Abstract
Background
To evaluate fluid balance, biomarkers of renal function and its relation to mortality in patients with acute kidney injury (AKI) diagnosed before, or within 24 h of intensive care unit admission.
Methods
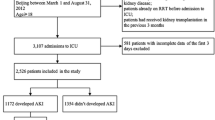
A prospective cohort study considered 773 critically ill patients observed over six years. Pre-intensive care unit-onset AKI was defined as AKI diagnosed before, or within 24 h of intensive care unit admission. Body weight-adjusted fluid balance and fluid balance-adjusted biomarkers of renal function were measured daily for the first three days of intensive care unit admission. Primary outcome was mortality in the intensive care unit.
Results
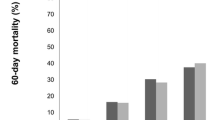
Prevalence of pre-intensive care unit-onset AKI was 55.1%, of which 55.6% of cases were hospital-acquired and 44.4% were community-acquired. Fluid balance was higher in AKI patients than in non-AKI patients (p < 0.001) and had a negative correlation with urine output (p < 0.01). Positive fluid balance and biomarkers of renal function were independently related to mortality. Multivariate analysis identified the following AKI-related variables associated with increased mortality: (1) In AKI patients: type 1 cardiorenal syndrome (OR 2.00), intra-abdominal hypertension (OR 1.71), AKI stage 3 (OR 2.15) and increase in AKI stage (OR 4.99); 2) In patients with community-acquired AKI: type 1 cardiorenal syndrome (OR 5.16), AKI stage 2 (OR 2.72), AKI stage 3 (OR 4.95) and renal replacement therapy (OR 3.05); and 3) In patients with hospital-acquired AKI: intra-abdominal hypertension (OR 2.31) and increase in AKI stage (OR 4.51).
Conclusions
In patients with pre-intensive care unit-onset AKI, positive fluid balance is associated with worse renal outcomes. Positive fluid balance and decline in biomarkers of renal function are related to increased mortality, thus in this subpopulation of critically ill patients, positive fluid balance is not recommended and renal function must be closely monitored.
Graphical abstract



Similar content being viewed by others
Availability of data, material and code
All data generated or analyzed during this study are included in this published article and its supplementary information files.
References
Koeze J, Keus F, Dieperink W, van der Horst IC, Zijlstra JG, van Meurs M (2017) Incidence, timing and outcome of AKI in critically ill patients varies with the definition used and the addition of urine output criteria. BMC Nephrol 18:70. https://doi.org/10.1186/s12882-017-0487-8
Turgut F, Awad AS, Abdel-Rahman EM (2023) Acute kidney injury: medical causes and pathogenesis. J Clin Med 12:375. https://doi.org/10.3390/jcm12010375
Sohaney R, Yin H, Shahinian V, Saran R, Ríos Burrows N, Pavkov ME et al (2022) In-hospital and 1-Year mortality trends in a national cohort of us veterans with acute kidney injury. Clin J Am Soc Nephrol 17:184–193. https://doi.org/10.2215/CJN.01730221
Ozrazgat-Baslanti T, Loftus TJ, Ren Y, Adiyeke E, Miao S, Hashemighouchani H et al (2021) Association of persistent acute kidney injury and renal recovery with mortality in hospitalised patients. BMJ Health Care Inform 28:e100458. https://doi.org/10.1136/bmjhci-2021-100458
Mehta S, Chauhan K, Patel A, Patel S, Pinotti R, Nadkarni GN et al (2018) The prognostic importance of duration of AKI: a systematic review and meta-analysis. BMC Nephrol 19:91. https://doi.org/10.1186/s12882-018-0876-7
Mayer KP, Ortiz-Soriano VM, Kalantar A, Lambert J, Morris PE et al (2022) Acute kidney injury contributes to worse physical and quality of life outcomes in survivors of critical illness. BMC Nephrol 23:137. https://doi.org/10.1186/s12882-022-02749-z
