GJ, Muñoz A, Schneider MF et al (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20(3):629–637. https://doi.org/10.1681/ASN.2008030287
Pierce CB, Muñoz A, Ng DK et al (2021) Age- and sex-dependent clinical equations to estimate glomerular filtration rates in children and young adults with chronic kidney disease. Kidney Int 99(4):948–956. https://doi.org/10.1016/j.kint.2020.10.047
Cohen BE, Edmondson D, Kronish IM (2015) State of the art review: depression, stress, anxiety, and cardiovascular disease. Am J Hypertens 28(11):1295–1302. https://doi.org/10.1093/ajh/hpv047
Nicholson A, Kuper H, Hemingway H (2006) Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J 27(23):2763–2774. https://doi.org/10.1093/eurheartj/ehl338
Wiehe M, Fuchs S, Moreira L et al (2006) Absence of association between depression and hypertension: results of a prospectively designed population-based study. J Hum Hypertens 20:434–439. https://doi.org/10.1038/sj.jhh.1002017
Meyer CM, Armenian HK, Eaton WW, Ford DE (2004) Incident hypertension associated with depression in the Baltimore Epidemiologic Catchment area follow-up study. J Affect Disord 83:127–133. https://doi.org/10.1016/j.jad.2004.06.004
Rubio-Guerra AF, Rodriguez-Lopez L, Vargas-Ayala G et al (2013) Depression increases the risk for uncontrolled hypertension. Exp Clin Cardiol 18(1):10–12 (Winter)
Meng L, Chen D, Yang Y, Zheng Y, Hui R (2012) Depression increases the risk of hypertension incidence: a meta-analysis of prospective cohort studies. J Hypertens 30(5):842–851. https://doi.org/10.1097/HJH.0b013e32835080b7
Bussotti M, Sommaruga M (2018) Anxiety and depression in patients with pulmonary hypertension: impact and management challenges. Vasc Health Risk Manag 8(14):349–360. https://doi.org/10.2147/VHRM.S147173
Liu MY, Li N, Li WA, Khan H (2017) Association between psychosocial stress and hypertension: a systematic review and meta-analysis. Neurol Res 39(6):573–580. https://doi.org/10.1080/01616412.2017.1317904
Marsland AL, Walsh C, Lockwood K, John-Henderson NA (2017) The effects of acute psychological stress on circulating and stimulated inflammatory markers: a systematic review and meta-analysis. Brain Behav Immun 64:208–219. https://doi.org/10.1016/j.bbi.2017.01.011
Shimba A, Ikuta K (2020) Control of immunity by glucocorticoids in health and disease. Semin Immunopathol 42(6):669–680. https://doi.org/10.1007/s00281-020-00827-8
Gill JM, Saligan L, Woods S, Page G (2009) PTSD is associated with an excess of inflammatory immune activities. Perspect Psychiatr Care 45(4):262–277. https://doi.org/10.1111/j.1744-6163.2009.00229.x
Rodriguez-Miguelez P, Looney J, Blackburn M et al (2022) The link between childhood adversity and cardiovascular disease risk: role of cerebral and systemic vasculature. Function (Oxf) 3(4):zqac029. https://doi.org/10.1093/function/zqac029
Agita A, Alsagaff MT (2017) Inflammation, immunity, and hypertension. Acta Med Indones 49(2):158–165
Kaperonis AE, Liapis CD, Dimitroulis D, Papavassiliou VG (2006) Inflammation and Athersclerosis. Eur J Vasc Endovasc Surg 31(4):386–393. https://doi.org/10.1016/j.ejvs.2005.11.001
Kubzansky LD, Adler GK (2010) Aldosterone: a forgotten mediator of the relationship between psychological stress and heart disease. Neurosci Biobehav Rev 34(1):80–86. https://doi.org/10.1016/j.neubiorev.2009.07.005
Mennuni S, Rubattu S, Pierelli G et al (2004) Hypertension and kidneys: unraveling complex molecular mechanisms underlying hypertensive renal damage. J Hum Hypertens 28:74–79. https://doi.org/10.1038/jhh.2013.55
Shatat IF, Becton LJ, Woroniecki RP (2019) Hypertension in childhood nephrotic syndrome. Front Pediatr 7:287. https://doi.org/10.3389/fped.2019.00287
Haas ME, Aragam KG, Emdin CA et al (2018) Genetic association of albuminuria with cardiometabolic disease and blood pressure. Am J Hum Genet 103(4):461–473. https://doi.org/10.1016/j.ajhg.2018.08.004
Johnson HM (2019) Anxiety and hypertension: Is there a link? A literature review of the comorbidity relationship between anxiety and hypertension. Curr Hypertens Rep 21:66. https://doi.org/10.1007/s11906-019-0972-5
Pariante CM, Lightman SL (2008) The HPA axis in major depression: classical theories and new developments. Trends Neurosci 31(9):464–468. https://doi.org/10.1016/j.tins.2008.06.006
O’Donovan A, Slavich GM, Epel ES, Neylan TC (2013) Exaggerated neurobiological sensitivity to threat as a mechanism linking anxiety with increased risk for diseases of aging. Neurosci Biobehav Rev 37(1):96–108. https://doi.org/10.1016/j.neubiorev.2012.10.013
Hall JE, Mouton AJ, da Silvia AA et al (2021) Obesity, kidney dysfunction, and inflammation: interactions in hypertension. Cardiovasc Res 117(8):1859–1876. https://doi.org/10.1093/cvr/cvaa336
Lim LF, Solmi M, Cortese S (2021) Association between anxiety and hypertension in adults: a systematic review and meta-analysis. Neurosci Biobehav Rev 131:96–119. https://doi.org/10.1016/j.neubiorev.2021.08.031
Blackwell CK, Elliott AJ, Ganiban J et al (2019) General health and life satisfaction in children with chronic illness. Pediatrics 143(6):e20182988. https://doi.org/10.1542/peds.2018-2988
Alcantra J, Ohm J, Alcantra J (2017) Comparison of pediatric self reports and parent proxy reports utilizing PROMIS: results from a chiropractic practice-based research network. Complement Ther Clin Pract 29:48–52. https://doi.org/10.1016/j.ctcp.2017.08.003
Cox ED, Connolly JR, Palta M et al (2020) Reliability and validity of PROMIS® pediatric family relationships short form in children 8–17 years of age with chronic disease. Qual Life Res 29:91–199. https://doi.org/10.1007/s11136-019-02266-x
Freitag GF, Salem H, Conroy K et al (2023) The Patient-Reported Outcomes Measurement Information System (PROMIS) pediatric and parent-proxy short forms for anxiety: psychometric properties in the Kids FACE FEARS sample. J Anxiety Disord. https://doi.org/10.1016/j.janxdis.2023.102677
Silvers JA, McRae K, Gabrieli JD et al (2012) Age-related differences in emotional reactivity, regulation, and rejection sensitivity in adolescence. Emotion 12(6):1235–1247. https://doi.org/10.1037/a0028297
Crowell JA (2021) Development of emotion regulation in typically developing children. Child Adolesc Psychiatr Clin N Am 30(3):467–474. https://doi.org/10.1016/j.chc.2021.04.001
Deng X, Sang B, Ku Y et al (2019) Age-related differences in the late positive potential during emotion regulation between adolescents and adults. Sci Rep 9:5738. https://doi.org/10.1038/s41598-019-42139-4
McKlveen JM, Myers B, Herman JP (2015) The medial prefrontal cortex: coordinator of autonomic, neuroendocrine and behavioural responses to stress. J Neuroendocrinol 27(6):446–456. https://doi.org/10.1111/jne.12272
Diorio D, Viau V, Meaney MJ (1993) The role of the medial prefrontal cortex (cingulate gyrus) in the regulation of hypothalamic-pituitary-adrenal responses to stress. J Neurosci 13(9):3839–3847. https://doi.org/10.1523/JNEUROSCI.13-09-03839.1993
Schaeuble D, Packard AEB, McKlveen JM et al (2019) Prefrontal cortex regulates chronic stress-induced cardiovascular susceptibility. J Am Heart Assoc 8(24):e014451. https://doi.org/10.1161/JAHA.119.014451
Franklin SS, Thijs L, Hansen TW et al (2013) White-coat hypertension: new insights from recent studies. Hypertension 62(6):982–987. https://doi.org/10.1161/HYPERTENSIONAHA.113.01275
Gallibois CM, Jawa NA, Noone DG (2017) Hypertension in pediatric patients with chronic kidney disease: management challenges. Int J Nephrol Renovasc Dis 10(null):205–213. https://doi.org/10.2147/IJNRD.S100891
“PROMIS® Score Cut Points.” (2022) Health measures, transforming how health is measured. https://www.healthmeasures.net/score-and-interpret/interpret-scores/promis/promis-score-cut-points
Acknowledgements
We would like to express our deepest gratitude to all the patients and families who generously participated in this study. We would also like to extend our thanks to the members of the NEPTUNE consortium listed below: Members of the Nephrotic Syndrome Study Network (NEPTUNE). NEPTUNE Enrolling Centers: Atrium Health Levine Children’s Hospital, Charlotte, SC: S Massengill (Principal Investigator), L Lo (Study Coordinator); Cleveland Clinic, Cleveland, OH: K Dell (Co-investigator), J Sedor (Co-investigator), B Martin (Study Coordinator); Children’s Hospital, Los Angeles, CA: K Lemley (Principal Investigator), C Fajardo (Principal Investigator), S Sharma (Study Coordinator); Children’s Mercy Hospital, Kansas City, MO: T Srivastava (Principal Investigator), K Markus (Study Coordinator); Cohen Children’s Hospital, New Hyde Park, NY: C