Messmer AS, Zingg C, Müller M, Gerber JL, Schefold JC, Pfortmueller CA (2020) Fluid overload and mortality in adult critical care patients-a systematic review and meta-analysis of observational studies. Crit Care Med 48:1862–1870. https://doi.org/10.1097/CCM.0000000000004617
Salahuddin N, Sammani M, Hamdan A, Joseph M, Al-Nemary Y, Alquaiz R et al (2017) Fluid overload is an independent risk factor for acute kidney injury in critically Ill patients: results of a cohort study. BMC Nephrol 18:45. https://doi.org/10.1186/s12882-017-0460-6
Perner A, Prowle J, Joannidis M, Young P, Hjortrup PB, Pettilä V (2017) Fluid management in acute kidney injury. Intensive Care Med 43:807–815. https://doi.org/10.1007/s00134-017-4817-x
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP et al (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 4:e296. https://doi.org/10.1371/journal.pmed.0040296
National Kidney Foundation (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2(Suppl 1):S19–S36. https://doi.org/10.1038/kisup.2012.1
Chávez-Íñiguez JS, Cano-Cervantes JH, Maggiani-Aguilera P, Lavelle-Góngora N, Marcial-Meza J, Camacho-Murillo EP et al (2021) Mortality and evolution between community and hospital-acquired COVID-AKI. PLoS One 16(11):e0257619. https://doi.org/10.1371/journal.pone.0257619
Lu JY, Babatsikos I, Fisher MC, Hou W, Duong TQ (2021) Longitudinal clinical profiles of hospital vs community-acquired acute kidney injury in COVID-19. Front Med 8:647023. https://doi.org/10.3389/fmed.2021.647023
Jiang L, Zhu Y, Luo X, Wen Y, Du B, Wang M et al (2019) Epidemiology of acute kidney injury in intensive care units in Beijing: the multicenter BAKIT study. BMC Nephrol 20:468. https://doi.org/10.1186/s12882-019-1660-z
Bendall AC, See EJ, Toussaint ND, Fazio T, Tan SJ (2022) Community-acquired versus hospital-acquired acute kidney injury at a large Australian metropolitan quaternary referral centre: incidence, associations and outcomes. Intern Med J. https://doi.org/10.1111/imj.15787
Neyra JA, Li X, Canepa-Escaro F, Adams-Huet B, Toto RD, Yee J et al (2016) Cumulative fluid balance and mortality in septic patients with or without acute kidney injury and chronic kidney disease. Crit Care Med 44:1891–1900. https://doi.org/10.1097/CCM.0000000000001835
Zhang Y, Zhang X, Xi X, Dong W, Zhao Z, Chen S (2022) Development and validation of AKI prediction model in postoperative critically ill patients: a multicenter cohort study. Am J Transl Res 14:5883–5895
Bourdeaux C, Ghosh E, Atallah L, Palanisamy K, Patel P, Thomas M et al (2020) Impact of a computerized decision support tool deployed in two intensive care units on acute kidney injury progression and guideline compliance: a prospective observational study. Crit Care 24:656. https://doi.org/10.1186/s13054-020-03343-1
Wang N, Jiang L, Zhu B, Wen Y, Xi XM (2015) The Beijing Acute Kidney Injury Trial (BAKIT) Workgroup. Fluid balance and mortality in critically ill patients with acute kidney injury: a multicenter prospective epidemiological study. Crit Care 19:371. https://doi.org/10.1186/s13054-015-1085-4
Patil VP, Salunke BG (2020) Fluid overload and acute kidney injury. Indian J Crit Care Med 24(Suppl 3):S94–S97. https://doi.org/10.5005/jp-journals-10071-23401
Wald R, Kirkham B, daCosta BR, Ghamarian E, Adhikari NKJ, Beaubien-Souligny W et al (2022) Fluid balance and renal replacement therapy initiation strategy: a secondary analysis of the STARRT-AKI trial. Crit Care 26:360. https://doi.org/10.1186/s13054-022-04229-0
Vaara ST, Ostermann M, Bitker L, Schneider A, Poli E, Hoste E et al (2021) Restrictive fluid management versus usual care in acute kidney injury (REVERSE-AKI): a pilot randomized controlled feasibility trial. Intensive Care Med 47:665–673. https://doi.org/10.1007/s00134-021-06401-6ç
Vaara ST, Parviainen I, Pettilä V, Nisula S, Inkinen O, Uusaro A et al (2016) Association of oliguria with the development of acute kidney injury in the critically ill. Kidney Int 89:200–208. https://doi.org/10.1016/j.kint.2015.12.007