Sethna (Principal Investigator), S Vento (Study Coordinator); Columbia University, New York, NY: P Canetta (Principal Investigator), A Pradhan (Study Coordinator); Duke University Medical Center, Durham, NC: R Gbadegesin (Principal Investigator), O Olabisi (Co-investigator), M Smith (Study Coordinator); Emory University, Atlanta, GA: L Greenbaum (Principal Investigator), CS Wang (Co-investigator), E Yun (Study Coordinator); The Lundquist Institute, Torrence, CA: S Adler (Principal Investigator), J LaPage (Study Coordinator); John H Stroger Cook County Hospital, Chicago, IL: A Amarah (Principal Investigator), M Itteera (Study Coordinator); Johns Hopkins Medicine, Baltimore, MD: M Atkinson (Principal Investigator), M Williams (Study Coordinator); Mayo Clinic, Rochester, MN: F Fervenza (Principal Investigator), M Hogan (Co-investigator), J Lieske (Principal Investigator; Study Coordinator); Medical University of South Carolina, D Selewski (Principal Investigator), C Alston (Study Coordinator); Montefiore Medical Center, Bronx, NY: F Kaskel (Principal Investigator), M Ross (Principal Investigator), P Flynn (Study Coordinator); NIDDK Intramural, Bethesda MD: J Kopp (Principal Investigator); New York University Medical Center, New York, NY: L Malaga-Dieguez (Principal Investigator), O Zhdanova (Co-investigator), LJ Pehrson (Study Coordinator); The Ohio State University College of Medicine, Columbus, OH: S Almaani (Principal Investigator), L Roberts (Study Coordinator); Stanford University, Stanford, CA: R Lafayette (Principal Investigator), S Dave (Study Coordinator); Temple University, Philadelphia, PA: I Lee (Principal Investigator), Z Pfeffer (Study Coordinator); Texas Children’s Hospital at Baylor College of Medicine, Houston, TX: S Shah (Principal Investigator), A Deslandes (Study Coordinator); University Health Network Toronto: H Reich (Principal Investigator), M Hladunewich (Co-investigator), P Ling (Study Coordinator), M Romano (Study Coordinator); University of California at San Francisco, San Francisco, CA: P Brakeman (Principal Investigator); University of Colorado Anschutz Medical Campus, Aurora, CO: A Podoll (Principal Investigator), N Rogers (Study Coordinator); University of Kansas Medical Center, Kansas City, KS: E McCarthy (Principal Investigator), E Landry (Study Coordinator); University of Miami, Miami, FL: A Fornoni (Principal Investigator), C Bidot (Study Coordinator); University of Michigan, Ann Arbor, MI: M Kretzler (Principal Investigator), D Gipson (Principal Investigator), A Williams (Study Coordinator), M Stelzer (Study Coordinator); University of Minnesota, Minneapolis, MN: P Nachman (Principal Investigator), M Rheault (Co-investigator), V Rao (Study Coordinator); University of North Carolina, Chapel Hill, NC: V Derebail (Principal Investigator), K Gibson (Principal Investigator), A Froment (Study Coordinator), F Ochoa-Toro (Study Coordinator); University of Pennsylvania, Philadelphia, PA: L Holzman (Principal Investigator), K Meyers (Co-investigator), K Kallem (Study Coordinator), A Swenson (Study Coordinator); University of Texas San Antonio, San Antonio, TX: K Sharma (Principal Investigator); University of Texas Southwestern, Dallas, TX: K Sambandam (Principal Investigator), E Robles (Study Coordinator), M Turk (Study Coordinator); University of Washington, Seattle, WA: A Jefferson (Principal Investigator), S Hingorani (Co-investigator), K Tuttle (Co-investigator) (Providence Medical Research Center, Spokane, WA), L Manahan (Study Coordinator), E Pao (Study Coordinator), K Kuykendall K (Providence Medical Research Center, Spokane, WA); Wake Forest University Baptist Health, Winston-Salem, NC: JJ Lin (Principal Investigator) no coordinators identified; Washington University in St. Louis, St. Louis, MO: E Cody (Principal Investigator) no coordinators identified. Data Analysis and Coordinating Center: Matthias Kretzler (Principal Investigator), Laura Barisoni (Co-investigator), Crystal Gadegbeku (Co-investigator), Brenda Gillespie (Co-investigator), Lawrence Holzman (Co-investigator), Laura Mariani (Co-investigator), Zubin Modi (Co-investigator), Matthew G Sampson (Co-investigator), Eloise Salmon (Co-investigator), John Sedor (Co-investigator), Abigail Smith (Co-investigator), Howard Trachtman (Co-investigator), Jarcy