Klein SJ, Lehner GF, Forni LG, Joannidis M (2018) Oliguria in critically ill patients: a narrative review. J Nephrol 31:855–862. https://doi.org/10.1007/s40620-018-0539-6
Su W, Cao R, Zhang X, Guan Y (2020) Aquaporins in the kidney: physiology and pathophysiology. Am J Physiol Renal Physiol 318:F193–F203. https://doi.org/10.1152/ajprenal.00304.2019
Goldstein SL (2020) Urine output assessment in acute kidney injury: the cheapest and most impactful biomarker. Front Pediatr 7:565. https://doi.org/10.3389/fped.2019.00565
Inkinen N, Pettilä V, Valkonen M, Serlo M, Bäcklund M, Hästbacka J (2022) Non-interventional follow-up versus fluid bolus in RESPONSE to oliguria in hemodynamically stable critically ill patients: a randomized controlled pilot trial. Crit Care 26:401. https://doi.org/10.1186/s13054-022-04283-8
Zhang L, Xu F, Li S, Zheng X, Zheng S, Liu H et al (2021) Influence of fluid balance on the prognosis of patients with sepsis. BMC Anesthesiol 21:269. https://doi.org/10.1186/s12871-021-01489-1
van Mourik N, Geerts BF, Binnekade JM, Veelo DP, Bos LDJ, Wiersinga JW et al (2020) A higher fluid balance in the days after septic shock reversal is associated with increased mortality: an observational cohort study. Crit Care Expl 2:e0219. https://doi.org/10.1097/CCE.0000000000000219
van Mourik N, Metske HA, Hofstra JJ, Binnekade JM, Geerts BF, Schultz MJ et al (2019) Cumulative fluid balance predicts mortality and increases time on mechanical ventilation in ARDS patients: an observational cohort study. PLoS One 14:e0224563. https://doi.org/10.1371/journal.pone.0224563
Inokuchi R, Hara Y, Yasuda H, Itami N, Terada Y, Doi K (2017) Differences in characteristics and outcomes between community- and hospital-acquired acute kidney injury: a systematic review and meta-analysis. Clin Nephrol 88:167–182. https://doi.org/10.5414/CN109011
Thongprayoon C, Hansrivijit P, Kovvuru K, Kanduri SR, Torres-Ortiz A, Acharya P et al (2020) Diagnostics, risk factors, treatment and outcomes of acute kidney injury in a new paradigm. J Clin Med 9:1104. https://doi.org/10.3390/jcm9041104´
Funding
This study did not receive any financial support for the conduct of the research and/or preparation of the article.
Author information
Authors and Affiliations
Contributions
All authors attest that they meet the current International Committee of Medical Journal Editors (ICMJE) criteria for authorship. Conceptualization: FDM-B, DB-A, LG-M, VO-R; data curation: FDM-B, DB-A, LG-M, VO-R, RC. C-G, JCM-P, JI-C, ES-dlR; methodology: FDM-B, VO-R, ES-dlR, OC-G; formal analysis: FDM-B, ES-dlR, OC-G; writing–original draft: FDM-B, JCM-P; writing–review and editing: FDM-B, DB-A, LG-M, VO-R, RCC-G, JC M-P, JI-C, ES-dlR, OC-G.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Human and animal rights
The study was conducted in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was in accordance with the national and local ethical standards.
Ethics approval
The study protocol was reviewed by the Ethics Committee for Scientific Research of the “Hermanos Ameijeiras” Hospital, Cuba (Approval number 54/10–06-2016).
Informed consent and patient details
The authors declare that this report does not contain any personal information that could lead to the identification of the patients. Written informed consent was obtained from all included patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Martos-Benítez, F.D., Burgos-Aragüez, D., García-Mesa, L. et al. Fluid balance, biomarkers of renal function and mortality in critically ill patients with AKI diagnosed before, or within 24 h of intensive care unit admission: a prospective study. J Nephrol 37, 439–449 (2024). https://doi.org/10.1007/s40620-023-01829-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-023-01829-z