Zee (Co-investigator), Gabrielle Alter, Hailey Desmond, Sean Eddy, Damian Fermin, Wenjun Ju, Maria Larkina, Shengqian Li, Shannon Li, Chrysta Lienczewski, Tina Mainieri, Rebecca Scherr, Johnathan Troost, Amanda Williams. Digital Pathology Committee: Carmen Avila-Casado (University Health Network, Toronto), Serena Bagnasco (Johns Hopkins University), Clarissa Cassol (Arakana), Lihong Bu (Mayo Clinic), Shelley Caltharp (Emory University), Dawit Demeke (University of Michigan), Brenda Gillespie (University of Michigan), Jared Hassler (Temple University), Leal Herlitz (Cleveland Clinic), Stephen Hewitt (National Cancer Institute), Jeff Hodgin (University of Michigan), Danni Holanda (Arkana), Neeraja Kambham (Stanford University), Kevin Lemley (Children’s Hospital of Los Angeles), Laura Mariani (University of Michigan), Nidia Messias (Washington University), Alexei Mikhailov (Wake Forest), Behzad Najafian (University of Washington), Matthew Palmer (University of Pennsylvania), Avi Rosenberg (Johns Hopkins University), Virginie Royal (University of Montreal), Barry Stokes (Columbia University), David Thomas (Duke University), Michifumi Yamashita (Cedar Sinai), Hong Yin (Emory University) Jarcy Zee (University of Pennsylvania), Yiqin Zuo (University of Miami), Co-Chairs: Laura Barisoni (Duke University) and Cynthia Nast (Cedar Sinai). Last Update: 17 May 2023.
Funding
The Nephrotic Syndrome Study Network (NEPTUNE) is part of the Rare Diseases Clinical Research Network (RDCRN), which is funded by the National Institutes of Health (NIH) and led by the National Center for Advancing Translational Sciences (NCATS) through its Division of Rare Diseases Research Innovation (DRDRI). NEPTUNE is funded under grant number U54DK083912 as a collaboration between NCATS and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Additional funding and/or programmatic support is provided by the University of Michigan, NephCure Kidney International and the Halpin Foundation. RDCRN consortia are supported by the RDCRN Data Management and Coordinating Center (DMCC), funded by NCATS and the National Institute of Neurological Disorders and Stroke (NINDS) under U2CTR002818. C. Sethna is supported by NIH/NHLBI 1R01HL162912-01A1 and NIH/NIDDK R01DK131091. K.R. Tuttle is supported by NIH research grants R01MD014712, U2CDK114886, UL1TR002319, U54DK083912, U01DK100846, OT2HL161847, UM1AI109568, CDC project number 75D301-21-P-12254. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
M.S. and C.B.S. conceptualized the overall research questions and designed the subanalysis of the NEPTUNE study. M.S. conducted the statistical analyses. Original draft preparation was performed by M.S. and C.B.S., and all authors (M.S., T.M.B, D.A.G., K.R.T., G.C-F., R.V.L., A.G-V., F.M.A., T.S., C.B.S.) contributed to editing and reviewing the manuscript. Overriding supervision: C.B.S.
Corresponding author
Ethics declarations
Conflicts of interest
A.G-V has no conflict of interest to report. C.Sethna was on an advisory board for Travere Therapeutics. K.R. Tuttle reports support from Eli Lilly; personal fees and other support from Boehringer Ingelheim; personal fees and other support from AstraZeneca; grants, personal fees and other support from Bayer AG; grants, personal fees and other support from Novo Nordisk; grants and other support from Goldfinch Bio; other support from Gilead; and grants from Travere outside the submitted work.
Ethical approval
The NEPTUNE study was approved by the Institutional Review Board (IRB) at each of the 29 participating sites. The NEPTUNE study protocol was reviewed and approved by University of Michigan Medical School (IRBMED), Approval Number HUM00158219.
Human and animal rights
All procedures were approved by the University of Michigan Institutional Review Board.
Informed consent
Written informed consent and/or assent was obtained from each participant and/or caregiver before joining the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schuchman, M., Brady, T.M., Glenn, D.A. et al. Association of mental health-related patient reported outcomes with blood pressure in adults and children with primary proteinuric glomerulopathies. J Nephrol (2024). https://doi.org/10.1007/s40620-024-01919-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40620-024-01919-6